Which is better for left main coronary artery disease: Stent or Bypass?
- Did Cloud Seeding Unleash a Deluge in Dubai?
- Scientists Identify Gut Bacteria and Metabolites that Lower Diabetes Risk
- OpenAI’s Model Matches Doctors in Assessing Eye Conditions
- UK: A Smoke-Free Generation by Banning Sales to Those Born After 2009
- Deadly Mutation: A New Monkeypox Variant Emerges in the DRC
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
Which is better for left main coronary artery disease: Stent or Bypass?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Which is better for left main coronary artery disease: stent or bypass? “The Lancet” publishes Harvard’s latest research
The left main coronary artery plays an important role in the blood supply of the heart, and more than 75% of the left ventricle is inseparable for blood supply.
Therefore, once the left main coronary artery is severely occluded, the patient will have a very high risk of facing serious consequences.
However, for patients with low-to-medium-level anatomical complexity of the left main coronary artery disease, the optimal revascularization strategy is still uncertain, drug-eluting stent percutaneous coronary intervention (PCI) and coronary artery bypass grafting ( CABG, the “bridging” technique) has always been controversial.
Recently, Professor Marc S Sabatine, a cardiovascular expert at Harvard Medical School (Brigham and Women’s Hospital and Harvard Medical School), led a team to simultaneously publish important research at the American Heart Association (AHA) Annual Scientific Meeting and the Lancet. Provide a reference for the clinical strategy of this important clinical problem.
This study conducted a meta-analysis of 4394 patient data and showed that there was no significant difference in 5-year all-cause mortality between patients who received drug-eluting stent implants and those who received bypass surgery.
However, there are still trade-offs in terms of the risks of myocardial infarction, stroke, and the need for revascularization.
Screenshot source: The Lancet
Specifically, the researchers searched 1599 studies and finally included 4 high-quality randomized controlled studies (SYNTAX, PRECOMBAT, NOBLE, and EXCEL) for meta-analysis, including 4394 patients with a median SYNTAX score of 25.0. These patients were randomized to receive drug-eluting stent implantation (n=2197) or bypass surgery (n=2197) in the corresponding trial.
The SYNTAX score is a measure of the burden and complexity of coronary atherosclerosis. The score ranges from 0 to >60 points. The higher the score, the more complicated the condition is.
The primary endpoint of the study was 5-year all-cause mortality, 11.2% in the drug-eluting stent implantation group and 10.2% in the bypass surgery group. The difference between the two groups was not statistically significant.
However, the results of Bayesian analysis (inferred probability) are more inclined to have the advantage of bypass surgery. The 5-year mortality rate of drug-eluting stent implantation is 85.7% higher than that of bypass surgery, and the absolute difference in 5-year mortality rate is large. The probability is not less than 1.0%.
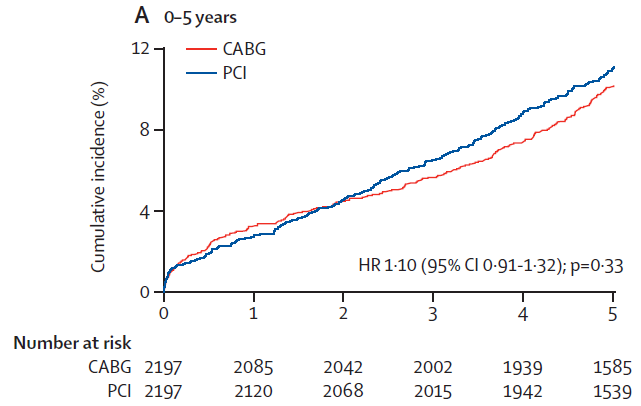
▲The 5-year all-cause mortality in the drug-eluting stent implantation group (PCI) and the bypass group (CABG) (picture source: reference [1])
At the secondary end point:
The difference in mortality is more due to non-cardiovascular deaths.
Spontaneous myocardial infarction occurred more frequently in the drug-eluting stent implantation group (6.2% vs 2.6%), and revascularization was more often required (18.3% vs 10.7%). The risks of the above events were 2.35 times that of the bypass group (HR 2.35) , 95% CI 1.71–3.23; p<0.0001) and 1.78 times (HR 1.78, 1.51-2.10; p<0.0001).
The difference in procedural myocardial infarction between the two treatment strategies depends on the definitions used in different studies.
There was no significant difference in the 5-year stroke rate between the drug-eluting stent implantation group and the bypass group (2.7% vs 3.1%), but in the first year after surgery, the drug-eluting stent implantation group had a significantly lower stroke risk by 63%.
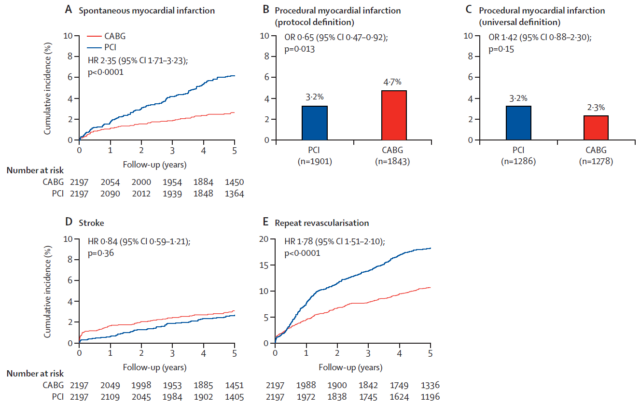
▲The risk of spontaneous myocardial infarction (A), programmed myocardial infarction (BC), stroke (D) and revascularization (E) in the drug-eluting stent implantation group (PCI) and the bypass group (CABG). (Image source: Reference [1])
Professor Sabatine said, “For every patient, these factors must be considered. These complex and subtle differences emphasize that the cardiac team needs to help patients make the most suitable treatment decisions.”
At the AHA conference, Dr. Robert Harrington of Stanford University participated in the discussion and emphasized that these results mean that there is no single best solution.
On the contrary, “the choice depends on the patient’s values and preferences, that is, what risks the patient tries to avoid and what gains they want to achieve. Benefit.
This does require careful discussion between the doctor and the patient, and consideration of the clinical and anatomical characteristics of each patient.”
In the same review article of The Lancet, two scholars from McMaster University also stated that the existing data is still not enough to distinguish between the superior and the inferior, and it is necessary to promote larger clinical trials in this field. To solve this problem.
Reference
[1] Marc S Sabatine, et al., (2021). Percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting in left main coronary artery disease: an individual patient data meta-analysis. The Lancet, DOI: https://doi.org/10.1016/S0140-6736(21)02334-5
[2] Emilie P Belley-Côté, P J Devereaux. (2021). PCI versus CABG for left main coronary artery disease: is the jury still out?. The Lancet, DOI: https://doi.org/10.1016/S0140-6736(21)02491-0
[3] Left-Main PCI, CABG Mortality Similar; Choice Remains Complex. Retrieved November 24, 2021, from https://www.medscape.com/viewarticle/963198
Which is better for left main coronary artery disease: Stent or Bypass?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



