The resistance mechanism of CAR-T therapy
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
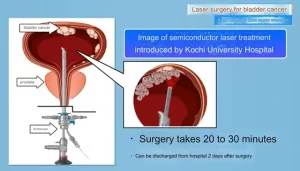
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
The resistance mechanism of CAR-T therapy
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- What is the difference between Atorvastatin and Rosuvastatin?
- How long can the patient live after heart stent surgery?
The resistance mechanism of CAR-T therapy. Chimeric antigen receptor (CAR) T-cell therapy has been successful in early clinical trials involving pre-B-cell acute lymphoblastic leukemia (ALL) or B-cell lymphoma, completely changing the anti-cancer therapy and providing patients with refractory standards Provides potential treatment options for treatment.
However, the CAR T cell persistence and/or cancer cell resistance is poor due to the loss or regulation of antigens, and many patients will have a short remission period. In addition, the initial experience of CAR T cells highlights the challenges associated with manufacturing patient-specific therapies.
In this article, we discussed factors that can rule out persistent remission after CAR T cell therapy, focusing on the drug resistance mechanism of disease recurrence. We also outline potential strategies for overcoming these obstacles in order to more effectively incorporate this unique treatment strategy into the standard treatment paradigm.
In April 2012, after the first successful CD19-directed chimeric antigen receptor (CAR) T cell therapy for adult follicular lymphoma or chronic lymphocytic leukemia (CLL) [1-3], the first Children with acute lymphoblastic leukemia (ALL) are injected with anti-CD19 CAR T cells [4,5]. The FDA approved 5 distinct anti-CD19 CAR T cell products [11-13] for the treatment of B-cell ALL and diffuse large B-cell lymphoma, and completely changed the field of anti-cancer immunotherapy.
As more and more patients receive treatment and obtain longer follow-up data, we realize that approximately 30-50% of patients have relapsed with anti-CD19 CAR T cells, most of which are within 1 year of treatment. Within [9,10]. Relapse is not unique to drugs that target CD19, because preliminary clinical experience with other CAR targets (such as CD22) shows that relapse will be a common and recurring challenge [15].
In addition, about 10-20% of patients fail to enter remission after receiving anti-CD19 CAR T cell therapy [7-10]. The loss or regulation of target antigen [15-17] and/or the persistent lack of CART cells [18], and the failure of product manufacturing [19,20] (Figure 1) are one of the most common obstacles to effective CAR T cell therapy. In addition, CAR T cells have not achieved similar success in diseases other than B-cell leukemia and lymphoma.
Understanding the limitations of CAR T cell therapy and overcoming these obstacles is essential to harness the full potential of this highly effective treatment method.

Figure 1 | Limitations of sustained remission after CAR T cell therapy. This figure summarizes several different limitations of achieving durable remission through chimeric antigen receptor (CAR) T cell therapy.
First of all, there are many reasons for CAR T cell failure: For some patients, CAR T cell products cannot be successfully produced, or the generated CAR T cells cannot be fully expanded (during in vitro production or after in vivo administration); in other patients Among them, the problem of limited persistence in the body is the underlying mechanism of disease recurrence.
Second, antigen regulation-characterized by the loss or down-regulation of CD19 and/or CD22 on malignant B cells-makes antigen escape a mechanism for resistance to CAR T cell therapy, which may also be a problem in non-B cell malignancies , Including solid tumors.
Third, the characteristic toxicity of CAR T cell therapy-mainly severe cytokine release syndrome (CRS) and/or neurotoxicity-can be fatal, thus eliminating the possibility of therapeutic benefit for a small number of patients.
In addition, data on the lasting impact of CRS treatment intervention on CAR remission are still unknown. Finally, unmet needs include certain disease backgrounds, which are the focus of ongoing research efforts to optimize the clinical utility of CAR T cell therapy.
For example, although anti-CD19 CAR T cells can provide substantial benefits to adults with lymphoma, their complete remission rate is lower than in leukemia patients. In addition, the results of CAR T cell therapy for pediatric lymphoma patients and central nervous system (CNS) patients are still an area of ongoing research.
It is worth noting that the curative effect of this therapy on patients with solid tumors is currently limited, and methods to optimize the response are being explored.
In this review, we summarized the knowledge about the rapid development of persistent CAR T cell-induced remission barriers.
We mainly discuss the mechanism of emerging resistance to CAR T cell therapy related to antigen escape. We also discuss antigen-positive recurrence related to poor CAR T cell persistence, and solve the problem of non-responsiveness or non-responsiveness related to product production.
Fully related limitations and toxicity. In addition, we will focus on actively researching potential strategies to overcome the limitations of CAR T cell therapies and new indications for these therapies.
Obstacle 1: Failure to achieve mitigation
The potential benefits of CAR T cells first require patients to obtain treatment, and successfully manufacture, infuse and effectively mediate cytotoxicity, thereby ideally leading to complete remission. This is the way to success for CAR T cell products. It is worth noting that these preconditions have been shown to be feasible for most ALL patients, although they still pose potential obstacles to effective CAR T cell therapy in some patients and therefore provide opportunities for improvement.
Product Manufacturing.
The first obstacle in the process of CAR T cell therapy is the collection of T cells for the production of CAR-expressing products. Unfortunately, data on the actual percentage of ALL patients who cannot obtain a sufficient number of T cells are limited, because patients are often excluded from consideration for CAR T cell therapy due to the pre-existing lymphopenia, which may be previous cells Caused by toxic therapy.
Even if T cells are successfully collected, for example, if the product fails to be manufactured, the patient may not receive treatment. It is worth noting that in a phase I study, the baseline absolute lymphocyte count (ALC) of pediatric patients treated with anti-CD19 CAR T cell therapy was analyzed [8], and the median ALC was 1,228 cells/μl (range 168– 4,488 cells/μl).
This finding indicates that the selection of patients is biased towards those with ALC patients within the normal physiological range, which may lead to the exclusion of patients who have received rigorous treatment or undergoing ongoing treatment. Although many centers’ research teams currently use minimal ALC or CD3+ cell counts for apheresis, improvements in CAR T cell production may reduce the limits of cell collection.
Our experience at the National Cancer Institute (NCI) shows that it is feasible to manufacture CAR T cell products with a cell count of CD3+≥150 cells/μl. In a clinical trial conducted by NCI, 55 of 56 patients successfully manufactured anti-CD22CAR T cell products.The median number of CD3+ cells in these patients was 567 cells/μl (range 145-2,144 cells/μl), and the median ALC was 775 cells/μl (range 230-4,620 cells/μl) (NNS and TJF unpublished observations) ).
The possibility of obtaining a sufficient number of T cells is undoubtedly an important consideration, and other data are needed in this field.
In addition to the number of cells, the characteristics of hematology products can also affect the ability to successfully manufacture CAR T cell products or the quality of the manufactured CAR T cell products. Previous treatments with chemotherapy (for example, chemotherapy containing clofarabine or doxorubicin) have been associated with the production of insufficient or poor quality CAR T cell products [7,21].
In addition, clinical data indicate that prior treatment with cyclophosphamide and cytarabine can selectively reduce the early lineage T cells associated with the expansion of productive CAR T cells [22]. The results published in the past 2 years indicate that the production of CAR T cell products from patients with high-risk solid tumors may be particularly challenging [19,21]. Collecting T cells early in patients who are determined to have a high risk of recurrence or before treating patients with recurrent disease may improve the quality of apheresis products and thus the CAR T cells produced.
Other details of the CAR T cell manufacturing process may also affect the quality of the resulting product, which in turn affects the subsequent clinical response. Current manufacturing protocols include a T cell expansion step usually induced by activation via T cell receptor (TCR) [25,26].
Anti-CD3 and anti-CD28 bead-based amplification and anti-CD3 antibody amplification protocols are used in the production of anti-CD19CAR T cell products approved by the FDA [27,28]. The expansion plan of CAR T cells usually also includes the use of cytokines, such as IL-2, IL-7 and/or IL-15; similarly, no method has clear advantages, but the different effects of these cytokines It may qualitatively affect the CAR T cell products obtained [29].
Almost all CAR T cell products are produced using CD4+ T cells and CD8+ T cells, and both of these cell populations may help improve efficacy. Although the difference in efficacy between products with different ratios has not been determined, the ratio of CD4+ to CD8+ T cells between patients may change substantially and may also affect CAR T cell products.
Based on preclinical data showing enhanced efficacy [30], in some trials, separate CD4+ and CD8+ CAR T cell products have been produced to deliver to patients in a determined ratio [8,31]. Repeated modifications to the manufacturing process have the potential to improve the effectiveness of CAR T cells, which may be of greater importance when testing CAR T cells beyond the ability of B cell malignancies.
New methods of CAR T cell manufacturing, such as the use of closed system automation equipment, combined with the above-mentioned foundation, have just begun to be implemented [32,33]. It is necessary to use these methods to conduct clinical trials and further analyze how these technologies will affect future CAR T cell therapies.
Even if CAR T cell products can be successfully manufactured, it has been proven that the initial T cell phenotype is an important determinant of subsequent clinical activities. Selecting T cells with a specific phenotype before manufacturing, such as central memory or stem cell-like memory T cells [22,34,35] or controlling manufacturing conditions to bias CAR T cell production toward specific T cell populations may improve the production of successful products Possibility [35].
Priority manufacturing methods involving these unique T cell populations are under development. In a study of CLL patients who received anti-CD19 CAR T cell products [36], it was found that the CAR T cell population of responders was rich in the expression of memory-related genes and had a higher expression capacity than non-responders.
A large number of CD27+ PD1-CD8+ CAR T cells express high levels of IL-6 receptors, thereby better controlling the tumor; this cell phenotype is more predictive of response than other diseases and patient characteristics [36].
Guidelines for the development of commercial CAR cell products have been formulated and may develop as our knowledge and experience increase [41,42].
CAR construct design is another parameter that may affect the characteristics of CAR T cell products and the subsequent in vivo behavior of modified cells (including their expansion kinetics and duration).
Most CAR T cell products tested in clinical trials are second-generation drugs, which means that they contain both a TCR stimulation domain (usually derived from the T cell surface glycoprotein CD3ζ chain (CD3ζ)) and a single stimulation domain. Products currently approved by the FDA contain CD28 or 4-1BB (also known as CD137) costimulatory domain. Although preclinical data [43] and patient observations [44,45] indicate that this aspect of CAR design significantly affects the durability of cell products.
Other details of CAR design, such as the specific characteristics of the antigen-binding domain, the presence and structure of the extracellular hinge region, and the characteristics of the transmembrane domain, may also affect CAR T cell properties.
An important issue in the field of CAR T cell research is to establish reliable standards to define the efficacy of CAR T cell products. At present, the standard parameters that define T cell efficacy (such as markers of T cell failure) are disappointing in predicting clinical efficacy [55,56]. In view of the high response rate of CAR T cell therapy in leukemia patients, the number of non-responders is small, so it is difficult to systematically evaluate and establish parameters related to lack of responsiveness-especially considering that the underlying causes may be many Factors and cannot be fully attributed to product variables.
However, in CLL patients, the response rate is much lower than that of ALL or lymphoma patients. Fraietta et al. [36] were able to identify favorable product characteristics, such as abundant IL-6–STAT3 markers and CD29+ before the formation of CAR T cells. The frequency of CD45RO-CD8+ T cells is increased.
In addition, compared with products with this multifunctional activity, pre-infusion anti-CD19 CAR T cell products containing a subset of multifunctional T cells have improved lymphoma compared to definitions based on cytokine and chemokine expression profiles Patient response. Establishing the ideal properties of CAR T cells will require additional data, but the optimal characteristics may vary depending on the CAR construct and the targeted malignancy.
Using cells from healthy donors to produce CAR T cell products is another strategy to solve the problem of poor CAR T cell quality. Several groups have now tested donor-based CAR-based treatment strategies using T cells directly derived from their original allogeneic stem cell donors in preclinical [58] and in patients whose disease has relapsed after transplantation [59-61 ]. The results of these early studies prove the feasibility of this method, only in the high frequency of high-grade graft-versus-host disease (GVHD) [59-61] low incidence.
Infusion of CAR T cells.
Obviously, failure to inject CAR T cell products in time before the patient develops disease or disease-related complications may also hinder successful treatment.
In the FDA-approved anti-CD19 CAR T-cell product tisagenlecleucel in a registered trial in children and young adults with ALL10, of 92 patients who had collected apheresis hemorrhage, 17 patients (18%) did not receive the rea These sons of CAR T cell infusions included product problems related to tesagilin in 7 patients (mainly due to poor cell growth), and 7 patients died before CAR T cell infusion (due to disease progression in 4 patients and other Infection-related complications) and the development of intermittent adverse reactions that make the patient unsuitable for CAR T cell infusion (fungal disease or GVHD).
In this study10, the median time for cell infusion was 45 days (range 30-105 days). With 20% to 30% of candidate patients unable to receive CAR T cell infusion, future strategies to reduce production time are expected to increase the likelihood of eligible patients to receive infusion, thereby increasing the number of patients benefiting from CAR T cell therapy The commercialization of spy CAR T-cell therapy and more readily available production plans are expected to reduce the delay in infusion time.
Activation and expansion of CAR T cells.
Clinical studies have shown that the dose of CAR T cells required for effective treatment is very small. The current dosage regimen is 0.2–5.0×106 transduced CAR T cells per kilogram or a total of 0.1–2.5×108 transduced CAR T cells per kilogram. Note, although cell activation and exponential expansion after infusion are essential [6-10,70,71].
As discussed, the quality of CAR T cell products and the inherent T cell phenotype can affect the behavior of CAR T cells after infusion. In addition, receptor-related factors are also important in the expansion of CAR T cells. For example, the burden of disease (and therefore antigen) can positively affect the degree of cell expansion, which in turn may increase the risk and severity of CRS [7,8].
Get CAR T cell therapy.
Although the FDA has approved the approval of CD19-directed CAR T cell products in the past two years [11,12], the access to these novel therapies is still limited.
In addition, cost and insurance coverage are persistent obstacles to expanding patients’ access to CAR T cell therapy [78-80]. With the development of this therapy, cost analysis and optimization of manufacturing strategies are required to reduce costs.
In addition, the eligibility criteria for receiving FDA-approved drugs can be viewed as restricting patient entry. For example, active central nervous system (CNS) involvement is still the exclusion criterion for patients with B-cell lymphoma. However, clinical trials to study the safety and effectiveness of CAR T cell therapy in this population and other populations are crucial, and the ultimate goal is to extend the therapeutic indications to all groups that may benefit.
Obstacle 2: Disease recurrence
Within 12 months after infusion, disease recurrence after anti-CD19 or anti-CD22 CAR T cell therapy may occur in up to 50% of B-cell ALL patients [8–10,15]. There are two main modes: early recurrence of antigen-positive leukocytes Or later recurrence is usually related to the loss of antigen (Figure 1). An in-depth understanding of the mechanisms of CAR T cell persistence and/or poor drug resistance and identifying patients with the highest likelihood of recurrence are essential for optimizing CAR T cell therapy.
Antigen-positive recurrence.
The early recurrence of ALL (usually within the first few months after successful induction of remission) is usually associated with limited CAR T cell persistence and/or transient B cell hypoplasia, which suggests the loss of CAR T cell-mediated pairing Active surveillance of leukemia [6].
The determinants of CAR T cell persistence have yet to be fully determined, except for inherent T cell quality (which may depend on the patient and background) [81] and initial T cell phenotype (including the ratio of CD4+ to CD8+) T cells [82], Including the costimulatory domain constructed in each unique CAR construct [83], preclinical reports have shown that the CAR containing the CD28 costimulatory domain has poor durability compared with the CD28 containing the 4-1BB costimulatory domain [45, 84]; These data are in line with clinical experience [6,7,85]. In the above-mentioned clinical trials of tessalyl ribonucleic acid 10, the median duration of CAR T cells based on 4-1BB in the blood is 168 days (range 20-617 days), and B is usually complicated in patients in remission. Cells are underdeveloped.
In contrast, the median duration of CD28-based anti-CD19 CAR T cell persistence is about 30 days, and these cells are rarely detected after 3 months [7,86]. CAR T cells containing the 4-1BB domain have better persistence, which may be partly due to the decreased tendency of T cell failure induced by tonic CAR signal when 4-1BB and CD28 domain mediate co-stimulation.
In addition to other methods [89,90], attempts to calibrate CAR activation potential to optimize response and balance the persistence of effectors relative to memory T cell expansion are ongoing [88]. Other costimulatory domains and multiple costimulatory domains have also been used in CAR constructs, which may affect the persistence of CAR T cells.
In addition, further analysis of the observations of patients with significant expansion and/or persistence of CAR T cells indicates that targeted genomic integration of CAR constructs can enhance persistence. For example, the experience of clonal expansion in CLL patients has shown that TET2 destruction can lead to changes in CAR T cell biology, leading to enhanced potency and central memory phenotypes [91].
Similarly, using the CRISPR-Cas9 editor to specifically integrate the CAR gene into the TCRα constant (TRAC) locus of the T cell genome can produce better resistance than CAR T cells that are routinely transduced in preclinical models. Tumor response [92]. Advances in gene editing technology [93], coupled with a better understanding of the determinants of CAR T cell efficacy and understanding of determinants of treatment responsiveness, will be critical to the design of next-generation CAR T cell technology [36,94].
Therefore, the future direction of improving CAR durability will largely depend on understanding the best T cell biology related to CAR T cell function, and subsequent optimization of CAR T cell design to promote durability (when durability is required). Time).
Clinically, strategies to improve durability independent of CAR T cell design and manufacturing are being tested;
for example, after remission induction, T cell antigen presenting cells (T APC) designed to activate anti-CD19 CAR T cells are administered regularly to determine recurrence Whether stimulation can reactivate and expand CAR T cells numerically and prevent antigen-positive recurrence (NCT03186118).
More broadly, the use of artificial antigen-presenting cells can optimize adoptive T cell immunotherapy by increasing the therapeutic efficacy and durability of infused T cells, thereby providing a potential off-the-shelf method [95]. Transfer of CAR T cells to central memory or stem cell-like memory phenotype is another unique method to enhance treatment response and cell persistence [35,36].
Combining CAR T cell therapy with immune checkpoint inhibitors or other immunomodulatory therapies can provide a synergistic approach to optimize the incidence, depth, and durability of clinical responses [98]. Clinical samples have confirmed evidence of increased PD-1 expression in CAR T cells during the period from infusion to peak expansion, and preclinical data of CAR T cell therapy support PD-1–PD-L1 blockade in improving heparin therapy The role of effect [99,100]. Clinical testing of this strategy using FDA-approved immune checkpoint inhibitors and CAR T cell products has provided anecdotal evidence of improved durability [101].
The persistence of anti-CD19 CAR T cells plays an important role in continuous monitoring, and seems to be important for the lasting remission of ALL patients.
However, it is unclear whether cell persistence is absolutely necessary to maintain the lasting remission achieved by all CAR T cell products. To date, Park and colleagues have reported the longest follow-up data of CD28-based anti-CD19CAR T cell therapy for ALL patients.
In this study, CAR T cell persistence other than induction of remission was rarely detected, but the overall median event-free survival was 6.1 months, and patients with low disease burden (<5% bone marrow blasts) were 10.6 months [9]. Although these findings still prove that the duration of CAR T cell persistence is shorter than that of the 4-1BB-based constructs, these findings still show that the persistence of CAR T cells is beyond the persistence of CAR T cells, which triggers related releases.
Determinants of other issues during the period. It is worth noting that the persistence of remission in patients with B-cell lymphoma is relatively similar to 4-1BB-based products and CD28-based products [71,102], thus indicating that the relevance of CAR T cell persistence may vary depending on the type of cancer.
Careful monitoring of the outcome of anti-CD19 CAR T cells treatment of B-cell malignancies and the results of treatment with CAR T cells targeting other antigens and/or tumor types is very important to fully understand the impact of cell persistence on cell durability .
In any case, the ability of CAR T cells to last for a long time and thus mediate continuous monitoring of disease recurrence is clearly the potential advantage of these drugs over other targeted immunotherapies (such as bispecific or conjugated antibodies), which usually have The limited inducing ability provides long-term and lasting remission [103-106].
The recurrence of antigen-positive disease provides a potential opportunity for retreatment of CAR T cells, although unfortunately, the success of the reinfusion strategy for the treatment of antigen-positive recurrence due to the persistent loss of CAR T cells has been limited. Gardner et al. [8] performed a second anti-CD19 CAR T cell infusion on ten children and young people with ALL.
Eight of these patients lost the persistence of CAR T cells, and only two had CAR T cell expansion after reinfusion, and only one had a complete response [8]. The remaining two patients with detectable CAR T cells were re-infused due to persistent or recurrent CD19+ disease, but none of them experienced substantial CAR T cell re-expansion, B cell hypoplasia or resistance The role of leukemia [8]. Lee et al. [7] described three patients who received a second CAR T cell infusion due to residual or recurrent CD19+ ALL 2–5.5 months after the initial infusion, but none of them had an objective response. Maude et al. [6] used a strategy of repeated infusions to combat the early loss of CAR T cells and related B cell recovery, resulting in the continued survival of CAR T cells [101]. Turtle et al. [31] reported 5 patients with ALL who received reinfusion of anti-CD19 CAR-T cells, none of which had re-expansion, persistence or anti-leukemia activity.
In addition, CAR-specific T cell responses were detected in all five patients, thus suggesting immune-mediated CAR T cell rejection after repeated administration [31]. The same group of patients reported similar poor prognosis after reinfusion of B-cell non-Hodgkin’s lymphoma patients, but the use of an intensive lymphatic phosphorus removal regimen containing fludarabine in addition to cyclophosphamide can improve the reinfusion response.
And improve the initial CAR T unit expansion and durability [107]. This concept of enhanced lymph node dissection has been similarly used in the reinfusion strategy of other CAR-based therapies, thereby improving clinical efficacy [108]. Alternative strategies to optimize reinfusion methods include the use of different CAR constructs or CARs that target different antigens.
Antigen loss or regulation is the mechanism of immune escape.
Targeted antigen modulation is one of the clearest mechanisms for successfully inducing disease relapse after remission using CAR T cells (Table 1), and it has also been used by other targeted immunotherapies (such as bispecific T cell binding agent (BiTE) antibodies). ) Describe constructs [110–112] or monoclonal antibodies [113].
Established mechanisms leading to the loss of CD19 expression include alternative splicing, which produces CD19 isoforms and destroys target epitopes and/or reduces cell surface expression [114,115], and interrupts the transport of CD19 to the cell surface [116]. Other ways to cause the loss of antigen are also under active research.
However, the development of resistance to the initially effective CAR T cell therapy may not require complete loss of antigen-even reduced antigen expression is sufficient. For example, using anti-CD22 CAR T cell therapy, a simple quantitative decrease in CD22 cell surface expression or antigen density in a leukemia population is sufficient to escape CAR T cells.
Therefore, despite CD22 positive, individuals can still relapse in leukemia resulting in the threshold antigen density Relapsed or resistant mutations [15]. Nevertheless, functional and/or retained CAR T cell activity may require a minimum antigen expression threshold-this concept has been implemented in preclinical models that target CD20 in B-cell malignancies and neuroblastoma. ALK[118].
The higher the antigen expression level, the higher the cytolytic activity and cytokine production of CAR T cells. Along these lines of thinking, the preclinical experience of CAR T cell therapy targeting EGFR has shown that the therapeutic potential is particularly dependent on the different antigen densities of EGFR in tumors and non-malignant tissues to limit the target and extra-tumor toxicity while maintaining Anti-cancer activity [119].

In ALL [114,115] patients, the antigen loss after effective CAR treatment is best described, but it is certainly not limited to this disease [120]. The results of preclinical model [121] studies in solid tumor models and the results of clinical studies in patients with glioblastoma [122,123] similarly imply that antigen modulation is a potential trap that undermines the efficacy of CAR T cell therapy.
In future research and the design of novel CAR constructs, it will be necessary to identify the role of antigen density in the anti-tumor response and identify the mechanism that leads to the blockage of target expression in order to optimize the CAR T cell response.
The additive effect of previous targeted immunotherapy may further increase the complexity of immune escape after CAR T cell therapy. For example, anti-CD19 BiTE blinatumomab and anti-CD22 antibody-drug conjugate inotuzumab ozogamicin have been approved by the FDA for the treatment of ALL, and the appearance of CD19-[111,112] or CD22-[113] has been reported in patients treated with these immunotherapies The escape variant.
Therefore, such drugs may make CAR T cells that target the same antigen less effective in future treatments, or reduce the durability of the response by increasing the risk of antigen-negative recurrence. It is worth noting that prior treatment with blinatumomab is the exclusion criterion for the key registration trial of tisagenlecleucel in ALL patients [10].
However, whether it is necessary to avoid targeted immunotherapy before administering CAR T cells to achieve a durable long-term response remains to be determined.
Therefore, the inherent tumor heterogeneity can easily lead to the emergence of antigen-negative clones. It has been thought that CD19 is ubiquitously expressed on all pre-B cell ALL clones, and antigen-negative subclones are formed after treatments targeting CD19.
However, a more detailed analysis of CD19 expression before treatment is necessary because rare patients have harmful cells that are negative or partially expressing CD19 at the time of diagnosis [124].
Indeed, we now have a greater understanding that there can be pre-existing CD19- subclones in diagnosis [115]. Some research data indicate that malignant B-cell progenitors may be CD19-, especially in patients with BCR-ABL1ALL. Medium [125].
Although CD22 is highly expressed in pre-B cell ALL cells, it has a well-described heterogeneity in surface expression, especially in infants with KMT2A (MLL) rearranged ALL, where CD22–ALL cell subgroups The detection of CD22 is more frequent[124,126-128], leading to the appearance of CD22- or CD22dim population after CD22 targeted therapy[15,127].
Lineage switching is another mechanism for evading CAR T cells.
In the context of infant-specific KMT2A rearrangement of leukemia subtypes (usually in the form of mixed-lineage leukemia), this phenomenon has been recognized before the advent of the era of targeted therapy, and patients have converted to AML after specific treatment for ALL, and vice versa The same goes for [129]. In preclinical and clinical settings, similar phenomena of myeloid subtypes have been reported after CD19 targeted immunotherapy in ALL patients with or without KMT2A rearrangement [16,17,110,125].
Similarly, in the preclinical ALL model, targeting FLT3 with CAR T cells can induce a reversible conversion of B cells to T cell lineage (while effectively avoiding conversion to FLT3+ myeloid lineage leukemia) [130]. Whether this resistance mechanism is effective in non-leukemic malignancies remains to be determined.
Although antigen regulation is regarded as a mechanism of immune escape, we currently have the ability to predict which patients are at high risk of developing antigen-regulated recurrent disease, except for those patients who have identified existing antigen-negative subclones, and those in antigen expression Patients with established heterogeneity or patients who have received previous immunolabeling against the same antigen.
The minimal residual disease (MRD) monitoring strategy based on flow cytometry is essential to identify the existence of subpopulations that may not be fully suitable for targeting a single antigen, and the responsibility for proactively screening for antigen-negative diseases is greater; therefore, , Will require more complex flow cytometry gating methods and other improvements in the characterization of single-cell immunophenotypes, especially when the burden of disease is low.
Tracking leukemia clones over time through assisted PCR and/or molecular assessment of VDJ immunoglobulin heavy chain (IgH) rearrangement may improve disease recurrence by identifying cell populations that have not been completely eradicated or incompletely eliminated by CAR T cell therapy The prediction can be easily identified using flow cytometry.
Therefore, in the phase I study of anti-CD19 CAR T cell therapy, Gardner et al. [8] found that according to flow cytometry assessment, 27 of 40 patients in MRD-negative remission (67.5%) also used next-generation sequencing . Most of these patients (17 of 27 patients; 65%) subsequently achieved complete molecular remission on day 63, although several patients did not, indicating that the persistence of leukemia may eventually be a precursor to future recurrence .
Considering the tendency of antigen modulation as a mechanism to evade effective immunotherapy, CAR constructs that incorporate multiple antigen targeting are being developed to address the inherent tumor heterogeneity and thus reduce the risk of recurrence of leukemia.
Preclinical data supporting the multi-target approach includes the use of tandem anti-CD19–CD20 CAR constructs [131], combined anti-CD19 and anti-CD123 (also known as IL-3Rα) strategies [132], and the use of single CAR construct targeting Both CD19 and CD22 target antigens or two unique CARs for each antigen [133], and multiple clinical trials of these strategies are ongoing (Table 2).
The development of multiple antigen-targeting combinatorial strategies to ensure an effective response to each antigen is crucial: the preference of one antigen over another may lead to bias towards functional responses to only one antigen without Eliminate the recurrence of antigen-negative problems.
However, the development of functional multi-target constructs is not an easy task, and it is highly dependent on preclinical testing to identify biologically active constructs that have the same ability to simultaneously target simultaneous antigens, which has been very important in Qin and colleagues. Described well [133].

The role of consolidation therapy after CAR T cell-induced remission.
Considering the concern about the recurrence of antigen-positive or antigen-negative diseases, the need to consolidate the remission induced by CAR T cells needs to be considered. The first successful clinical application of CAR T cell therapy was in patients with hematological malignancies.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a validated treatment option; therefore, the use of allogeneic-HSCT for consolidation therapy is very relevant Topic, especially if no previous transplant has been done. In the initial reports of Davila et al. [86] and Lee et al. [7,134], respectively, a high proportion of adults, children and adolescent adults entered remission after receiving CD28-based anti-CD19 CAR T cell therapy, allogeneic hematopoietic stem cell transplantation, Overall improvement.
Specifically, in an analysis, combined with data from the anti-CD19 and anti-CD22 CAR T cell product trials conducted at NCI, 25 patients were subsequently subjected to allo-HSCT, which was the first allo-HSCT134 of 19 patients. Using a competitive risk analysis (recurrence risk and transplant-related mortality), among all 25 patients and 19 patients undergoing HSCT for the first time, the 24-month cumulative incidence of allo-HSCT recurrence was 13.5% (95% CI3.2– 32.1%) and 11.3% (95% CI 1.7–31.1%) [134].
Obstacle 3: Toxicity associated with CAR T cells
In the past few years, some in-depth reviews of the latest knowledge and management methods related to CAR T cell-related toxicity have been published in this journal and elsewhere [136-142]. It is worth noting that efforts are being made to establish a unified multicenter grading scale. In this regard, the original CRS grading performance proposed by Lee et al. [141] has been updated and published as the “American Society of Blood and Bone Marrow Transplantation Consensus Guidelines” [143] .
Algorithms and treatment methods to optimize the safety of CAR T cell therapy are being studied, including early intervention strategies [144], and the use of suicide genes and other genetic engineering strategies to reduce CAR T cell toxicity [145].
Of particular relevance to the discussion in this article is that severe or even fatal CRS and other toxicities are barriers to persistent CAR T cell-induced remission in some patients. In this regard, in addition to established literature and development guidelines, we Two methods are also provided and other areas to be considered.
First, we must recognize the fact that the literature on CRS management is mainly based on the experience of anti-CD19 CAR T cell therapy trials.
Therefore, because of targeting novel antigens, it is important to realize that not all CRS cases are the same, and therefore, appropriate intervention strategies may vary. For example, in the absence of any early intervention strategies, the CRS observed after anti-CD22 CAR T cell treatment appears to be less severe than that observed with anti-CD19 CAR T cells.
However, new toxicities have emerged for targeting CD22, such as clinically related coagulopathy, which requires different treatment methods (N.N.F. and T.J.S., unpublished observations).
Second, as the treatment of CRS and/or other toxicants becomes better, it will be equally important to evaluate the effects of such treatments, especially to reduce the impact of CRS preemptive or preventive strategies on anticancer activity.
At present, limited available data show that early intervention strategies can effectively reduce the severity of CRS without compromising the peak expansion or functional durability of CAR T cells [144]. However, these data come from a single experiment using a single CAR configuration, and therefore may not be widely applicable. A trial is currently underway to study the best time to use tocilizumab for anti-IL-6 therapy to treat CRS associated with anti-CD19 CAR T cell therapy (NCT02906371).
Obstacle 4: Beyond leukemia
In view of the success achieved so far in a large number of pretreated patients, the early use of CAR T cells has great potential to change the treatment model for children and adults with relapsed and/or refractory or high-risk B-cell malignancies. In fact, efforts are being made to understand how best to incorporate these therapies into pre-treatments to improve overall efficacy. However, when the application of CAR T cells expands to cancers other than ALL, there are substantial obstacles.
CAR T cell response, persistence and recurrence of lymphoma. Antigen loss may be a mechanism of lymphoma recurrence after CAR T cell therapy [120,146], but it seems that the incidence of B-cell lymphoma is lower than that of ALL patients (Table 1). It is worth noting that there are limited reports on the frequency of antigen loss in patients with B-cell lymphoma. This may be due to the fact that the sampling frequency of lymphoma disease is lower than that of leukemia patients, but it is still an important consideration for patients with lymphoma recurrence after CAR T cell therapy.
The CAR T cell strategy goes beyond B cell targeting.
CD19 is commonly expressed on most B cells. Targeting non-malignant and malignant CD19+ cells is a treatment strategy with acceptable safety, while targeted therapy, non-tumor toxicity may be more inhibitory in other cancers. For example, for AML, broad targeting of myeloid lineage cells, especially continuous, is unacceptable, and supportive interventions cannot be used to make the immune system simpler, such as immunoglobulin replacement therapy for patients with chronic B-cell dysplasia .
In this case, using less durable CAR T cell products and giving allogeneic donors to rescue stem cells after an effective CAR T cell response may be a reasonable strategy. The first human study using CAR T cells containing anti-CD123 and CD28 domains to target bone marrow cells showed that their anti-leukemia activity has a promising future, but the bone marrow suppression effect is not prolonged [148]. It is planned to conduct clinical testing of CD28-based anti-CD33CAR T cell products targeting bone marrow cells [149].
A key problem with solid tumors is that inherent tumor heterogeneity may be a major obstacle to determining the best target, and relatedly, antigen loss may be a key factor in ruling out the cure rate.
In fact, the antigen density of antigen expression in solid cells (as described above, regarding ALK in neuroblastoma cells [118]) and the inherent tumor heterogeneity (for example, mesothelin 154 expressed by non-small cells, HER2 (Reference 155) or MUC1 (Reference 156)) lung cancer) may limit the therapeutic potential of drugs that target a single antigen and raise concerns about different targets and extra-tumor toxicity.
Among the fastest-growing CAR T cell-based strategies, products targeting disialioganglioside GD2 have shown anti-tumor activity in patients with neuroblastoma, leading to complete remission [157], thus emphasizing the effect on solid tumors. The potential for CAR T cell therapy.
In addition, overcoming the immunosuppressive tumor microenvironment may lead to inactivation of adoptively transferred T cells, which is particularly relevant for effective solid tumor CAR T cell therapy. Several methods to overcome this problem are currently being evaluated, including optimizing the preparation protocol prior to infusion of CAR T cells [150,158].
Armored CAR T cells that constitutively secrete pro-inflammatory cytokines as a mechanism to overcome local immunosuppression are a new concept. Similarly, combining immune checkpoint suppression into CART cell-based strategies through various combinations or built-in methods may improve the response [98]. The results of several preclinical studies support the effectiveness of this method, and further clinical validation is needed [98,152,159,160].
Targeting CNS tumors requires careful consideration of the optimal delivery mechanism for CAR T cell therapy.
A case report in 2016 described the use of CAR T cells targeting IL-13 receptor subunit α2 (IL-13Rα2) in patients with glioblastoma. Multiple infusions (into the tumor resection) cavity within a month and then into the ventricular system [122]). The patient’s clinical response was impressive, with all intracranial and spinal tumors completely regressing for 7.5 months [122].
The strategy for optimizing the strategy for IL-13Rα2 includes the use of enriched central memory T cells to design the second-generation CAR product of the 4-1BB costimulatory domain. In the orthotopic glioblastoma model, the product is effective regardless of corticosteroid therapy (the main treatment of glioblastoma), and the efficacy of intraventricular infusion is higher than that of intravenous delivery (in multifocal It may also be higher in disease than intratumoral administration) [161].
Anti-GD2 CAR T cell therapy for histone H3 lysine 27-methylation (H3K27me) diffuse midline glioma (a pediatric CNS tumor that is fatal) is another promising approach [162]. CART cell-based medulloblastoma targeting based on anti-HER2, 4-1BB domains has also shown efficacy in both mouse and non-human primate models, and has good tolerance to intraventricular administration Sex [163].
Most notably, HER2-specific CAR T cells have been tested in a phase I dose escalation study involving patients with progressive glioblastoma. The preliminary results prove the safety and feasibility of this method. And because some adrenal cortex hormones provide early signs of activity, one patient’s condition is relieved while the other patients’ disease is stable [164].
Similarly, in patients with glioblastoma, EGFRvIII-directed CAR T cells were found to be safe and feasible, but it can be seen from ALL patients that antigen loss and tumor heterogeneity are the main determinants of immune escape[123] . Therefore, optimizing CAR T cell methods and testing new delivery mechanisms for CAR T cells targeting CNS diseases are still active areas of research.
Summary:
Many challenges must be overcome in the optimization of CAR T cell therapy for diseases other than ALL, but great progress has been made in the past few years.
The lessons learned from the strategy for B cells will provide the basis for the advancement of this research field, but careful methods are needed to understand and try to mitigate the novel toxicities associated with CRS and the early non-target toxicities that may lead to tumor metastasis.
It gave up promising new strategies based on CAR T cells to treat solid tumors.
(source:internet, reference only)
Disclaimer of medicaltrend.org