First real-world data on HPV vaccination: Incidence rate reduced up to 87%!
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
- New Ocrevus Subcutaneous Injection Therapy Shows Promising Results in Multiple Sclerosis Treatmen
- Dutch Man Infected with COVID-19 for 613 Days Dies: Accumulating Over 50 Virus Mutations
First real-world data on HPV vaccination: Incidence rate reduced up to 87%!
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
The First real-world data on HPV vaccination: Incidence rate reduced up to 87%! The sooner women get vaccinated, the better.
HPV, or human papillomavirus, is the most common sexually transmitted virus in the world. HPV infection is usually silent. Although most infections can be cleared, some are chronic and may cause oral cancer, throat cancer, and cervical cancer. Cervical cancer is one of the most common gynecological malignancies, and the number of cases and deaths are both ranked fourth among female cancers.
In addition, HPV can also cause genital warts and anal cancer. Among them, HPV6 and HPV11 cause about 90% of genital warts, and HPV16 and HPV18 cause about 70% of cervical cancer and anal cancer. Therefore, both men and women may be infected with HPV.
New HPV infections can be prevented with reliable and safe vaccines. If the infection is detected early and treated in time, it can also be cured.
On November 3, a real-world data published in the authoritative medical journal “the Lancet” showed that the incidence of cervical cancer among women vaccinated with HPV in England has plummeted. The study was led by King’s College London and Public Health England.
First real-world data on HPV vaccination: Incidence rate reduced up to 87%!
According to previous data, the number of new cases of cervical cancer worldwide in 2020 is about 604,000, and the death toll is about 342,000.
In November 2020, the World Health Organization launched the “Global Strategy to Accelerate the Elimination of Cervical Cancer,” and 194 countries pledged to eliminate this cancer for the first time.
This new study provides the first direct evidence from the real world on the impact of the bivalent (Cervarix) HPV vaccine on the incidence of cervical cancer.
In September 2008, England introduced the bivalent vaccine (Cervarix) HPV vaccination program. Regular vaccination is provided to girls aged 12-13, and supplementary vaccination is not provided to women aged 14-18. The researchers quantified the early impact of the immunization program on cervical cancer and precancerous lesions (cervical carcinoma in situ and cervical intraepithelial neoplasia).
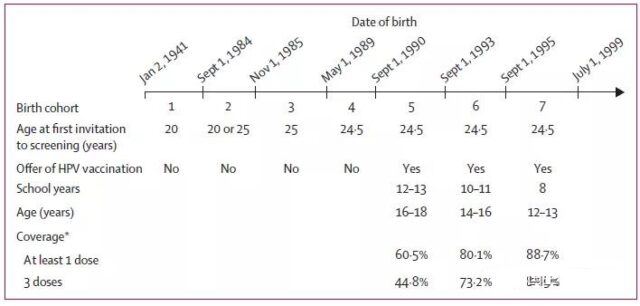
They evaluated the diagnostic data of cervical cancer and cervical precancerous lesions in women aged 20-64 who lived in England between January 1, 2006 and June 30, 2019.
Researchers found that the rate of cervical cancer and precancerous lesions decreased the most among the youngest women vaccinated.
Specifically, compared with the control cohort not vaccinated with HPV vaccine, the incidence of cervical cancer vaccinated at 12-13 years old was reduced by 87%; at 14-16 years old, the incidence of cervical cancer was reduced by 62%; at 16-18 years old The vaccination was reduced by 34%.
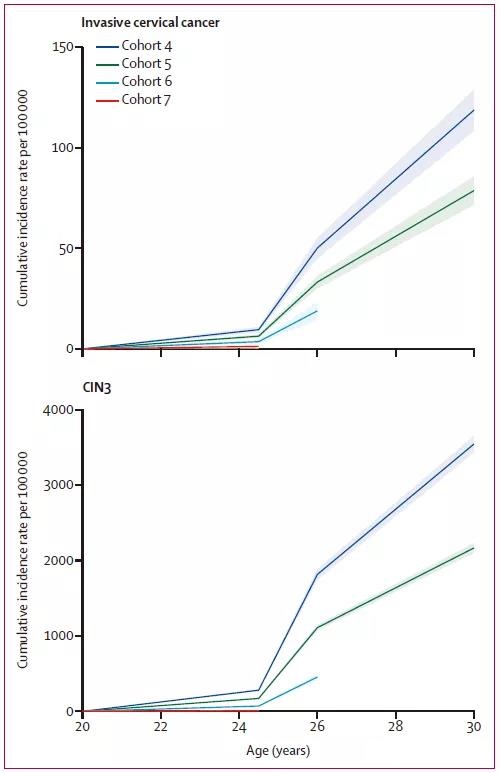
Researchers said that the HPV vaccination program almost eliminated cervical cancer in women born after September 1, 1995.
The author of a review article published in the same period pointed out that although this new study seems to support the widespread use of HPV vaccines, there are still problems with the vaccination and availability of HPV vaccines.

Authors Maggie Cruickshank and Mihaela Grigore wrote: “Even in developed countries like the United Kingdom where HPV vaccination is free, the vaccination rate has not reached the WHO target of 90% for 15-year-old women. Moreover, The COVID-19 epidemic is another challenge that has led to the supply of HPV vaccines. Not only that, but there are also a series of challenges, including access to affordable vaccines, low-temperature control supply chain infrastructure required for vaccines, delivery, and waste disposal.”
The author also pointed out some limitations, including that cervical cancer rarely appeared in the under-25 age group investigated in the study. Because even in the absence of a vaccine, the incidence of people under the age of 25 is very low.
Paper link:
https://doi.org/10.1016/S0140-6736(21)02178-4
https://doi.org/10.1016/S0140-6736(21)02396-5
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



