Oral contraceptives and hormone replacement therapy need to be cautious!
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
- New Ocrevus Subcutaneous Injection Therapy Shows Promising Results in Multiple Sclerosis Treatmen
- Dutch Man Infected with COVID-19 for 613 Days Dies: Accumulating Over 50 Virus Mutations
Eight-year follow-up of more than one million women: oral contraceptives and hormone replacement therapy need to be cautious! The risk of gout may increase!
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Eight-year follow-up of more than one million women: oral contraceptives and hormone replacement therapy need to be cautious! The risk of gout may increase!
Gout is the most common inflammatory arthritis in adults, and its incidence has been increasing in recent decades.
The incidence of gout in men is 3-10 times that of women. However, the incidence of gout in postmenopausal women increases, while premenopausal women are protected by estrogen.
Past epidemiological studies have investigated the relationship between reproductive factors and gout.
A cross-sectional analysis of 1530 women showed that postmenopausal status, early menarche age, and oral contraceptive (OC) use were associated with high serum uric acid concentrations.
In the nurse’s health study, early menopause was associated with an increased risk of gout, and hormone replacement therapy (HRT) was associated with a reduced risk of gout.
However, there are conflicting results in other research reports.
A study published in 2008 analyzed data from the National Health and Nutrition Examination Survey (NHANES) from 1988 to 1994. It reported that menopause was associated with higher serum uric acid levels, and hormone replacement therapy was associated with lower uric acid levels.
In contrast, a study analyzing NHANES data from 1999 to 2010 showed that the prevalence of hyperuricemia was not related to menopause or current use of HRT.
As shown above, the results of the association between gout and female reproductive factors are largely inconclusive.
In the studies so far, the maximum sample size is 120,000 subjects, and many studies are conducted in a case-control or cross-sectional manner.
In addition, various reproductive factors are not included. In premenopausal and postmenopausal women, the influence of reproductive factors on the occurrence of the disease may be different.
Variables such as menopausal age, reproductive span and HRT can only be evaluated in postmenopausal women.
Therefore, this study aims to investigate the relationship between various female reproductive factors and the incidence of gout in postmenopausal women across the country.
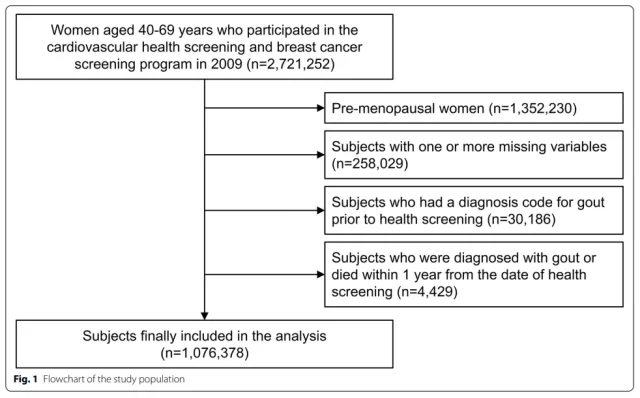
The study included 1076378 postmenopausal women aged 40-69, with an average follow-up time of 8.1 years, and 64,052 cases of gout (incidence rate was 7.31 per 1,000 person-years).
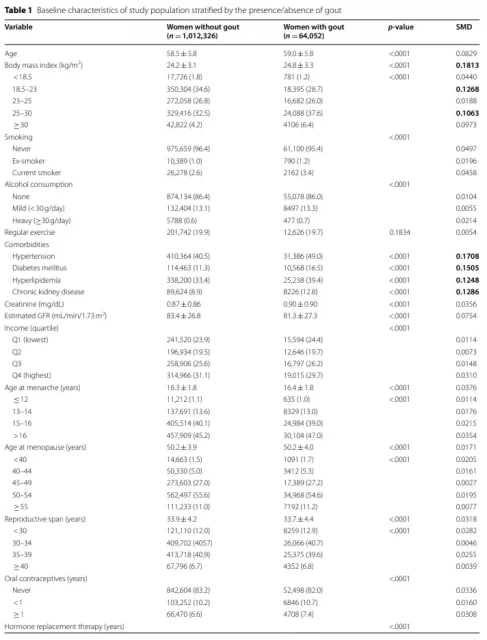
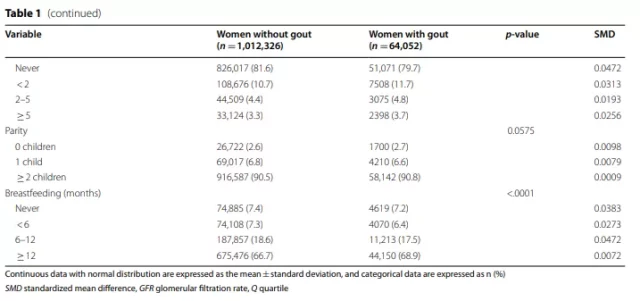
1. Baseline characteristics
The baseline characteristics of the study population stratified according to the presence or absence of gout are shown in Table 1.
The average ages of the subjects with gout and without gout were 59.0 years and 58.5 years, respectively. Compared with women without gout, women diagnosed with gout have a higher BMI and a higher percentage of comorbidities.
Although the difference is not significant (standardized mean difference <0.1), compared with subjects without gout, subjects diagnosed with gout have late menarche, early menopause, shorter reproductive period, use of OC, HRT, and breastfeeding ≥1 The proportion of the year is higher.
2. The relationship between the incidence of gout and endogenous estrogen related factors
The average follow-up time was 8.14±1.2 years. During the study period, 64,052 people were newly diagnosed with gout (incidence rate 7.31/1000 person-years).
In the multivariate model, a later age at menarche, an earlier age at menopause, and a shorter reproductive period were associated with an increased risk of gout (Table 2).
Women who experienced menarche after the age of 16 had a higher risk of gout than women who experienced menarche before the age of 12 (Adjusted HR [aHR] 1.10, 95% CI 1.02-1.19).
Compared with women who were menopausal between 50-54 years old, menopause before 50 years old (<40 years old [aHR 1.12, 95% CI 1.06-1.19], 40-44 years old [aHR 1.06, 95% CI 1.02-1.10] and 45 Women aged -49 years [aHR 1.03, 95% CI 1.01–1.04]) have a higher risk of gout, while women who have undergone menopause after 55 years of age (aHR 0.97, 95% CI 0.94–0.99) have a lower risk.
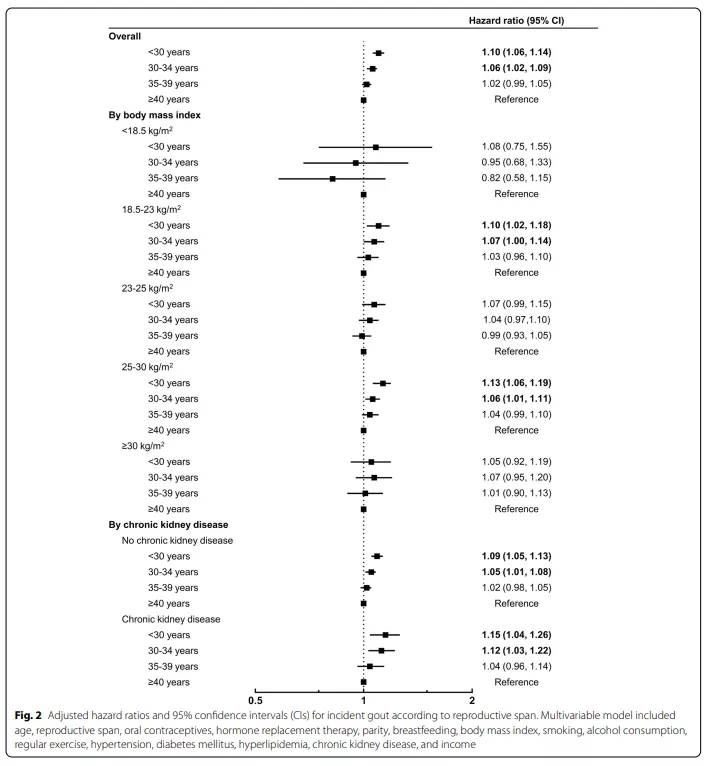
Compared with women with a reproductive span ≥40 years, women with a reproductive span <35 years have a higher risk of gout: <30 years (aHR 1.10, 95% CI 1.06-1.14) and 30-34 years old (aHR 1.06, 95%) CI 1.02-1.09) (Figure 2).
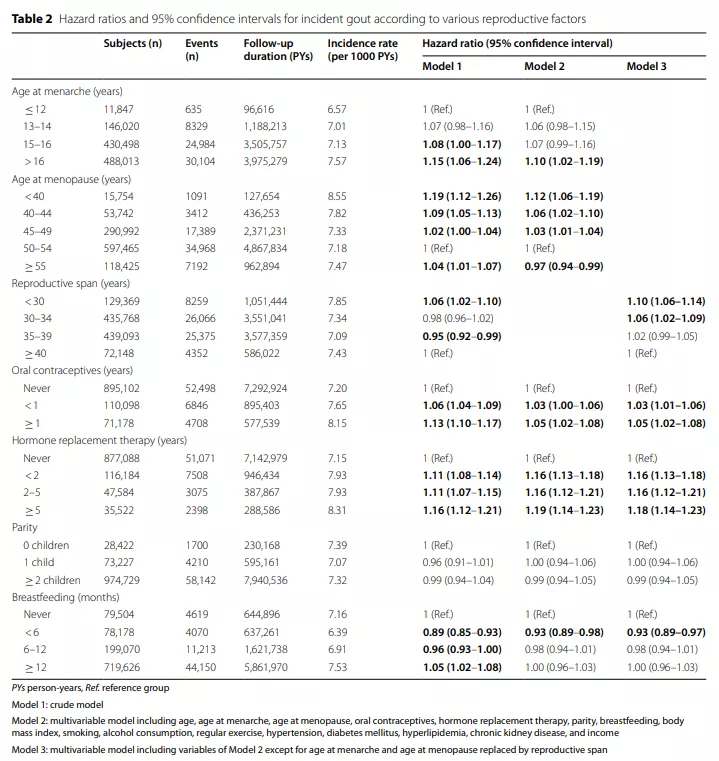
3. The relationship between the incidence of gout and related factors of exogenous estrogen
Compared with women who have never used OC (oral contraceptives), women who use OC have a higher risk of gout (aHR for women who use OC for <1 year is 1.03, 95% CI is 1.00-1.06, and use OC ≥ The aHR of the 1-year female was 1.05, and the 95% CI was 1.02-1.08).
The use of HRT (hormone replacement therapy) is also associated with an increased risk of gout, and the risk is highest in patients using HRT>5 (aHR 1.19, 95% CI 1.14-1.23).
4. The relationship between the incidence of gout and pregnancy-related factors
Parity does not affect the risk of gout. Compared with subjects who had never breastfed, subjects who were breastfed for less than 6 months had a lower risk of gout (aHR 0.93, 95% CI 0.89–0.97).
However, breastfeeding for ≥6 months was not associated with gout risk (aHR 0.98, 95% CI 0.94-1.01 for 6-12 months, aHR 1.00, 95% CI 0.96-1.03 for 6-12 months).
5. Hierarchical analysis
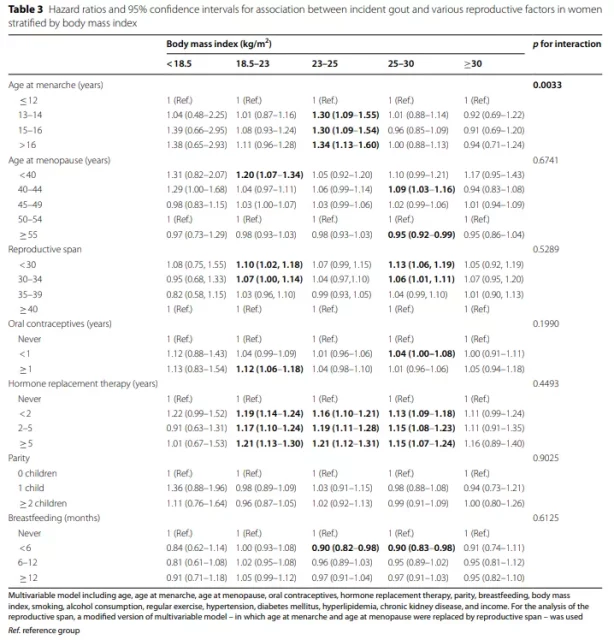
Table 3 shows the influence of reproductive factors on the risk of gout in women stratified by BMI.
The association between the age at menarche and the onset of gout differed according to the BMI group (interaction p = 0.0033).
n the hyper-recombination, the late menarche age was most significantly associated with the risk of gout (aHR 1.30, 95% CI 1.09-1.55 for the 13-14 year old group vs. aHR 1.30, 95% CI 1.09-1.54 vs. 15-16 year old group) . >16-year-old group aHR 1.34, 95% CI 1.13-1.60).
In the normal and underweight group, the risk is no statistical significance, but still observed with age at menarche increasing trend.
However, in the obesity and severe obesity groups, there was no association between age at menarche and gout risk. The association between other reproductive factors and the onset of gout was not affected by BMI (interaction p>0.05).
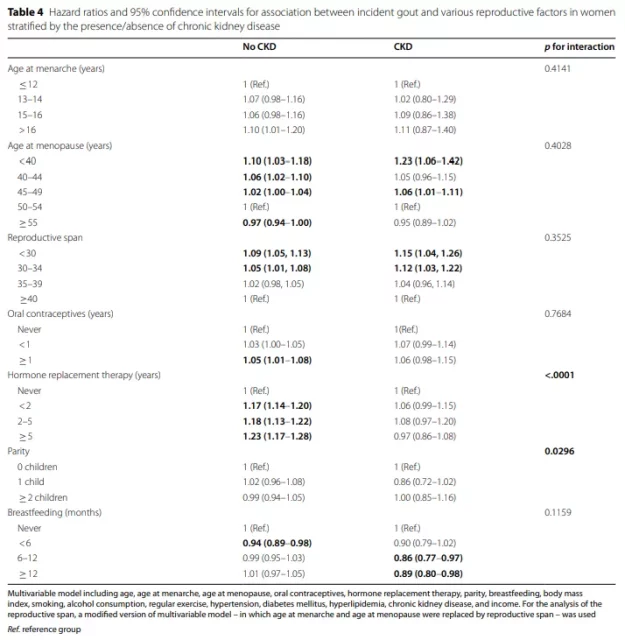
In a stratified analysis based on the presence or absence of CKD, the relationship between menarche age, menopausal age, reproductive period, parity, and gout risk did not differ between the groups (Table 4).
In the CKD group, breastfeeding for >6 months was associated with a lower incidence of gout (breastfeeding for 6-12 months: aHR 0.86, 95% CI 0.77-0.97, breastfeeding for ≥12 months: aHR 0.89, 95 % CI 0.80-0.98). OC use> 1 year (aHR 1.05, 95% CI 1.01–1.08) and HRT (use <2 years: aHR 1.17, 95% CI 1.14–1.20, use 2–5 years: aHR 1.18, 95% CI 1.13–1.22, Use for ≥5 years: aHR 1.23, 95% CI 1.17–1.28,) only showed a high risk of gout in the group without CKD.
In summary, in this population-based cohort of large-scale postmenopausal women, the average follow-up time was 8.1 years, and the incidence of gout was 64,052 (incidence rate was 7.31 per 1,000 person-years).
Late menarche, earlier menopause age and shorter reproductive period are associated with a high risk of gout.
No association between parity and gout incidence was observed.
The use of oral contraceptives (OC) and hormone replacement therapy (HRT) is associated with an increased risk of gout.
The association between reproductive factors and gout was not statistically significant in the high BMI group.
The effect of OC and HRT on gout was not significant in the CKD group.
In general, this study found that shorter exposure to endogenous estrogen is associated with an increased risk of gout events.
Exposure to exogenous estrogen, such as OC and HRT, is associated with a high risk of developing gout.
However, this association is weak in severely obese women and CKD women. Subsequent research is needed to further determine the mechanism by which reproductive factors affect the development of gout.
Reference:
Eun et al.Association between female reproductive factors and gout: a nationwide population-based cohort study of 1 million postmenopausal women.Arthritis Research & Therapy (2021) 23:304
https://doi.org/10.1186/s13075-021-02701-w
Oral contraceptives and hormone replacement therapy need to be cautious!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



