TKA: First Total Knee Replacement Surgery
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
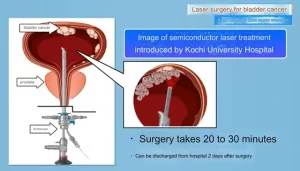
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
TKA: First Total Knee Replacement Surgery
TKA: First Total Knee Replacement Surgery. The medial parapatella approach is the most commonly used method of exposure for TKA. The most commonly used skin incision is the midline skin incision before the knee.
The conventional surgical approach for knee replacement is divided into the medial parapatella approach, the inferior medial femoral approach, the transmedial femoral approach, and the lateral parapatella approach according to the incision of the joint capsule. When the operation is difficult, especially in the case of knee ankylosis, in order to reveal enough to ensure the smooth progress of the operation, quadriceps femoris cut, quadriceps shaping, tibial tubercle osteotomy, etc. can be used to expand the exposure methods. The above methods have been explained in Chapter 5. This section provides further supplements for the most commonly used parapatellar approach in TKA surgery.
Conventional surgical approach
The medial parapatella approach is the most commonly used method of exposure for TKA. The most commonly used skin incision is the midline skin incision before the knee. It starts from about 7.5cm above the patella and goes down the midline of the knee to 1cm inside the tibial tubercle.
The joint capsule is cut on the inside of the parapatella, at the junction of the middle and inner 1/3 of the quadriceps tendon, from near to far, along the longitudinal axis to cut the quadriceps tendon to the vicinity of the patella stop of the medial femoral muscle. The inner edge of the patella extends downward along the inner edge of the patellar ligament to the inner and lower edge of the tibial tubercle 5-10mm (Figure 6-3-1).
The advantages of this approach are low difficulty, convenient incision extension, adequate exposure, and less vascular and nerve trauma. If extended to the full length, this operation can provide good exposure for the knee joint. As long as the length of the incision is appropriately extended, most knee joint operations can be completed through this incision.
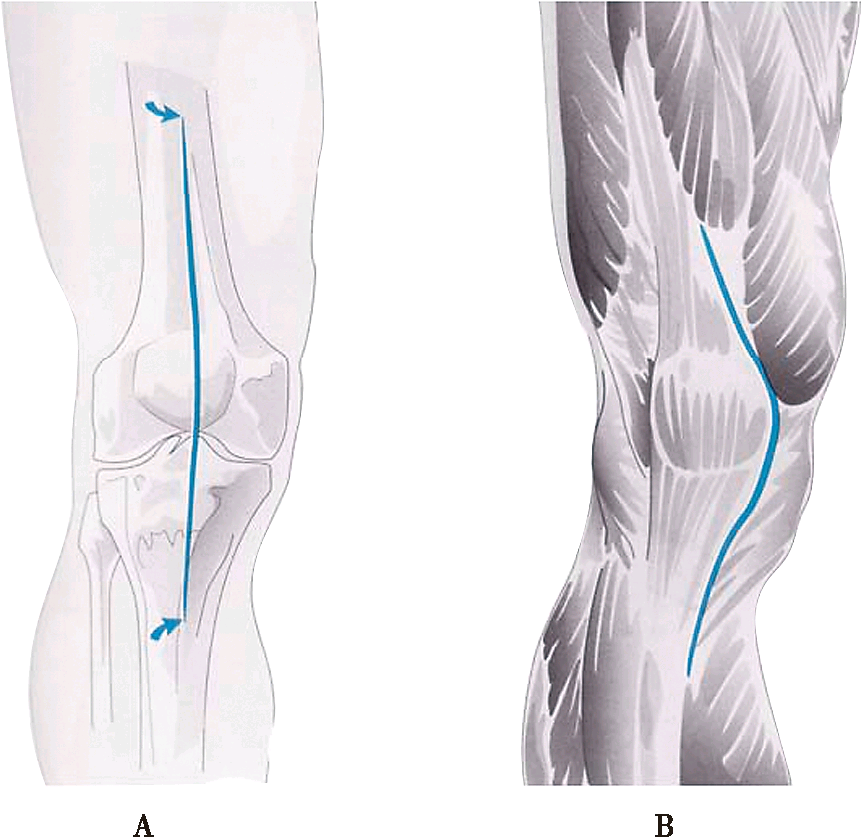
Figure 1 Medial parapatella approach: A surgical incision; B joint capsule incision
Standard exposure technique
After the joint capsule is cut, the osteotomy cannot be performed immediately. The upper and lower articular surfaces must be fully exposed before the osteotomy, and the flexion and extension of the soft tissues must meet the requirements to ensure the correct osteotomy and placement of the prosthesis.
1. First do the subperiosteal dissection of the medial proximal tibia. The subperiosteal dissection should start at the knee extension position and proceed gradually with the knee flexion process. Loosen the deep layer of MCL to near the stop point of the semimembranous muscle extension. Loosen the posterior medial joint capsule. Subperiosteal dissection is conducive to the high flexion of the knee joint and the external rotation of the tibia, making it easy for the tibia to protrude from below the femur, and it is also conducive to the outward movement of the patella and the femoral extension device;
2. Dissociate under the periosteum near the tibial tubercle of the patellar tendon to reduce the risk of patellar ligament avulsion;
3. Loosen the lateral patellofemoral ligament, which is conducive to patellar valgus;
4. Appropriate removal of the subpatellar fat pad can not only improve the mobility of the patella, but also reduce the formation of subpatellar scars after surgery;
5. When the outer edge of the patella is loosened, the main method is to cut off the joint capsule at the outer edge of the patella to increase the range of motion of the patella;
6. If the above method is still insufficient, you can extend the incision proximally to enlarge the exposure.
Revealing technique of tonic knee
When the patient has a rigid knee or a stiff knee, the risk of the patellar ligament being avulsed from the tibial tubercle during the exposure process is high. All of the above methods to increase the patellar mobility, such as medial semimembranosus bursectomy, subpatellar fat pad removal, and Lateral release of the patella and external rotation of the tibia are effective methods to prevent avulsion of the patellar ligament. In addition, supplementary methods such as exposing the lateral tibial plateau, removing scars, and stripping the joint capsule to Gerdy’s nodules are included to increase the movement space of the patella. These supplementary measures must avoid damaging the cochineal tendon and the lateral collateral ligament. In addition to external rotation of the tibia, it also helps to reverse the patella. When none of the above methods meet the exposure requirements, the following methods can be used to meet the exposure requirements.
(1) Rectus femoris cutting technique
On the basis of the traditional medial parapatella approach, simply place the proximal end of the incision obliquely toward the outer and upper rectus femoris muscle to cut off the rectus femoris tendon. The operation method is simple and easy to implement, while effectively improving the exposure of the stiff knee joint, it will not significantly increase the incidence of complications.
It will not damage the lateral superior knee artery, and will not affect postoperative rehabilitation and quadriceps function. Assess the difficulty of turning the patella and flexing the knee joint during the operation.
If the patella is difficult to flip through the conventional approach, which may cause avulsion of the tibial tubercle, extend the proximal end of the incision at 45° outward and upward, and cut off the rectus femoris near the rectus femoris tendon-abdominal joint to help the patella Flip down and out (Figure 6-3-2). If there is still difficulty, observe whether there is a thickened scar tissue that needs to be removed, or the external support of the patella is loose. For those who have difficulty, it is necessary to consider quadriceps V-Y shaping.
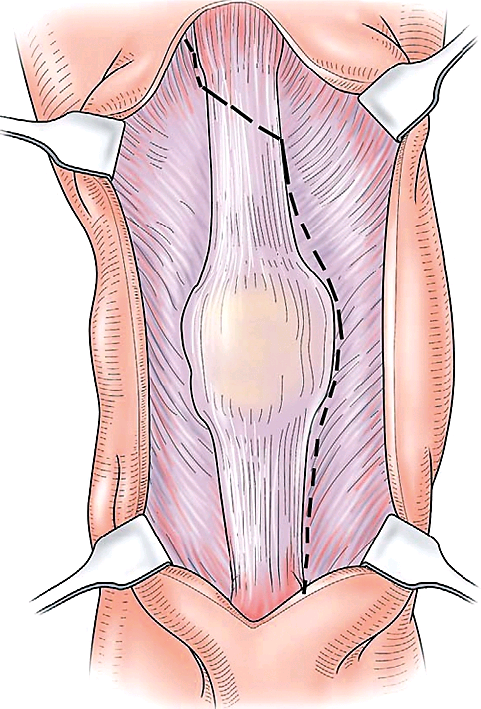
Figure 2 Quadriceps cut: incision method
(2) Tibial tuberosity osteotomy technique
Tibial tuberosity osteotomy also has the effect of extending the knee extension device, and does not damage the quadriceps, and the muscles will not leave scars, and have little effect on the function of the quadriceps. Moreover, the strength of bone-to-bone healing is more reliable. On the basis of the conventional medial parapatella approach, it extends down to 8-10cm away from the tibial tubercle. The osteotomy block includes the tibial tubercle with the patellar ligament intact and the tibial anterior cortex with the tibial crest at the distal end. The bone piece is about 6cm long and 2cm wide (not less than 1cm). Use a bone knife or electric saw to cut off the tibial tubercle and its distal bone block from the tibia, but maintain the complete connection of the soft tissue and periosteum on the outer edge of the bone block and preserve the blood supply. Fully expose the knee joint. The key to the success of the operation is that the cut bone block with tibial tuberosity must be large enough, the stem end of the tibial prosthesis must exceed the distal end of the osteotomy, and the periosteum of the outer edge of the osteotomy block must be intactly connected and firmly fixed. Because screws can cause local stress concentration in the bone graft, fractures are prone to occur. Therefore, for the re-fixation of the osteotomy block, the wire binding method is usually used (Figure 6-3-3).
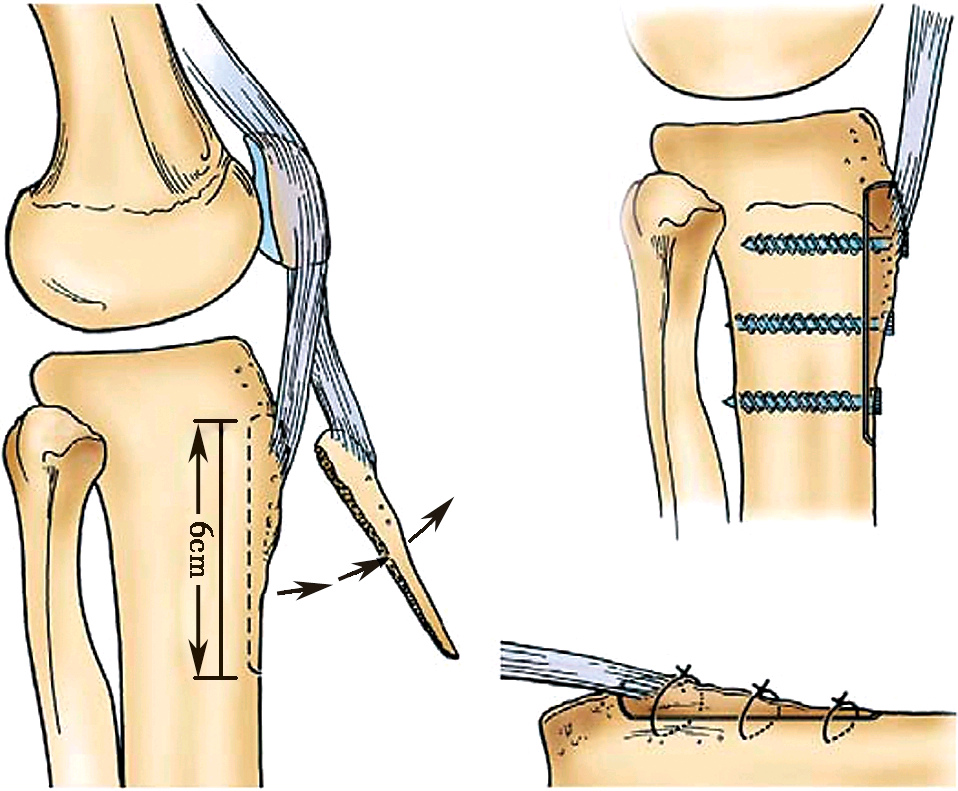
Figure 3 Tibial tuberosity osteotomy
Extensive subperiosteal dissection technique
It is very difficult to expose patients with knee ankylosis. In addition to quadriceps tendonotomy and tibial tubercle osteotomy, extensive subperiosteal stripping of the femur and tibia is also an alternative method. The specific method is as follows: First, perform subperiosteal dissection of the proximal medial end of the tibia to the middle section of the tibial shaft, and gradually flex and externally rotate the knee joint. Care must be taken to protect the attachment point on the femoral side of the MCL. If the medial subperiosteal dissection cannot sufficiently flex the knee joint, perform a subperiosteal dissection of the distal femur to ensure the integrity of the soft tissue sleeve, and carefully peel back to make the distal femur prolapse. The advantages of subperiosteal dissection of the distal femur and subperiosteal dissection of the proximal tibia are that important soft tissue structures are not damaged or torn during knee flexion, and the complete soft tissue sleeve can be reset and applied to the bone surface when the incision is closed. .
However, this extensive subperiosteal dissection technique may cause instability in and out of the joint. At this time, a highly restrictive prosthesis needs to be selected; in addition, extensive subperiosteal dissection may also cause avascular necrosis of the femoral condyle. Therefore, this technique can only be used when there are no other options.
(source:internet, reference only)
Disclaimer of medicaltrend.org