Cell: Can Patients with COVID-19 use hormone therapy?
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
Cell: Can Patients with COVID-19 use hormone therapy?
Cell: Can Patients with COVID-19 use hormone therapy? In conjunction with 21 hospitals, Li Hongliang’s team found the key points for whether patients with COVID-19 can use hormone therapy.
Corticosteroids have been used to treat inflammation and acute respiratory distress syndrome (ARDS) for more than half a century. However, whether corticosteroids are clinically effective for new coronavirus pneumonia (COVID-19) is still a heated debate The problem.
The results of many clinical trials published recently show that corticosteroids dexamethasone or hydrocortisone can reduce the risk of death in severely ill patients with new coronavirus disease, and therefore have a beneficial effect on severely ill patients with new coronavirus disease.
After systematically reviewing 7 randomized clinical trials of corticosteroids and standard therapies, the World Health Organization (WHO) released the latest guidelines for corticosteroids in the treatment of new coronavirus pneumonia. The guidelines recommend systemic corticosteroid therapy for severely ill patients with new coronavirus disease, while corticosteroid therapy is not recommended for non-critical patients.
However, the current problem is that there is no clear standard to define severely ill patients with new coronavirus disease, which makes it sometimes impossible to determine whether a patient should receive hormone therapy.
Considering that corticosteroid therapy can cause many side effects, it is particularly important and urgent to develop objective, practical and reliable clinical parameters to identify which patients with new coronavirus disease can benefit from hormone therapy.
On January 5, 2021, Cell Metabolism magazine published a research paper entitled: The neutrophil-to-lymphocyte ratio determines clinical efficacy of corticosteroid therapy in patients with COVID-19, published by Li Hongliang and other teams from Wuhan University in advance.
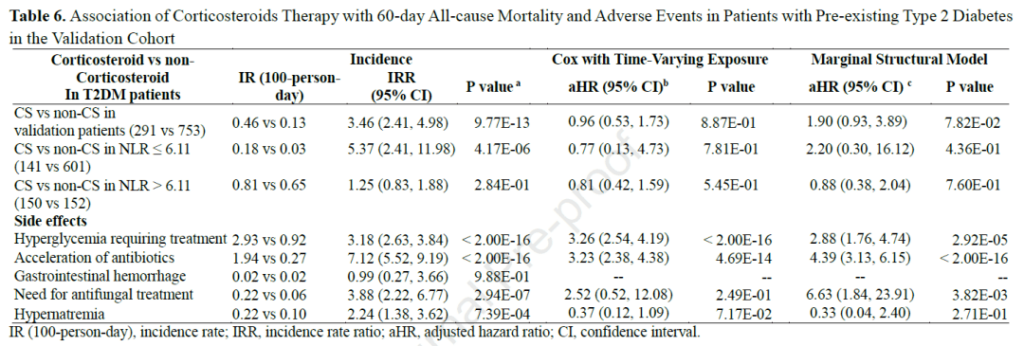
The research team analyzed 12862 COVID-19 cases in 21 hospitals in Hubei Province and found that patients with a neutrophil to lymphocyte ratio (NLR)> 6.11 at the time of admission have a higher mortality rate. More importantly, the use of corticosteroids in these patients can reduce the risk of all-cause mortality within 60 days.
On the contrary, for patients with NLR≤6.11 or with type 2 diabetes at the time of admission, corticosteroid therapy did not reduce their mortality, but hormone therapy increased the risk of hyperglycemia and infection.
These findings show that patients with neutrophil to lymphocyte ratio (NLR)> 6.11 when patients with new coronavirus disease are admitted to the hospital can reduce their risk of death by using corticosteroids, thereby allowing them to benefit from it. Therefore, neutrophils The ratio of cells to lymphocytes (NLR) can be used as a criterion for judging whether patients with new coronavirus disease need to receive hormone therapy.
Corticosteroids are currently almost the only drug that can definitely reduce the mortality of severely ill patients with new coronavirus disease. However, corticosteroid treatment can cause many side effects. Therefore, the FDA’s treatment guidelines do not recommend its use for non-critical patients. However, there is currently no clear standard that can distinguish severe patients from non-critical patients with new coronavirus disease.
In order to find an objective, practical and reliable clinical parameter to identify which COVID-19 patients can benefit from hormone therapy, the research team analyzed 12,862 COVID-19 cases in 21 hospitals in Hubei Province.
The results showed that patients with a neutrophil to lymphocyte ratio (NLR)> 6.11 at admission had a higher mortality rate. More importantly, the use of corticosteroids in these patients can reduce the risk of all-cause mortality within 60 days.
On the contrary, for patients with NLR≤6.11 or with type 2 diabetes at the time of admission, corticosteroid therapy did not reduce their mortality, but hormone therapy increased the risk of hyperglycemia and infection.
This shows that the neutrophil-to-lymphocyte ratio (NLR) at admission of patients with new coronavirus disease> 6.11, the use of corticosteroids can reduce their risk of death, thereby allowing them to benefit from it. Therefore, neutrophils and lymphocytes The ratio (NLR) can be used as a criterion for judging whether patients with COVID-19 need to receive hormone therapy.
The model diagram of the paper uses the form of comics to describe the research conclusion vividly:
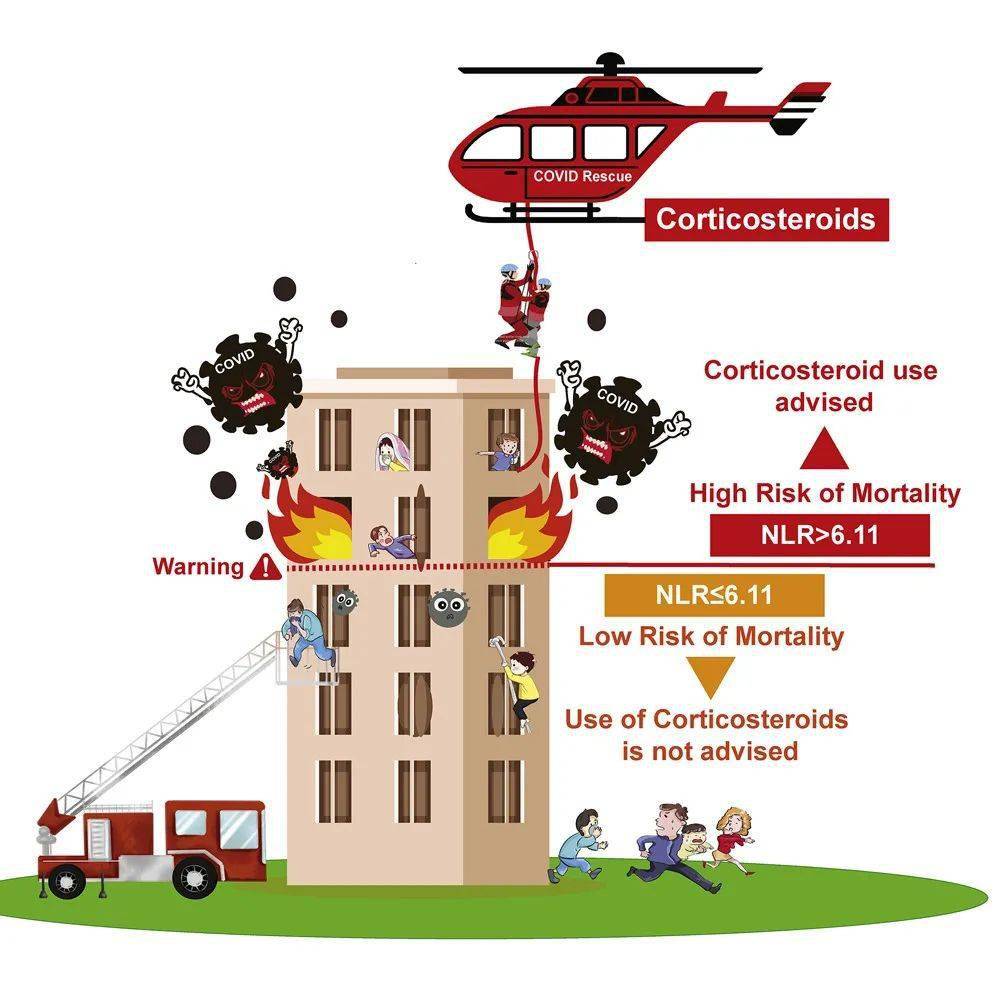
Infecting the COVID-19 is like a building on fire. When the patient’s neutrophil to lymphocyte ratio (NLR) is less than or equal to 6.11, the virus is still relatively mild in the body, and hormone therapy is not required, just like the one on the bottom of the building. People, facing a small fire, can use the fire ladder and climb down from the windows of the building.
When the ratio of neutrophils to lymphocytes (NLR) of the patient is greater than 6.11, the virus has already broken out in the body and hormone therapy is needed, just like the fire is already violent, and the passage downstairs is no longer possible. Can use helicopter for air rescue.
(sourceinternet, reference only)
Disclaimer of medicaltrend.org