Impacts of oxygenation goals on organ dysfunction in critically ill patients
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
- New Ocrevus Subcutaneous Injection Therapy Shows Promising Results in Multiple Sclerosis Treatmen
- Dutch Man Infected with COVID-19 for 613 Days Dies: Accumulating Over 50 Virus Mutations
JAMA: Impacts of oxygenation goals on organ dysfunction in critically ill patients
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
JAMA: Impacts of oxygenation goals on organ dysfunction in critically ill patients. Oxyemia may also have antibacterial effects.
Oxygen is one of the important factors for maintaining life, and the treatment of critically ill patients is ultimately to maintain the oxygen and blood supply of the body’s cell metabolism.
However, is it more beneficial to give higher oxygen in the treatment of critically ill patients? Observational studies from 1999 to 2006 showed that PaO2 had a U-shaped relationship with mortality, which triggered a debate about the optimal oxygenation goal for critically ill patients.
Potential negative effects of hyperoxaemia include lung toxicity, systemic vasoconstriction and reduction of organ perfusion, and aggravate ischemia/reperfusion injury.
On the other hand, hyperoxemia may reduce the vasodilation caused by systemic inflammatory response syndrome (SIRS) through systemic vasoconstriction, which is conducive to the redistribution of blood flow. In addition, hyperoxemia may also have antibacterial effects.
In view of the inconsistent results of the existing RCT studies, as well as the bias of the research and the design flaws of the research objectives, the Angelique de Man team at the University of Amsterdam Medical Center in the Netherlands conducted a multi-center randomized clinical trial to clarify the difference with the higher normal PaO2 Compared with the target, whether the lower normal PaO2 target can alleviate the organ dysfunction in critically ill patients with SIRS. The research was published in JAMA on September 14, 2021.
Methods:
Patient inclusion criteria: ①Age ≥18 years old and admitted to ICU; ②Expected hospital stay ≥48h; ③Meet at least two or more SIRS diagnostic criteria.
Exclusion criteria: patients admitted for surgery; pulmonary hypertension grade III or IV; severe acute respiratory distress syndrome; pregnancy; severe chronic obstructive pulmonary disease; refusal of tracheal intubation; carbon monoxide or cyanide poisoning or methemoglobinemia; sickle cell disease ; The heart shunts from right to left.
Randomization: Patients are screened immediately upon admission, and eligible patients are randomly assigned to the low-normal or high-normal PaO2 target range group.
Stratified by age, gender, and reason for admission (medical, surgical, or trauma). By inhaling oxygen to ensure that the PaO2 of each group is maintained within the corresponding range, the target of low normal PaO2 is 8~12kPa (60~90mmHg), and the target of high normal PaO2 is 14~18kPa (105~135mmHg).
For mechanically ventilated patients, the target PaO2 is achieved by adjusting FiO2 and positive end expiratory pressure (PEEP). Unless otherwise specified in the clinic, the maximum value of FiO2 is 0.60, and the maximum value of PEEP is 10cmH2O.
From the perspective of clinical treatment, prone position ventilation can be performed on the patients in need, and the mask oxygen can be changed to non-invasive mechanical ventilation or tracheal intubation. Temporary measures to increase oxygenation during treatment include tracheotomy and bronchoscopy.
All participating hospitals draw arterial blood samples in accordance with routine clinical practice. When the patient’s PaO2 is not within the target range, adjust the oxygen supply, and collect an arterial blood sample 15 minutes later to check whether the patient is within the target range.
The intervention started within 12 hours of entering the ICU and continued until the 14th day, before ICU discharge or death. Calculate PaO2, arterial oxygen saturation (SaO2), SpO2 and FiO2 time weighted values.
The primary endpoint is SOFARANK, which is a graded result of non-respiratory organ failure, quantified by the non-respiratory component of the sequential organ failure assessment (SOFA) score, and aggregated in the first 14 study days. The SOFARANK score is a comprehensive reflection of organ failure, mortality and 14-day discharge.
The secondary endpoint includes the results derived from the other 3 SOFA scores as a sensitivity analysis for the design choice of the primary endpoint. The secondary SOFA score endpoints were non-respiratory SOFA score, non-respiratory SOFA score minus baseline score, and non-respiratory SOFA score decline rate.
Adverse events include: myocardial infarction during admission to the ICU (new-onset), stroke during admission to the ICU, renal replacement therapy required for more than 24 hours after admission to the ICU, prone position ventilation, and severe liver failure (new-onset).
Results
In the end, a total of 400 patients were enrolled in the study, of which 205 cases and 195 cases were enrolled in the lower normal PaO2 group and the higher normal PaO2 group, respectively.
The median PaO2 difference between the two groups was -1.93 kPa (14.475mmHg) (Figure 1) The median SOFARANK score of the lower normal PaO2 group was 35 points, while the PaO2 higher normal group was 40 points, the difference between the groups Not significant (Figure 2)
The median mechanical ventilation time of the two groups of patients was 3.4 days and 3.1 days, respectively, and the in-hospital mortality rate was 32% and 31%, respectively, and there was no statistically significant difference between the groups.
The incidence of mild hypoxemia in the low-normal PaO2 group was 1.9%, which was significantly higher than that in the high-normal PaO2 group (1.2%). Acute renal failure occurred in 20 cases (10%) in the lower normal PaO2 group, and 21 cases (11%) in the higher normal PaO2 group.
Acute myocardial infarction occurred in 6 cases (2.9%) in the lower normal PaO2 group, and 7 cases (3.6%) in the higher normal PaO2 group.
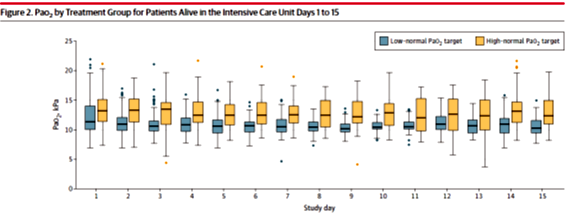 Figure 1 PaO2 values of the two groups of patients in the ICU
Figure 1 PaO2 values of the two groups of patients in the ICU
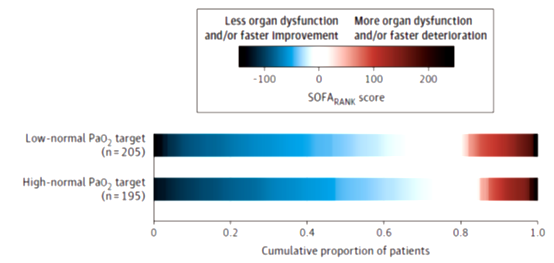
Figure 2 SOFARANK scores of the two groups of patients
Conclusion:
Among critically ill patients who met 2 or more SIRS criteria, compared with patients in the higher normal PaO2 target group, the incidence of organ dysfunction in the lower normal PaO2 target group did not significantly decrease.
Expert Reviews & Comments:
During the First World War, Haldane successfully treated chlorine poisoning with oxygen, and oxygen inhalation became an important treatment for critically ill patients. However, any substance that enters the human body and produces effects can be considered a drug, and drugs must have side effects.
Therefore, more and more studies believe that oxygen therapy is a double-edged sword. Excessive oxygen therapy brings different degrees of adverse reactions and damages to patients with different conditions, which should arouse widespread attention and require in-depth research and summary in combination with clinical practice.
Retinopathy of prematurity, chronic lung disease, and nervous system damage caused by improper neonatal oxygen therapy have long been reported.
Simply increasing the inhaled oxygen concentration and continuous FiO2>70% for a long time can increase pulmonary complications. In recent years, the “less is more” strategy believes that low-level treatment measures may be more beneficial.
Clinical studies on oxygen therapy either believe that the results of the low-normal PaO2 group are more favorable, or that there is no significant difference between the low-normal oxygenation group and the high-normal oxygenation group.
The Oxygen-ICU trial was stopped due to ethical factors after 434 patients were enrolled. At that time, the mortality rate of patients in the hypoxia group was significantly reduced.
In the HYPERS2S trial, mechanically ventilated patients with sepsis were randomly assigned to the 100% oxygen group (hyperoxemia group) or 88%-95% SpO2 group.
Due to the high mortality of patients in the hyperoxemia group, they stopped prematurely (Oxygen -ICU clinical trial: 20.2% vs 1.6%; HyperS2S clinical trial 43% vs 35%).
Two other randomized controlled trials did not find a significant difference in mortality between hypoxic and hyperoxic groups.
The ICU-ROX trial randomly assigned 965 mechanically ventilated patients to different SpO2 oxygenation target groups, and found no significant difference in the number of days without ventilator and survival rate.
The HOT-ICU trial randomly selected 2928 critically ill patients with acute hypoxic respiratory failure, with a goal of PaO2 of 8-12kPa (60-90mmHg).
In the population with an average baseline of FiO2 of 70% and an oxygenation index of PaO2:FiO2 of 120 mmHg, there was no significant difference in mortality between different oxygenation groups.
In the LOCO2 test conducted in ARDS patients, the target oxygenation was 7.3-9.3kPa and 12-14kPa, and it was stopped early due to 5 cases of mesenteric ischemia in the hypoxic group.
At this time, the 90-day mortality rate of patients in the hypoxia group was significantly increased. However, the larger HOT-ICU trial did not find differences between serious adverse events.
Recent clinical studies on the effect of inhaled oxygen concentration on postoperative NT-proBNP and myocardial injury in patients undergoing major abdominal surgery during perioperative period suggest that 30% or 80% inhaled oxygen concentration during anesthesia surgery is effective for patients with high risk of cardiovascular events after surgery.
There was no significant difference in the effects of NT-proBNP or myocardial injury index troponin, and there was no significant effect on the 30-day mortality rate or the incidence of adverse events.
The results of this trial on critically ill patients with systemic inflammatory response syndrome showed that compared with the low-normal group, the improvement rate of non-respiratory organ failure in the target group with high normoxia increased, but this difference was not statistically significant .
The improvement of organ function in the target group of hyperoxia may be related to the increase of oxygen delivery at the tissue level. In addition, the systemic vasoconstriction induced by hyperoxemia may counteract the vasodilation induced by SIRS, thereby allowing better redistribution of blood.
Limiting FiO2 to 60% may minimize the pulmonary toxicity caused by excessive oxygen concentration. The most important feature of the study is the design of the primary endpoint (SOFARANK), which is the grading result of non-respiratory organ failure, which is quantified by the non-respiratory component of the sequential organ failure assessment (SOFA) score, which is organ failure, mortality and 14-day discharge Comprehensive reflection of the situation.
It is worth adding that neither the partial pressure of blood oxygen nor the saturation of pulse oxygen can truly represent the oxygen supply of the tissues.
Only when sufficient perfusion is ensured, these indicators can represent the oxygen supply of the organs and tissues.
The ultimate goal of oxygen therapy is to ensure oxygen supply to tissues and organs, and related research still needs to be further in-depth.
Impacts of oxygenation goals on organ dysfunction in critically ill patients
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



