Clinical application of interleukin in tumor immunotherapy
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
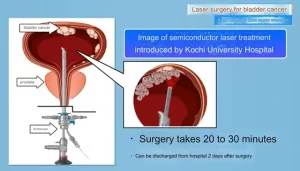
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
Clinical application of interleukin in tumor immunotherapy
Clinical application of interleukin in tumor immunotherapy. Interleukins and related cytokines are the communication means of innate and adaptive immune cells and non-immune cells and tissues.
Therefore, interleukins play a key role in the occurrence, development and control of cancer, and some interleukins are particularly related to the occurrence and development of cancer. A variety of cell sources, receptors and signal pathways determine the pleiotropic effects of interleukins in cancer.
Interleukins can cultivate an environment conducive to cancer growth and are also a necessary condition for tumor-directed immune responses.
These properties of interleukins can be used to improve immunotherapy to increase efficacy and limit side effects. In recent years, the therapeutic potential of interleukins has always been a hot spot in tumor basic and translational research. More and more clinical trials are currently underway highlighting their value as therapeutic drugs and targets.
Therapeutic neutralizing antibody
IL-1
The CANTOS study provides the strongest evidence for the neutralizing effect of IL-1 in cancer. The study included patients with stable coronary heart disease who received standard treatment, but the level of high-sensitivity C-reactive protein (hsCRP) continued to rise. The patient had no cancer diagnosis at the time of enrollment, and was subsequently treated with the anti-IL-1β antibody canakinumab. The results showed that compared with the placebo group, canakinumab not only reduced hsCRP levels, but also significantly reduced the overall cancer mortality after the occurrence of cancer, especially lung cancer.
This discovery gave birth to some clinical trials that block IL-1β. In 2018, canakinumab began a phase III trial of monotherapy and placebo in patients with non-small cell lung cancer (NCT03447769). Similarly, a phase II trial investigating canakinumab as a single agent in the treatment of myelodysplastic syndrome and chronic myelogenous leukemia began in 2020 (NCT04239157).
In 2018, a phase III trial of canakinumab combined with pembrolizumab and chemotherapy for the treatment of non-small cell lung cancer (NCT03631199) was started, and a phase III trial of canakinumab and chemotherapy alone (NCT03626545) was started in 2019.
IL-6
IL-6 can protect cancer cells from treatment-induced DNA damage, oxidative stress, and apoptosis, and can induce immunosuppression and maintain a cancer stem cell population that is highly resistant to treatment. Therefore, the neutralizing effect of IL-6 may reverse resistance to traditional cancer treatments.
The anti-IL-6 antibody siltuximab slowed tumor growth in a xenograft cholangiocarcinoma model, but as a monotherapy, it achieved only very limited results in multiple myeloma. Siltuximab is also ineffective as a monotherapy for solid tumors. In prostate cancer, the best result obtained is stable disease; in renal cell carcinoma (RCC), the best result obtained is 1 case of PR, in a group of mixed solid tumors No clinical efficacy was observed. In addition, some clinical trials have observed treatment-related side effects, such as a higher infection rate after siltuximab treatment, which generally does not support siltuximab’s anti-tumor treatment.
Combined with chemotherapy, the anti-IL-6R antibody tocilizumab showed positive results for the first time. However, the combination of neutralizing IL-6 and immune checkpoint inhibitors (ICIs) has caused controversy. Although IL-6 neutralization may allow patients to continue to receive ICIs by reducing the cytokine release syndrome, IL-6 inhibition can inhibit the expression of PD1 and PD-L1, which may reduce the effectiveness of ICIs. As preclinical studies have proven to neutralize the synergy between IL-6 and ICIs, some clinical trials have begun to test this combination in patients.
IL-8
HuMax-IL-8 is an IL-8 neutralizing antibody. Although there is no objective response to monotherapy, 73% of patients with solid tumors have stable disease and no dose-limiting toxicity. IL-8 induces resistance to multiple chemotherapeutics and ICI. Therefore, some clinical trials are exploring the combination of HuMax-IL-8 with Nivolumab (NCT03400332, NCT04123379 and NCT04050462), combined with Nivolumab and degarelix (NCT03689699), and Nivolumab and radiotherapy ( NCT04572451).
IL-17
In a mouse gastric cancer model, blocking IL-17 can slow down tumor growth, and combined with anti-PD1 therapy can clear 80% of tumors. In preclinical mouse prostate cancer models, neutralizing IL-17 also slowed tumor progression. In addition, IL-17 can accelerate the progression of multiple myeloma. Preclinical studies have shown that neutralizing IL-17 can indeed lead to a reduction in the growth of multiple myeloma. A clinical trial started in 2017 is currently exploring the efficacy of the anti-IL-17A antibody CJM112 in multiple myeloma (NCT031111992).
IL-23
In castration-resistant prostate cancer, IL-23 derived from MDSC has been shown to activate the androgen receptor pathway, thereby supporting the survival and proliferation of cancer cells under androgen deficiency conditions. In mouse models, neutralizing IL-23 antibodies can significantly reduce tumor growth and prolong survival, which suggests that anti-IL-23 therapy may support anti-androgen therapy. To assess this potential, the anti-IL-23 antibody tildrakizumab is currently in a phase I/II trial for castration-resistant prostate cancer patients in combination with the androgen synthesis inhibitor abiraterone (NCT04458311).
IL-33
Preclinical studies have shown that IL-33 can directly act on tumor cells, induce polyploidy and rapid proliferation, and cause treatment resistance. The use of specific IL-33 blocking antibody can restore the efficacy of anti-PD1 therapy for ICI-resistant B16F10 melanoma.
Recombinant and engineered interleukin

IL-2
Although high-dose IL-2 treatment induces a lasting complete response in some patients with melanoma and renal cell carcinoma, it is also accompanied by potentially life-threatening adverse events. Therefore, low-dose IL-2 regimens have been evaluated in some trials, however, at low abundance, IL-2 preferentially binds to its high-affinity receptor expressed on Treg cells, which may lead to immune evasion. Therefore, several IL-2 variants with enhanced affinity for IL-2R expressed on CTL are under development.
Bempegaldesleukin is a pegylated IL-2 variant. In addition to increasing its half-life, the coupling of polyethylene glycol to IL-2 blocks its binding site to the high-affinity subunit IL-2Rα. Over time, the PEG group will be lost and the active form of Bempegaldesleukin will be continuously released, thereby minimizing the risk of overdose.
In a phase I clinical trial for patients with metastatic solid tumors (mainly including melanoma or renal cell carcinoma), the best response observed with bempegaldesleukin monotherapy was stable disease, compared with traditional IL-2 therapy in melanoma This is disappointing compared with the long-lasting CR of 7% and 9% for renal cell carcinoma. However, bempegaldesleukin shows good safety and encourages its use in combination with ICIs. In a phase I clinical trial for metastatic solid tumors, bempegaldesleukin combined with nivolumab achieved a complete remission rate of 19%. Other clinical trials in combination with ICIs, including phase III clinical trials for patients with bladder cancer (NCT04209114), RCC (NCT03729245) and melanoma (NCT03635983) are currently underway.
Other IL-2 variants are also undergoing clinical trials in conjunction with ICIs, such as ALKS 4230, a circular structure of IL-2 and IL-2Rα designed to selectively activate intermediate affinity IL-2R. Currently, four clinical trials are evaluating the effects of monotherapy and combination therapy with pembrolizumab in patients with advanced solid tumors or noncutaneous squamous cell carcinoma of the head and neck (NCT04592653, NCT02799095, NCT03861793 and NCT04144517). THOR707 is an engineered non-α IL-2 variant that is being evaluated for the efficacy of monotherapy or combination therapy with ICI or anti-EGFR antibody in patients with solid tumors (NCT04009681).
NARA1 is a fusion protein structure formed by the fusion of IL-2 and anti-IL-2 antibody NARA1. NARA1 therefore permanently masks the CD25 binding site of IL-2, thereby eliminating CD25-mediated Treg cell development. It showed effective anti-tumor response in mouse melanoma model. Some other IL-2 variants also include RO6874281, RO7284755, Darleukin, etc. The clinical trials of these drugs are ongoing, as shown in the table below.

IL-10
IL-10 has anti-inflammatory and CTL stimulating properties, which makes it a potential anti-cancer drug. The PEGylated IL-10 variant pegilodecakin can induce systemic immune activation, increase the level of immunostimulatory cytokines, and reduce the expression of TGF-β in patients with solid cancer.
In clinical trials, pegilodecakin treatment can observe PR and long-term disease stability. In a follow-up clinical study, the expansion and activation of CTL in the tumor was observed after treatment. In addition, the first clinical trial of the combination of pegilodecakin and ICIs also showed promising results; however, due to the poor risk-benefit ratio, the two follow-up trials of the combination of nivolumab (NCT03382912) and pembrolizumab (NCT03382899) were terminated early.
CmAb-(IL-10)2 is a fusion protein consisting of anti-EGFR cetuximab and IL-10 dimer. It is still in the preclinical research stage and shows superior anti-tumor activity.
IL-12
IL-12 has significant immune activation and tumor control effects, but it can cause serious adverse reactions at the dose required to induce anti-tumor effects. However, the targeted drug delivery strategy enables IL-12 to reach a high concentration at the tumor site while avoiding systemic reactions, which has stimulated people’s interest in IL-12 in cancer treatment.

Gene therapy can better control the location and quantity of interleukins in the treatment plan. Tavokinogene telseplasmid is an IL-12 encoding plasmid that was electroporated into melanoma lesions. In the phase II trial, the ORR was 36% and the CR was 18%. It is worth noting that 46% of patients experienced regression in at least one lesion not injected with Tavokinogene telseplasmid, and 25% of patients experienced regression in all lesions not injected with Tavokinogene telseplasmid, indicating that systemic anti-tumor immunity was induced. In addition, when combined with pembrolizumab, the ORR was increased to 41% and the CR was 36%. In addition, a number of clinical trials have been conducted on triple negative breast cancer (NCT03567720), head and neck squamous cell carcinoma (NCT03823131) and melanoma (NCT04526730 and NCT03132675).
CBD-IL-12 is a fusion protein composed of IL-12 and collagen binding domain. Collagen will be exposed in tumor vascular disorders, and CBD-IL-12 will accumulate in the tumor. Through extensive activation of the immune system at the tumor site, it shows better anti-tumor effects than IL-12.
In addition, there are multifunctional oncolytic nanoparticles, the purpose is to send several different signals at the same time to trigger anti-tumor response. Studies have shown that nanoparticles composed of self-replicating RNA can induce tumor cell death, because the contained RNA acts as a signal for pathogen recognition receptors and encodes IL-12, which further enhances the induction of immune responses.
IL-15
Compared with IL-2, IL-15 does not cause the expansion of Treg cells and has similar immunostimulatory properties.
ALT-803 is another dimeric protein containing IL-15 mutant (IL-15N72D) and IL-15RαSu/Fc, which has been shown to have excellent anti-tumor activity in mouse models. In the first human phase I trial (NCT01885897), ALT-803 treatment was well tolerated, but clinical response was observed in 19% of patients with hematological malignancies. Another dose-escalation phase I trial was recently conducted to evaluate the safety and efficacy of ALT-803 combined with nivolumab in the treatment of patients with advanced non-small cell lung cancer (NSCLC) (NCT02523469); no dose-limiting toxicity was recorded, 6 out of 21 patients Name gets an objective response. The continuous recruitment of patients in the second phase is ongoing.
BJ-001 is the world’s first tumor-targeting IL-15 fusion protein independently researched and developed by Boge Biosciences and has a global patent. Its design not only overcomes the shortcomings of recombinant IL-15’s short half-life, but more importantly, the tumor targeting molecule in its domain allows it to be enriched in tumors with high expression of αvβ3, αvβ5 and αvβ6 integrins, thereby having a reduction system Toxicity, the potential to enhance curative effect.
The clinical trials of other IL-15 variants are shown in the following table:

IL-18
The preclinical efficacy of IL-18 treatment is limited, which may be due to IL-18BP, a high-affinity IL-18 decoy receptor. At present, researchers use direct evolution technology to develop anti-bait IL-18 (DR-18), which maintains the signal transduction potential and supports the development of effector T cells, reduces T cell failure, and enhances the activity and maturity of NK cells. And other ways, exert a powerful anti-tumor effect in mice.
IL-23 and IL-36
The combined application of IL-36γ with IL-23 and OX40 ligands has been successfully used to promote acute inflammation in preclinical animal models to effectively control tumors. It is currently being studied in clinical trials (NCT03739931).
Supplement to adoptive cell therapy
Adoptive Cell Therapy (ACT) is an important breakthrough in the field of cancer treatment in the past decade. Interleukins such as IL-2, IL-7 and IL-15 have been widely used to improve the in vitro expansion and differentiation of adoptive cells, and they have been introduced into metastatic cells through co-administration or genetic engineering to assist in the treatment of ACT.

IL-2
Treatment with IL-2 to support ACT has achieved varying success in several cancer types. For example, IL-2 is combined with TIL in melanoma. In addition, the combination of CAR-T cells and IL-2 has also obtained benefits in some trials, but this method still faces similar toxicity problems as using interleukins alone.
The strategy to overcome the toxic effects of systemic IL-2 therapy while maintaining its ability to support ACT therapy is to pair the designed IL-2 with IL-2R. The designed IL-2 cannot bind to wild-type IL-2R, but can bind to the designed IL-2R to transmit natural IL-2 signals. This design avoids systemic toxicity. In the mouse melanoma model, it showed enhanced ACT product efficacy and negligible toxicity.
IL-8
A completely different approach is to use tumor-related interleukins, such as IL-8, to improve the infiltration of CAR-T cells into tumors by overexpressing the corresponding receptors. In preclinical models of glioblastoma, ovarian cancer, and pancreatic cancer, the expression of IL-8 receptor CXCR1 or CXCR2 in CAR-T cells significantly enhanced migration and persistence in tumors, and induced tumors The complete disappearance and lasting immune memory.
IL-12
Another strategy currently used in some trials is to express certain interleukins through cell therapy products. In this way, interleukins are only expressed locally at the tumor site, thereby avoiding systemic toxic effects and recruiting additional immune cells to establish an immune response against the CAR antigen-negative tumor cell population. This method is called “T cell redirected antigen non-restrictive cytokine-initiated killing” (TRUCKs). IL-12 was the first interleukin used in TURCK’s proof of concept, and other interleukins, such as IL-7, IL-15 and IL-23, have since been used in CAR-T cell design.
In preclinical trials, the IL-12 expression of CAR T cells leads to the recruitment and activation of macrophages, which are essential for eliminating cancer cells, and the loss of cancer cell antigens usually escapes CAR-induced killing. The first clinical trial was for patients with metastatic melanoma. However, the study had to be terminated due to the possibility of serious toxic effects due to excessive release of IL-12. Recently, some clinical trials have begun to use CAR-T cells that express IL-12 with a safety switch in an attempt to avoid uncontrolled IL-12 release.
IL-7
IL-7 and CC chemokine ligand 19 (CCL19) are necessary to maintain the T cell area of lymphoid organs. Before the clinic, compared with traditional CAR-T cells, CAR-T cells expressing IL-7 and CCL19 are superior to conventional CAR-T cells in tumor killing. Histopathological analysis showed that the infiltration of DCs, CAR-T cells and endogenous T cells in the tumor increased. Currently, there are 4 clinical trials evaluating the effect of CAR T cells overexpressing IL-7 and CCL19 (NCT03198546, NCT03929107, NCT03932565 and NCT04381741).
IL-15
Pre-clinical studies have shown that the expression of IL-15 in NKT cells leads to a decrease in the expression of depletion markers, an increase in continuity in the body, an enhanced tumor location and an improved tumor control ability. In CAR-T cells, membrane-bound IL-15 leads to an increase in the abundance of T memory stem cells, and the duration is long, which has a good effect on CD19+ leukemia. Ongoing clinical trials have introduced engineered IL-15 into CAR-T cells and CAR NKT cells. Interim analysis showed that IL-15-expressing anti-GD2 CAR NKT cells have no effect on 3 children with refractory neuroblastoma. Dose-limiting toxicity, the tumor site showed the presence of CAR NKT cells, and one patient had regression of bone metastases.
IL-23
IL-23 is a recently reported method to replace potentially toxic interleukins such as IL-12 and IL-15. A preclinical study showed that engineered CAR-T cells containing IL-23 subunit p40 can generate autocrine IL-23 signals, promote the selective proliferation of activated T cells, and improve anti-tumor ability. In addition, the side effects seem to be reduced compared to the use of IL-18 or IL-15.
Summary
In general, interleukin monotherapy still faces great limitations, and many new strategies have recently emerged to solve these problems. This trend is shifting from using the natural form of interleukins to complex engineering methods, involving changing the receptor affinity of target cell populations or designing tumor-targeted fusion structures to improve efficacy and reduce systemic toxicity.
In addition, in order to increase the application rate of interleukin therapy, combination therapy is becoming more and more important. New insights into how interleukins affect tissue repair, cancer progression, and immune evasion will greatly help determine how interleukins participate in resistance to established therapies such as chemotherapy or ICI treatment. Therefore, interleukin therapy can unleash the potential of other therapies, thereby helping drug-resistant patients benefit from them.
In short, interleukin is a key element for coordinating TME and controlling tumor-immune cell interaction. Interleukin has made a lot of exciting new progress in preclinical and clinical research in the treatment of cancer. These studies will have more interesting results in the next few years. .
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.