AJRCCM: Qualitatively uncertain lung nodules!
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
AJRCCM: Qualitatively uncertain lung nodules!
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
AJRCCM: Qualitatively uncertain lung nodules!
In recent years, as people pay more attention to health and the resolution and image quality of chest CT examinations have improved, the detection rate of lung nodules and early lung cancer has increased, which has reduced the mortality rate of lung cancer by 26%-61%. [1], suggesting the importance of early detection and diagnosis in reducing the incidence and mortality of lung cancer.
Although pulmonary nodules are closely related to lung cancer , benign lesions such as inflammation and granuloma can also be expressed as nodules.
Because there is no histological diagnosis, these nodules cannot be determined as benign or malignant and are called uncertain lung nodules. Section (IPN) .
In clinical practice, the error rate of IPN diagnosis and the proportion of IPN patients undergoing invasive procedures such as needle biopsy and surgery are relatively high.
In order to avoid missed diagnosis and over-diagnosis and treatment, it is very important to seek a non-invasive and accurate diagnosis method.
Lung cancer screening and the development of lung cancer prediction models are very important in the early diagnosis of lung cancer.
Among them, PET-CT is one of the most commonly used tools for lung cancer diagnosis and staging, but it is expensive and has a false positive rate of 25% (infection The high incidence area of sexual disease can reach 39%) [2].
Some models that have been used clinically, such as the Mayo clinical model [3], based on clinical variables such as the patient’s age, smoking history, tumor history in other parts, and characteristics of the nodules.
For high-risk classification, a Mayo score lower than 0.1 is considered low risk, higher than 0.7 is considered high risk, and 0.1 to 0.7 is considered medium risk.
However, it is still unable to accurately diagnose the benign and malignant pulmonary nodules, especially for patients in the middle-risk group .
Other non-invasive diagnostic methods such as blood markers and imaging examinations are also commonly used clinical auxiliary diagnostic tools, but their accuracy needs to be further verified.
To this end, the team led by Professor Michael N Kammer carried out a prospective collection, retrospective blinding (PRoBE) study, and constructed a new lung cancer prediction model- including three biomarkers (clinical variables, hematology) And imaging omics) combined biomarker model (CBM) [4].
Specifically, the use of CBM can reduce the invasive operation rate of patients with intermediate-risk benign nodules from 62.9% to 50.6%, shorten the median time for diagnosis of lung cancer from 60 days to 21 days , and also enable patients to receive CT again. The chance of inspection is reduced by 29.1% .
This research was recently published in American Journal of Respiratory and Critical Care Medicine .
▲ Screenshot of the paper’s homepage
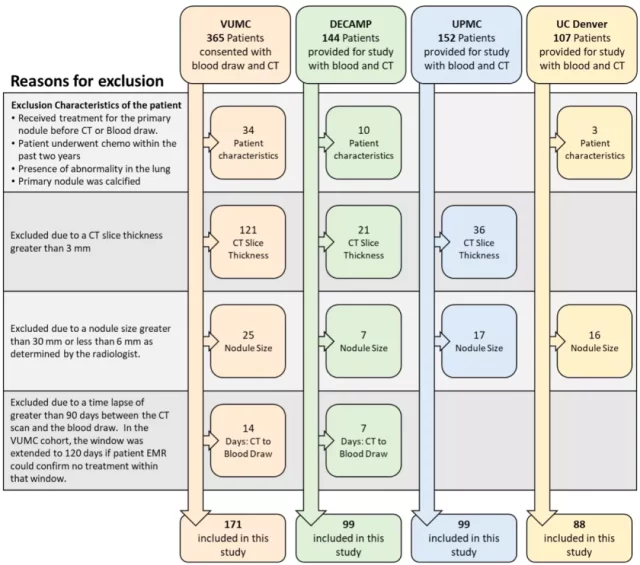
The study included 4 case-control cohorts with IPN from 4 different medical centers: VUMC cohort (n=171), DECAMP cohort (n=99), UPMC cohort (n=99) and UC Denver cohort (n= 88), a total of 456 patients.
The Kammer team first used the Mayo clinical model to divide these patients into low-, medium-, and high-risk groups, and most of the IPN (67%) of all patients were classified as medium-risk groups .
For the VUMC cohort, a Brooke University model containing emphysema, the number of lung nodules, the solid component of the nodule, and the family history of lung cancer was additionally added for risk scoring [5].
At the same time, they also collected the patient’s hematology and imaging data and followed up until the patient was diagnosed with lung cancer or benign nodules.
Among all blood biomarkers of lung cancer, multiple studies have found that serum high-sensitivity cytokeratin 19 fragment (hs-CYFRA 21-1) has a relatively high diagnostic value in IPN [6].
This study by the Kammer team also proved that hs-CYFRA 21-1 is more accurate than the Mayo clinical model alone, and the combination of hs-CYFRA 21-1 and the Mayo clinical model is better than the single hs-CYFRA 21-1. The diagnosis accuracy is higher .
Next, the Kammer team evaluated the risk of IPN based on CT imaging omics.
In all four cohorts, the diagnostic accuracy of imaging omics was higher than the Mayo clinical model.
Combining imaging omics with the Mayo clinical model can be Improve the diagnostic accuracy of both .
It can be seen that the combined model has more advantages in diagnosis than the single model, so the researchers constructed a new lung cancer prediction model CBM.
CBM includes Mayo clinical model, serum hs-CYFRA 21-1 level and CT imaging omics .
In order to verify the accuracy of the model, first train the CBM in the VUMC cohort, and calculate the difference in risk assessment after adding other biomarkers to the Mayo clinical model.
The results show that the diagnostic accuracy of a CBM are higher than a single model Mayo Clinic, Mayo Clinic genomics + image model, and the model Mayo Clinic + hs-CYFRA 21-1 levels (p values of P <1.7 × 10 – 7 , p=2.196×10 -5 and p=2.966×10 -3 ) .
Then the CBM was verified in the remaining three cohorts. The Kammer team found that in the four cohorts, the diagnostic accuracy of CBM was higher than the Mayo clinical model .
The AUC of the VUMC cohort increased by 0.104 on average, and the AUC of the DECAMP cohort increased by 0.165. , The AUC of the UPMC queue increased by 0.087, and the AUC of the UC Denver queue increased by 0.176.
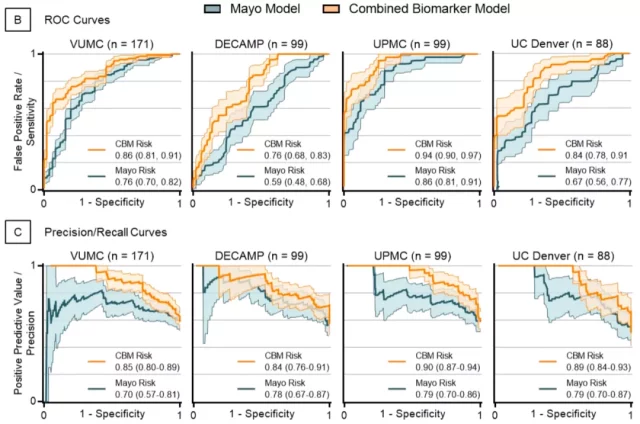
▲ Comparison of diagnostic efficacy between CBM and Mayo clinical model in 4 cohorts
In addition, for the subgroup that underwent PET-CT examination, compared with another Herder model [7] that has been used clinically, the Mayo clinical model has higher diagnostic efficiency in the VUMC cohort (AUC=0.66 vs. AUC) =0.71), but the diagnostic performance of the UC Denver cohort decreased (AUC=0.88 vs. AUC=0.83), but in these two cohorts, the diagnostic performance of CBM was the highest .
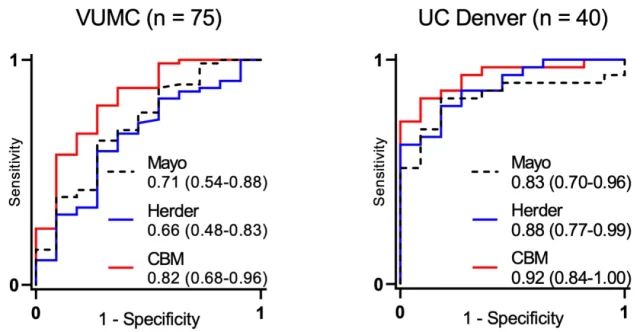
▲ Comparison of diagnostic efficacy between CBM, Herder model and Mayo clinical model
After verifying the diagnostic accuracy of CBM in an independent cohort, the Kammer team finally combined the four cohorts (n=456), re-adjusted and calibrated the model to improve the applicability of the model in the clinic.
As expected, the diagnostic accuracy of CBM in the combined cohort was superior to the Mayo clinical model, blood biomarkers, and imaging omics, and the AUC of the Mayo clinical model was increased by 0.124 (95%CI: 0.091- 0.156, p<2×10 -16 ) .
In general, CBM improves the accuracy of clinical diagnosis in a series of situations.
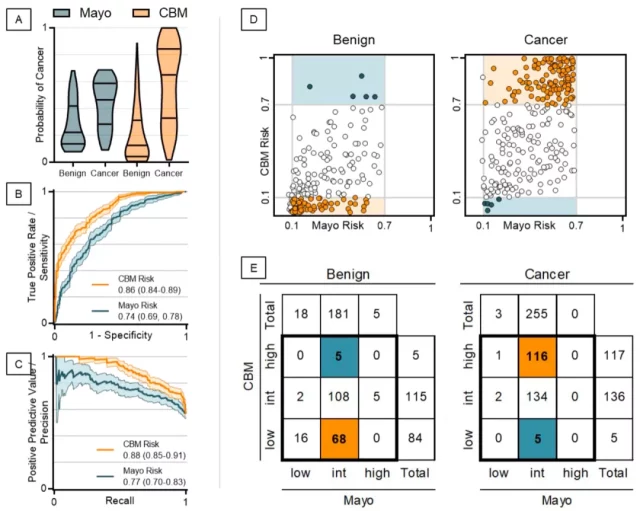
▲ Comparison of the diagnostic efficacy of CBM and Mayo clinical model in the combined cohort
Finally, clinical follow-up of all patients found that using CBM and British Thoracic Society (BTS) guidelines to guide the diagnosis of IPN patients can reduce the invasive operation rate of patients with benign nodules at medium risk from 62.9% to 50.6%. % of 12.3 (P = 0.1127), the CBM will be diagnosed with lung cancer, the median time from 60 days to 21 days (p <0.0001), to improve the survival rate of patients with lung cancer to some extent, but also the patient receiving CT examination again The odds are reduced by 29.1% .
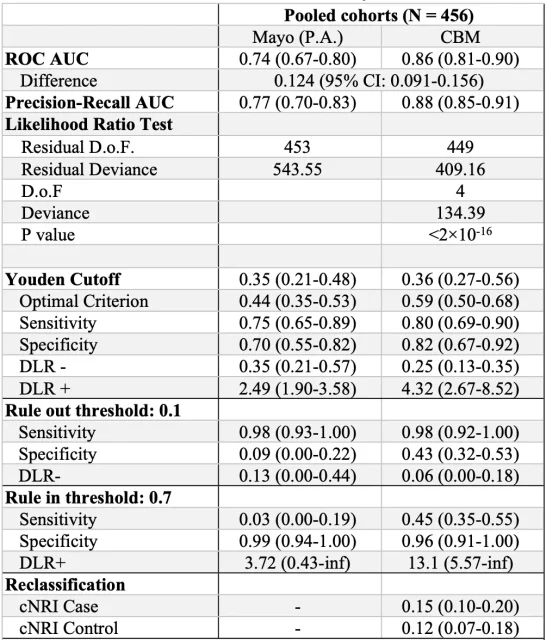
▲ Validation results of CBM and Mayo clinical model in the combined cohort
In general, compared with the Mayo clinical model and expensive PET-CT, CBM only needs to increase the CT imaging analysis of lung nodules and fast and cheap hematology detection.
More importantly, compared with existing predictive models, the combined biomarker model based on three biomarkers (clinical variables, hematology, and imaging omics) not only significantly improves the diagnostic accuracy of IPN patients, but also While realizing early diagnosis, unnecessary invasive operations are reduced .
Sicentists look forward to the early promotion of CBM in clinical practice to benefit patients with pulmonary nodules!
references:
[1] de Koning, H.J., C.M. van der Aalst, P.A. de Jong, et al., Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020;382(6):503-513. doi:10.1056/NEJMoa1911793
[2] Deppen, S.A., J.D. Blume, C.D. Kensinger, et al., Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: a meta-analysis. Jama. 2014;312(12):1227-1236. doi:10.1001/jama.2014.11488
[3] Gould, M.K., L. Ananth, and P.G. Barnett, A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388. doi:10.1378/chest.06-1261
[4] Kammer, M.N., D.A. Lakhani, A.B. Balar, et al., Integrated Biomarkers for the Management of Indeterminate Pulmonary Nodules. Am J Respir Crit Care Med. 2021;204(11):1306-1316. doi:10.1164/rccm.202012-4438OC
[5] McWilliams, A., M.C. Tammemagi, J.R. Mayo, et al., Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919. doi:10.1056/NEJMoa1214726
[6] Kammer, M.N., A.K. Kussrow, R.L. Webster, et al., Compensated Interferometry Measures of CYFRA 21-1 Improve Diagnosis of Lung Cancer. ACS Comb Sci. 2019;21(6):465-472. doi:10.1021/acscombsci.9b00022
[7] Herder, G.J., H. van Tinteren, R.P. Golding, et al., Clinical prediction model to characterize pulmonary nodules: validation and added value of 18F-fluorodeoxyglucose positron emission tomography. Chest. 2005;128(4):2490-2496. doi:10.1378/chest.128.4.2490
AJRCCM: Qualitatively uncertain lung nodules!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



