What’s the research progress of mRNA vaccines for infectious diseases?
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
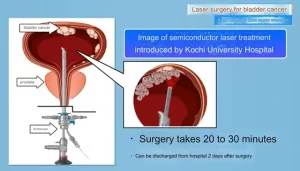
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
What’s the research progress of mRNA vaccines for infectious diseases?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What’s the research progress of mRNA vaccines for infectious diseases?
mRNA-based treatments represent a relatively novel and highly effective class of drugs. Several recently published studies have emphasized the potential efficacy of mRNA vaccines in the treatment of different types of malignant tumors and infectious diseases, where traditional vaccine strategies cannot elicit a protective immune response.
Infectious disease vaccines are currently the leading application of mRNA therapy. Most mRNA vaccines currently undergoing preclinical trials and clinical use are injected into the skin, muscle or subcutaneously in a single dose, where they are absorbed by immune or non-immune cells and converted into antigens, which are displayed to T cells And B cells.

As of the end of 2019, 15 candidate mRNA vaccines for infectious diseases have entered clinical trials. At that time, it was believed that it would take at least 5-6 years for mRNA vaccines to obtain regulatory approval. But when the COVID-19 pandemic hit the world in early 2020, these expectations were subverted.
In the next few months, the development, manufacturing and deployment of mRNA vaccines have entered a stage of rapid leapfrogging.

SARS-CoV-2 vaccine
Most SARS-CoV-2 vaccine candidates produce an immune response to the spike protein on the surface of the virus. The spike protein binds to the receptor angiotensin converting enzyme 2 on the surface of its host cell. Then, the cell’s transmembrane serine protease 2 cleaves the attached spike protein. The protease induces a conformational change, exposes the fusion peptide of the spike protein and promotes fusion with the cell or endosomal membrane. Generally, the antigen encoded by vaccine mRNA is either the full-length spike protein or the receptor binding domain of the spike protein.

As of June 18, 2021, 185 CVID-19 vaccine candidates are in the preclinical development stage, and another 102 have entered clinical trials. In clinical trials, 19 are mRNA vaccines. On December 11, 2020, Pfizer’s BNT162b2 vaccine received emergency authorization from the FDA and became the first mRNA drug approved for use in humans. A week later, Moderna vaccine mRNA-1273 was also authorized for use in the United States. In the end, they were the first SARS-CoV-2 vaccines authorized in the United States, the United Kingdom, Canada and several other countries.
Pfizer and BioNTech have jointly developed five mRNA candidate vaccines, which encode variants of the spike protein antigen. The two main drug candidates BNT162b1 and BNT162b2 use Acuitas Therapeutics’ ionizable lipid ALC-0315 and nucleoside modified mRNA, in which all uridines are replaced by N1 methyl pseudouridine to enhance mRNA translation. BNT162b1 encodes the receptor binding domain of the trimeric secreted spike protein, while BNT162b2 encodes the full-length SARS-CoV-2 spike glycoprotein, with two proline substitutions in the S2 subunit, locking the protein in the pre-fusion conformation .
In the first phase test of the two vaccines, high titers of neutralizing antibodies can be induced, and strong CD4+ and CD8+ reactions are produced, accompanied by mild to moderate adverse reactions. The two candidate vaccines are well tolerated and effective, but only the BNT162b2 vaccine entered the phase II/III trial due to its milder systemic and local adverse reactions. In the third phase of the trial, BNT162B2 showed 95% overall prevention and 90-100% efficacy.
Moderna developed mRNA-1273 in cooperation with the National Institutes of Health. The vaccine uses the ionizable lipid SM-102 to prepare LNP, which encapsulates N1 methylpseudouridine-modified mRNA. This sequence encodes the SARS-CoV-2 spike protein, with two proline substitutions, giving it a pre-fusion conformation.
In phase 1 clinical trials, mRNA-1273 was very effective and well tolerated. In a phase III trial involving 30,420 volunteers, the prevention rate of two 100μg doses of vaccine was 94.1%, and local pain at the injection site was the most common side effect. After the second dose, half of the volunteers reported moderate to severe systemic side effects (such as fatigue, muscle pain, joint pain), and these side effects disappeared within 48 hours.
Although the vaccines produced by Pfizer and Moderna have proven to have good efficacy and safety, their demand for cold chain storage has brought huge difficulties to guarantee. mRNA-1273 can be stored at 4-8°C for one month, while BNT162b2 needs to be stored at -60°C.
CureVac’s candidate vaccine CVnCoV can be stored stably for 3 months at 5°C. CVnCoV uses ionizable lipids from Acuitas Therapeutics (probably ALC-0315) and unmodified mRNA encoding a full-length spike protein with two proline substitutes. In the first phase of clinical trials, the neutralizing antibodies produced by volunteers were similar to those of CVID-19 convalescent patients and were well tolerated. Unfortunately, in a phase III clinical trial involving 40,000 people, CVnCoV only showed 47% efficacy. The interim analysis showed that the lower efficacy of CVnCoV was attributed to the emerging SARS-CoV-2 mutation.
Currently, CureVac is cooperating with GSK to develop the second-generation drug candidate-CV2CoV, which has been optimized to enhance translation and immunogenicity relative to CVnCoV. CV2CoV uses the 5’UTR from the human hydroxysteroid 17-β-dehydrogenase 4 gene and the 3’UTR from the human proteasome 20S subunit β3 gene. In preclinical studies, CV2CoV showed 1.8 times higher protein expression than CVnCoV in vitro, and induced B. coli in rats. 1.1.7, B. 1.1.298 and B. 1. High-titer cross-neutralizing antibodies of the 351 variant.
Another heat-resistant vaccine candidate, ARCoV, was developed by the Chinese People’s Liberation Army Military Science Academy in cooperation with Walvax Biotechnology Company, and can be stable for one week at 25°C. ARCoV encodes the receptor binding domain of the spike protein. In preclinical studies, high SARS-CoV-2 specific IgG antibodies and strong virus neutralization titers can be induced in cynomolgus monkeys. Although the reasons behind the thermal stability of CVnCoV and ARCoV are unclear, mRNA secondary structure, smaller mRNA size, GC content, and lipids may be important factors.
Some other mRNA vaccine candidates are also under development. LNP-nCoVsaRNA was jointly developed by Imperial College London and Acuitas Therapeutics, and encodes a full-length spinous protein. Currently, a 0.1–1?g dose escalation protocol is being used for phase I clinical trial evaluation (ISRCTN17072692), which uses the lowest RNA dose among all candidate mRNA vaccines.
Another self-amplifying mRNA vaccine candidate ARCT-021 (also known as LUNAR-COV19) was developed by Arcturus using its proprietary LUNAR lipid carrier and self-transcribing and replicating RNA (STARR) platform. It encodes the full-length fusion prespinous protein.
Influenza virus vaccine
Approximately 290,000 to 650,000 people die from influenza viruses worldwide each year. Current vaccines target the viral hemagglutinin protein that promotes virus entry. The traditional flu vaccine is an inactivated flu virus grown in eggs, which takes a long time to produce and is difficult to purify. In addition, viruses mutate in eggs for optimal growth, sometimes rendering them ineffective in humans.

Therefore, there is indeed a need for alternative antigen targets and production methods. Synthetic mRNAs transcribed in vitro can meet this need and ensure rapid production of vaccines when new influenza strains emerge. For example, in 2013, a self-amplified mRNA vaccine based on LNP (DLinDMA) was quickly developed within 8 days after the outbreak of H7N9 in China. Unfortunately, because there were no GMP facilities for mRNA manufacturing at that time, clinical trials could not be conducted.
There are also efforts to develop a universal flu vaccine that does not need to be revised every year. This vaccine can produce immunity to several influenza virus strains and subtypes. In the influenza mRNA vaccine shown for the first time in 2012, three intradermal injections induced homologous and heterologous immunity against H1N1 and H5N1 strains in mice, respectively.
It is worth noting that the conservative handle region of hemagglutinin, which is not prone to mutation, has recently become a new universal vaccine target. Another study used LNPs to deliver 50 ng of mRNA, encoding three conserved influenza proteins: neuraminidase, nucleoprotein and matrix-2 ion channel protein, and hemagglutinin handle. Incredibly, this tiny dose of mRNA produces a wide range of protective antibodies.
Zika virus vaccine
Zika virus infection was first discovered in 1947. Patients infected with Zika virus are usually asymptomatic or have mild symptoms such as fever, rash, and muscle pain. However, Zika virus became a global health crisis during the 2015-2016 pandemic in the Americas. The virus caused severe fetal neurological malformations and fetal death during pregnancy. Membrane and envelope protein (prM-E) is a common antigen choice for mRNA vaccines against Zika virus, because neutralizing antibodies against prM-E can prevent virus fusion.

Moderna collaborated with the University of Washington School of Medicine to develop an improved prM-E mRNA that contains a mutant fusion ring epitope in the E protein. Two 10 μg doses of mRNA can protect mice from Zika virus attack and reduce the production of dengue-enhancing antibodies. These encouraging pre-clinical results promoted the progress of the phase I trial. The mid-term results showed that the vaccine mRNA-1893 induced 94-100% of seroconversion within 10 days and was well tolerated.
In addition, another study used passive immunization methods, using squalene-based nanocarriers to deliver mRNA encoding ZIKV neutralizing antibodies. This is an attractive method for immunodeficiency patients whose immune system is impaired and unable to synthesize autoantibodies.
HIV virus vaccine
Globally, HIV currently affects 38 million people and is expected to affect as many as 42 million people by 2030. Despite 30 years of research, an effective vaccine has not yet been developed. This is mainly because the HIV envelope protein has significant antigenic diversity and hides the key envelope protein epitope “glycan barrier”.
Several preclinical studies have used a variety of carriers, including cationic nanoemulsions, DOTAP/DOPE liposomes, Polymers, and ionizable LNP, and they have seen some effects in varying degrees. These studies show that in addition to effective carriers, new antigens are very critical for effectively targeting HIV.

Respiratory syncytial virus vaccine
Respiratory syncytial virus is the main cause of acute lower respiratory tract infections worldwide. Every year, an estimated 60,000 children under the age of 5 die, and more than 14,000 people over the age of 65 die.

The current RSV vaccine candidates mainly target the highly conserved F protein. Although some candidates failed to pass clinical trials due to insufficient neutralizing antibody titers, new findings on the F protein conformation showed that vaccination against the pre-fusion conformation can produce an excellent neutralizing antibody response. This discovery is expected to improve future vaccine design.
Moderna is evaluating three single-dose vaccine candidates that encode pre-fusion F protein: mRNA-1172 and mRNA-1777 for adults, and mRNA-1345 for children. In phase I clinical trials, mRNA-1777 induced a strong humoral response to RSV neutralizing antibodies, and CD4 + T cells responded to RSV F protein without serious adverse events.
The sequence of mRNA-1345 has been further designed and codon optimized to enhance translation and immunogenicity relative to mRNA-1777. One month after vaccination, the neutralizing antibody titer produced by mRNA-1345 is about eight times that of mRNA-1777.
Ultimately, Moderna’s goal is to integrate mRNA-1345 with its pediatric human metapneumovirus/parainfluenza virus type 3 (hMPV/PIV3) candidate vaccine mRNA-1653, and use a single formulation to vaccinate children against three different pathogens.
Ebola virus vaccine
Ebola virus (EBOV) was first identified as the causative agent of Ebola disease in 1976. This viral hemorrhagic fever killed more than 11,000 lives in the 2014-2016 Ebola epidemic in West Africa. In 2019, the FDA approved an Ebola vaccine (rVSV-EBOV) based on recombinant vesicular stomatitis virus (VSV).
Although the effectiveness of rVSV-EBOV in preventing the spread of Ebola is 97.5% compared with unvaccinated, clinical trials have noted some safety issues (such as acute arthritis and skin rash).

Anti-EBOV mRNA vaccines may be safer than this virus-based vaccine because they will not replicate in the body. An mRNA vaccine encoding EBOV glycoprotein has proven efficacy in mice. The vaccine induces strong expression of glycoprotein-specific IgG antibodies, IFN-γ and IL-2 through CD8+ and CD4+ T cells, which can protect animals from deadly viruses.
Rabies virus vaccine
Rabies is a zoonotic disease characterized by neurological symptoms and a mortality rate of nearly 100%. Although the vaccine has been approved, more than 50,000 people still die from rabies each year, highlighting the need for more effective and cheaper vaccines.

In order to meet this demand, CureVac used its RNActive platform to screen the unmodified mRNA vaccine CV7201 that encodes the glycoprotein of rabies virus. In a preclinical study, CV7201 can induce high neutralizing antibody titers in mice and pigs, and induce antigen-specific CD4+ and CD8+ T cell responses.
However, in the Phase I clinical trial, it was found that although the route of administration does not affect the immune response, the drug delivery device only has an intradermal syringe to produce a short-term humoral immune response. This weak drug delivery effect and high incidence of adverse events indicate that the drug delivery platform needs to be further optimized.
Subsequently, CureVac used the proprietary LNP produced by Acuitas Therapeutics as the carrier for its new vaccine CV7202. In a preclinical study, CV7202 induced strong antibody titers and CD8+ and CD4+ T cell responses. The results of phase I clinical trials showed that two 1?g doses can produce high titers of neutralizing antibodies and a strong adaptive immune response, which is well tolerated.
Plasmodium vaccine
Although the vast majority of mRNA vaccines under development are to prevent viral infections, there are also efforts to prevent other infectious diseases. Malaria is caused by a single-celled eukaryotic parasite, and its morbidity and lethality ranks first.
Every year, malaria afflicts more than 200 million people around the world and takes the lives of more than 400,000 patients. Due to the lack of surface antigens and the complex life cycle of Plasmodium, the production of anti-malarial vaccines has been difficult.
Fortunately, research on the human body’s natural immune response to Plasmodium infection has identified potential non-surface antigen targets.

For example, the cytokine macrophage migration inhibitory factor (PMIF) secreted by malaria parasites has been shown to prevent T cells from producing long-term memories. Based on this discovery, a vaccine was prepared from a cationic nanoemulsion based on squalene loaded with self-amplifying mRNA encoding PMIF. Two 15?g doses can improve the development of helper T cells and induce anti-Plasmodium IgG antibodies and memory T cell responses.
Another study on the mechanism of malaria infection found that Plasmodium falciparum glutamate-rich protein (PfGARP) is a potential mRNA vaccine target. A nucleoside modified mRNA vaccine encoding the PfGARP antigen is under development. The vaccine uses Acuitas Therapeutics’ proprietary LNP. Preclinical studies have shown that the vaccine can reduce the response of animals infected with Plasmodium.
Reference: What’s the research progress of mRNA vaccines for infectious diseases?
1. mRNA vaccines for infectious diseases:principles, delivery and clinical translation. Nat RevDrug Discov. 2021 Aug 25 :1–22.
What’s the research progress of mRNA vaccines for infectious diseases?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.