Seven categories of biomarkers: definitions and application considerations
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
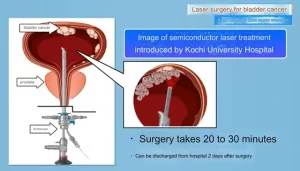
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
Seven categories of biomarkers: definitions and application considerations
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Seven categories of biomarkers: definitions and application considerations.
A biomarker is an indicator used to evaluate normal biological processes, pathogenic processes, and response to exposure or intervention measures.
1. Diagnostic Markers
Definition
Diagnostic biomarkers can detect or confirm the presence of a disease or condition, or identify an individual with a subtype of the disease. These biomarkers can be used not only to identify patients with diseases, but also to redefine the classification of diseases.
Application and precautions
A diagnostic biomarker requires sufficient accuracy and reliability. Therefore, a verification method is needed to ensure that biomarkers are low-cost, reliable, accurate, and reproducible. Normally, the detection method has not been validated, which can lead to misleading assumptions about the value of the biomarker.

Steps in the evaluation framework for biomarkers (Experimental Biology and Medicine 2018; 243)
The complexity of verification can be seen in the use of troponin. As an important biomarker for the diagnosis of acute myocardial infarction, various detection methods of troponin vary greatly in operation, especially under the lower threshold, misclassification may lead to major deviations in treatment measures. When small increases in troponin occur at previously undetectable levels, the clinical consequences are unclear.
If diagnostic biomarkers go beyond general applications, such as transfer to prospective research or clinical practice, you must pay close attention to the context of use.
Diagnostic biomarkers are valuable in one set of clinical situations, but can be misleading in another. For example, in low-prevalence diseases such as pancreatic cancer or ovarian cancer, the new diagnosis is psychologically devastating or the test is invasive, and the biomarker must have a very low false positive rate. On the other hand, in screening for hypertension or hyperlipidemia, there is little risk of repeated assessments, a high false positive rate is tolerable, and the focus of attention may be the false negative rate.
In addition, decision-making thresholds and clinical utility are becoming important measures to evaluate the value of biomarkers in clinical applications.
2. Monitoring markers
Definition
When a biomarker can be continuously measured to evaluate diseases (exposure to medical products or environmental agents), and to evaluate the effects of medical products or biological agents, it is a monitoring biomarker.
Monitoring markers is a broad concept, so other types of biomarkers overlap.
Application and precautions
Monitoring biomarkers has important value in clinical care. When treating blood pressure or using low-density lipoprotein (LDL) cholesterol-lowering drugs, blood pressure or low-density lipoprotein cholesterol levels are monitored. Similarly, when treating HIV infection, the CD4 count is monitored.
The monitoring of clinical applications needs to be intuitive, but the changes of biomarkers and the clinical process and decision-making are complicated and often not as accurate as ideal.
For example, the measurements of hemoglobin (Hb) A1C, blood pressure, and LDL cholesterol are reversible. In addition, the test interval and duration require sufficient experience accumulation. Many biomarkers that are routinely used in clinical practice have very imprecise operating characteristics, so it is necessary to combine clinical “Gestalt” and “clinical judgment”.
When medical products are being developed, changes in biomarkers are often used to determine whether a critical threshold has been reached, and developers can use this to conclude whether the target is sufficient to be worthy of continued development.
Monitoring biomarkers is also important to ensure the safety of human research participants. For example, the safety threshold of drugs that may have hepatotoxicity is measured by continuous monitoring of liver function, and cardiovascular events are measured by using continuous troponin.
Monitoring biomarkers can also help measure pharmacodynamic effects, detect early evidence of treatment response, and detect complications of disease or treatment.
Many researchers and clinicians hold an unchanging belief that changes in biomarker results are a measure of the effectiveness of drugs in patients or populations. However, in many cases, actual measurement results, rather than changes, are the best predictors of clinical outcomes, even if changes are the best way to monitor whether the treatment itself is effective. For example, angiotensin-converting enzyme (ACE) inhibitors may cause an increase in serum creatinine and/or potassium, which provides a measure of the effect of drugs. However, the risk to patients or study participants is mainly determined by the measured absolute levels of creatinine or potassium, rather than changes in potassium levels.
3. Pharmacodynamic markers
Definition
When the level of a biomarker changes with the use of medical products or environmental agents, it can be called a pharmacodynamic/response biomarker.
Application and precautions
This type of biomarker is very useful in clinical practice and early drug development. For example, if a person is being treated for hypertension or diabetes, and the treatment does not lower blood pressure or blood sugar, there is a good reason why the drug or treatment plan is ineffective, and another intervention is sought.
Similarly, in phase 1 clinical trials, drug candidates that do not change the key parameter of biomarkers may not be worth studying. Of course, for normal people participating in the Phase 1 study, significant changes in the baseline values of disease-related biomarkers (for example, blood pressure) are undesirable. If a major change occurs, it is necessary to prove whether the drug is safe for use in patients with the target disease. For many drugs, the dose to be administered is determined by measuring changes in pharmacodynamics/response biomarkers at the time of treatment.
However, the interpretation of pharmacodynamics/response biomarkers is not simple. For example, biomarkers in the acute phase cannot reflect the long-term effects of patients, and different patients have different responses to the same therapeutic dose. How do biomarkers reflect this difference? Therefore, it is necessary to screen and verify whether the changes in pharmacodynamics/response biomarkers provide reliable signals for the expected treatment response.
Another problem is that sometimes easily measurable biomarkers do not reflect the true pharmacodynamic response. For intravenous fibrinolytic drugs, serum pharmacokinetics does not reflect the drug’s activity in thrombosis. Similarly, amiodarone is deposited in fat in large amounts, so its duration of activity is much longer than predicted by a simple measurement of serum levels.
4. Predictive markers
Definition
Predictive biomarkers are the presence or changes of biomarkers, which can predict that an individual or a group of individuals are more likely to have a favorable or unfavorable impact from the medical product or agent exposed to the environment.
Verify predictive markers
Want to prove whether a biomarker is useful in this regard? A rigorous clinical research method is needed. Ideally, patients with or without biomarkers are randomly assigned to one of two or more treatment regimens (or placebo-controlled), and the difference in the outcome of the treatment is the same as the presence, absence, or absence of biomarkers. The difference in level is significantly related.
Application and precautions
The design and implementation of predictive biomarkers in clinical trials can help focus on the development of strategies. Especially in the pre-registration stage, the enrollment population is concentrated on participants who predict elevated levels of biomarkers, and patients whose treatment may be “effective” are recruited.
The use of predictive biomarker enrichment is a more targeted approach than the use of prognostic biomarkers. These markers can be used to increase the incidence of events, but it is not possible to select specific patients who are more likely to respond or not to respond to treatment.
The same idea is the basis of the current consensus on treatment options in clinical practice. For example, antihypertensive drugs are used for hypertensive patients; blood transfusion is used for patients with anemia with low hemoglobin; acute reperfusion is suitable for patients with elevated ST segment on the electrocardiogram, and patients with high levels of glycosylated hemoglobin benefit the most from active treatment of diabetes.
A major growth area for predicting biomarkers is the genetic and genomic markers of precision medicine. For example, patients who are PD-1/PD-L1 positive are more sensitive to immune checkpoint inhibitors.
5. Prognostic biomarkers
Definition
Prognostic biomarkers are used to identify patients with disease or disease symptoms, the likelihood of a clinical event, disease recurrence, or disease progression.
Application and precautions
In clinical trials, prognostic biomarkers are usually used to set trial entry and exclusion criteria to identify high-risk groups. The key issue is that the statistics of an experiment are determined by the number of events rather than the sample size. If the high-risk population is enriched, the amount of time will increase; if the treatment is effective, the difference in the treatment result will be enlarged in number.
In addition, prognostic biomarkers are particularly important in predicting the risk of an individual’s event or poor prognosis. This information is the key to determining the length of hospitalization and/or intensive care unit stay.
Another major use of prognostic biomarkers is the rational allocation of resources. Healthcare institutions can distinguish which patients can benefit from more intensive monitoring and evaluation, and others avoid unnecessary additional diagnostic tests or medical interventions.
6. Safety Markers
Definition
Safety biomarkers are measured before or after exposure to medical interventions or environmental agents to indicate the likelihood, existence, or extent of toxicity as an adverse event.
Application and precautions
For many treatments, monitoring liver, kidney, or cardiovascular toxicity is essential to ensure that a given treatment can be safely maintained. Safety biomarkers help identify patients who are experiencing adverse reactions to treatment. When using antiarrhythmic drugs, prolonging the QT interval of the ECG is a safe biomarker because it can predict the risk of fatal arrhythmia and can be used to identify patients who need effective treatment.
Similarly, safety biomarkers can be used to monitor people exposed to environmental risks, or to continue monitoring after exposure.
7. Susceptibility/risk markers
Definition
A biomarker that characterizes the likelihood of a certain disease in an individual who currently has no obvious clinical disease is classified as a susceptibility/risk biomarker.
Application and precautions
Such biomarkers are the basis for conducting epidemiological research on disease risk.
Brief comment:
1. Our ability to accurately use biomarkers in the development of new drugs is not very strong, especially in traditional medicine.
2. In clinical practice, the accurate use of various markers and the thinking of systemic treatment still need to be cultivated.
References:
Robb MA, McInnes PM, Califf RM. Biomarkers and surrogate endpoints: developing common terminology and definitions. JAMA 2016;315:1107–8
FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and other Tools) Resource. Silver Spring (MD): Food and Drug Administration (US); Bethesda (MD): National Institutes of Health (US), www.ncbi. nlm.nih.gov/books/NBK326791/ (2016, accessed 22 September 2017)
US Food and Drug Administration. Center for Drug Evaluation and Research. Summary Review. Scientific dispute regarding accelerated approval of Sarepta Therapeutics’ eteplirsen (NDA 206488) – Commissioner’s Decision. September 16, 2016, www.accessdata.fda. gov/drugsatfda_docs/nda /2016/206488_summary%20review_ Redacted.pdf (accessed 27 September 2017)
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.