Fierce argument: Organ donation from died COVID-19 patients
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
- New Ocrevus Subcutaneous Injection Therapy Shows Promising Results in Multiple Sclerosis Treatmen
- Dutch Man Infected with COVID-19 for 613 Days Dies: Accumulating Over 50 Virus Mutations
Fierce argument: Organ donation from died COVID-19 patients
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Fierce argument: Organ donation from died COVID-19 patients.
After the death of the COVID-19 patient, two people were saved by donating kidneys, but why the experts quarreled?
If your life is hanging by a thread and an organ transplant is urgently needed, at this time there happens to be an organ matching successfully, but the organ donor is a confirmed patient with COVID-19, would you accept it?
In May of this year, a woman in her 50s in Los Angeles, USA, committed suicide more than a year after being diagnosed with the COVID-19 due to her unbearable condition.
She signed an organ donation agreement before her death.
Currently, 2 patients with end-stage renal disease have received kidney transplants from this donor.
This incident has triggered a debate among medical experts. Some people oppose transplantation and believe that there is no effective treatment for the COVID-19 and that such dangerous organs should not be transplanted to patients; some people support transplantation and believe that the donated organs are so precious, as long as the risk of infection is not High can be used.
So, how should we treat the organs donated by COVID-19 patients?
Objection: Transplanting organs from patients with COVID-19 can spread the virus
The incident mentioned at the beginning has aroused opposition from many professionals. In an interview with the New York Times, Dr. Zijian Chen, medical director of the COVID-19 Rehabilitation Care Center, said that if the organs of COVID-19 patients are used, the virus is likely to spread to the recipients.
This is also the most worrying issue for most opposition experts.
In May 2020, a paper that brought together opposing views mentioned that the new coronavirus may be transmitted through organ transplantation in two ways: one is transmission through blood, and the other is direct transmission through transplanted organs.
 “Arguments against the use of organs from COVID-19 positive donors”
“Arguments against the use of organs from COVID-19 positive donors”
Source: Reference [2]
The COVID-19 virus will be present in the blood of people infected with the COVID-19. Viremia occurs in 15% of severely infected patients, and complete viral RNA may also be present in asymptomatic infections.
This means that the virus may enter the donor’s organs through the blood, and then enter the recipient’s body through the organ transplant, and infect the recipients of these organs.
In addition, the virus is also present in the organs of patients with COVID-19. The main target of the new coronavirus is the angiotensin-converting enzyme (ACE-2) receptor, which is mainly found in the vascular endothelial cells and vascular smooth muscle cells of the lung, and its expression in the lung is more dense than other tissues.
It is also present in the epithelial cells of the bile duct, heart, intestine and kidney, so these tissues may also carry virus particles.
In other words, transplanting these organs may bring the virus directly into the recipient’s body.
At the same time, due to the infectious characteristics of the new coronavirus, its content distribution in different organs is also different.
The lungs of patients with COVID-19 have the highest virus content, followed by the kidneys. Other organs such as liver, pancreas, and heart contain less virus, but they do exist.
German scientists conducted autopsies on 27 patients who died of the COVID-19 and found that more than 60% of the dead contained the COVID-19 virus in their kidneys and heart tissues; one A retrospective study of patients recovering from COVID-19 showed that 6.9% of patients had COVID-19 in their urine; a study showed that 30% of patients with COVID-19 found the virus during endocardial biopsy.
The difference in the amount of virus in each organ may be related to the risk of transplantation.
Many studies have proved that the risk of lung transplantation is far greater than that of non-lung organs.
Fifteen asymptomatic or mildly infected people with replicated new coronaviruses donated a total of 25 non-pulmonary organs (16 kidneys, 6 livers and 3 hearts).
After transplantation, only 25 recipients One case of COVID-19 infection occurred, and the donor in this case was the recipient’s mother.
It is difficult to judge whether the COVID-19 virus was spread before surgery or through an organ transplant.
The presence of two body complex system of infected with COVID-19 donated his lung and transplanted into the body of the recipient.
The donor’s nucleic acid test before organ donation was false negative, so these two lungs at risk of infection were not intended to be transplanted to the recipient.
The two recipients of postoperative respiratory failure, we can see, should try to avoid the presence of transplanted within the complex system of lung infection of the virus of the COVID-19.
In addition to the infection risk of organ recipients, the opposing views also believe that the current knowledge about the COVID-19 is limited, doctors cannot provide clear guidance to recipients, and it is difficult for patients to give effective informed consent on the basis of full understanding.
In addition, in the process of organ transplantation of patients with COVID-19, because the COVID-19 virus can survive on the surface of the object for several hours, it is likely to increase the risk of infection by medical staff.
Support: The risk of cured patients with COVID-19 disease is small
Although transplanting the organs of patients with COVID-19s faces many risks, there are still many experts who support transplantation because the organs are too scarce.
In an interview with the New York Times, Dr. Glenn Franklin, a medical consultant of the American Organization for Organ Acquisition (AOPO), said that in the early stage of the COVID-19 epidemic in the United States, patients with COVID-19s were not allowed to donate organs, but this attitude has now changed.
The main reason was the severe shortage of organs during the epidemic. The number of organ donors and organ transplant operations dropped sharply during the COVID-19 pandemic in the United States.
Compared with the same period in 2019, the number of donors from March to May of 2020 decreased by 11%; compared with 2019, the number of transplants in 2020 The total number of organs has been reduced by 17%.
Every day, 17 people in the United States die while waiting for their organs, which makes people have to start thinking about using organs donated by COVID-19 patients.
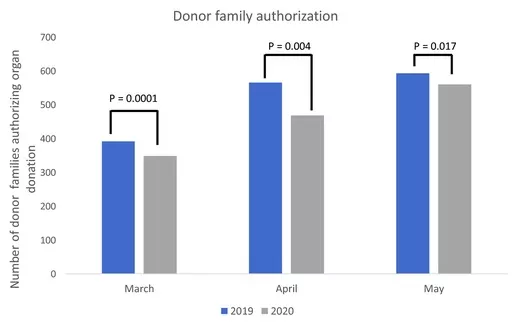
Comparison of the number of donors from March to May 2019 and the same period in 2020 ( Source: Reference [7])
The support experts pointed out that the current information shows that the risk of spreading the virus from organs donated by patients who have recovered from the COVID-19 is small.
The results of non-lung organ transplants donated by COVID-19 patients are very good. A literature analysis of multiple case reports showed that 55 COVID-19 survivors had donated their non-pulmonary organs (including 45 kidneys, 14 livers, and 6 hearts), and their median number of organ donations from the diagnosis of COVID-19 to the The duration was 54 days, of which only one donor had symptoms, and all the other donors were asymptomatic or mildly infected. The organs they donated were successfully transplanted, and none of them caused symptomatic COVID-19 infections in the organ recipients.
However, of these 65 recipients, 18 have had the COVID-19 or vaccinated against the COVID-19, and its impact cannot be ruled out.
Among the non-pulmonary organs donated by COVID – 19 survivors , kidney transplantation, which has a relatively high risk of infection, has also been successful.
A document summarized 31 cases of kidney transplantation from COVID-19 recovery donors.
The results showed that the transplant success rate and patient survival rate were 100%, the acute cell rejection rate was only 6.4%, and the median serum creatinine was 1.0 mg/dL.
No delay in the recovery of transplanted kidney function occurred.
There were only 3 cases of lung transplantation with the highest risk of infection, and no virus transmission occurred. The donors tested negative for COVID-19 at 3 months, 90 days, and 49 days before donation. After lung transplantation, the recipients tested negative for COVID-19. However, 2 of these 3 recipients have been infected with the new coronavirus and may have a certain degree of immunity.
As a result, the support experts believe that in the context of organ shortage, using organs donated by recovered patients with COVID-19s has more advantages than disadvantages.
However, although these transplants have achieved good results, we are still unable to answer the most critical question: How long will it take for patients with COVID-19 disease to recover before they can guarantee that their organs are not at risk of spreading the virus?
Due to limited knowledge of the COVID-19, the answer is currently unknown. Moreover, within a certain period of time after the recovery of the COVID-19, the positive nucleic acid results of asymptomatic patients are likely to represent the continued removal of viral RNA, rather than viral replication or new infections. This makes the judgment of the time interval more confusing.
The debate between the pros and cons is still going on, so how do countries deal with this issue in reality?
The American Organ Donation Association has developed a more detailed solution. In the “American Society of Transplantation |(AST) Recommendations and Guidance for the Evaluation of Organ Donors”, for donors who have had COVID-19, consider accepting their organs under the following circumstances:
- Donors whose COVID-19 symptoms have been relieved for 21 days (among them, asymptomatic and mildly ill patients can be shortened to 10 to 14 days when facing a super-urgent transplant);
- Patients whose symptoms are relieved 21 to 90 days after the diagnosis of COVID-19 but whose nucleic acid is still positive.
- Non-lung transplantation can be performed for donors who have undergone nucleic acid testing more than 90 days after the initial infection, but the potential risks, recovery ability, medical conditions, and the urgency of transplantation must be considered.
In addition, the “Recommendations and Guidance” emphasizes that the use of organs from donors with active neocoronavirus in the body should be avoided; the acquisition of organs from asymptomatic donors with a history of neocoronavirus exposure within 14 days should be postponed; in view of the kidney function related to neocoronavirus infection The barriers and their long-term effects are not yet known and need to be evaluated separately when a kidney transplant is performed.
The United States once conducted a relatively successful practice on this issue.
In October 2020, a number of scholars and doctors in Texas formulated a set of very detailed standards to classify the exposure of donors, the clinical risk of donors, the exposure risk of transplant recipients, and the clinical risk of transplant recipients. Evaluate and discuss the situation of different organs to reach the best match between donors and recipients.
Within 2 months of implementing this standard, they performed 7 heart transplants (including 1 cardiopulmonary and 1 heart/kidney patient), 3 lungs, 2 kidneys, and 15 liver transplants. 100% of the recipients survived , And none of them were infected with the new coronavirus.
However, in the world, there are still a few countries that accept organ donations from COVID-19 patients. In December 2020, organ donation associations in 19 countries issued position statements on the use of organs donated by COVID-19 patients.
Among them, 16 associations strongly recommend avoiding the use of organs from donors who test positive for COVID-19 or are at high risk of infection. Only 3 associations recommend using organs donated by COVID-19 patients for transplantation.
Reference:
[1]Vivek B. Kute,Vidya A. Fleetwood,Hari Shankar Meshram,Alexis Guenette,Krista L. Lentine.Use of Organs from SARS-CoV-2 Infected Donors: Is It Safe? A Contemporary Review.Curr Transplant Rep. 2021 Oct 26 : 1–12.
[2]Malay B. Shah, Raymond J. Lynch, Hanine El-Haddad, Brianna Doby, Diane, Brockmeier, David S. Goldberg.Utilization of deceased donors during a pandemic: argument against using SARS-CoV-2–positive donors.05 May 2020
[3]https://www.nytimes.com/2021/11/07/health/covid-organ-transplants.html
[4]https://www.myast.org/sites/default/files/Donor%20Testing%20Document_07.07.21.pdf
[5]https://www.myast.org/sites/default/files/2021%200809%20COVID19%20FAQ.pdf
[6]N. Thao N. Galvan,Nicolas F. Moreno,Jay E. Garza,Susan Bourgeois,Marion Hemmersbach-Miller, Bhamidipati Murthy,Katherine Timmins,Christine A. O’Mahony, James Anton,Andrew Civitello,Puneet Garcha,Gabe Loor,Kenneth Liao,Alexis Shaffi,John Vierling,Rise Stribling,Abbas Rana,John A. Goss.Donor and transplant candidate selection for solid organ transplantation during the COVID-19 pandemic.10 June 2020
[7]Ola Ahmed,Diane Brockmeier,Kevin Lee,William C. Chapman,M. B. Majella Doyle.Organ donation during the COVID-19 pandemic.13 July 2020
[8] Organ Transplantation Branch of Chinese Medical Association. Guidelines for National Organ Donation and Transplantation during the Novel Coronavirus Pneumonia Epidemic (Adopted on February 23, 2020). Organ Transplantation. 2020.3.11 (12) :180-184
Fierce argument: Organ donation from died COVID-19 patients
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



