Atrial fibrillation risk doubles after breast cancer diagnosis? !
- Did Cloud Seeding Unleash a Deluge in Dubai?
- Scientists Identify Gut Bacteria and Metabolites that Lower Diabetes Risk
- OpenAI’s Model Matches Doctors in Assessing Eye Conditions
- UK: A Smoke-Free Generation by Banning Sales to Those Born After 2009
- Deadly Mutation: A New Monkeypox Variant Emerges in the DRC
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
EHJ: Atrial fibrillation risk doubles after breast cancer diagnosis? !
Atrial fibrillation is known to be an important cause of thrombosis-related disease and cardiovascular-related death [1].
Over the past 20 years, atrial fibrillation has received increasing attention, especially in patients diagnosed with cancer .
Breast cancer is a cancer with a high incidence in women. Improvements in breast cancer treatment over the past two decades have increased patient survival rates.
However, the increasing risk of cardiovascular disease has become a limiting factor for optimal prognosis in breast cancer patients [2].
Although we already know that atrial fibrillation has a poor prognosis in noncancer populations [3], we still do not know the incidence of atrial fibrillation after breast cancer diagnosis and how atrial fibrillation affects breast cancer prognosis [4] ].
After breast cancer diagnosis, should a cardiologist be brought in to prevent and manage possible cardiovascular risks? This article will tell you the answer.
A recent study led by Dr. Avirup Guha of Case Western Reserve University in the United States analyzed breast cancer cases in the SEER database and found that within the first 60 days of newly diagnosed breast cancer, the incidence of atrial fibrillation was 3.3%. Among control non-cancer participants, it was only 1.8% [5].
In addition, the grade of breast cancer also affects the incidence of atrial fibrillation.
According to the American Joint Committee on Cancer (AJCC) classification of breast cancer, compared with patients with stage I, patients with stage II are associated with a 51% higher risk of atrial fibrillation, and patients with stage III are associated with a 51% higher risk of atrial fibrillation.
Stage IV patients were associated with a 163% increased risk of atrial fibrillation, and patients with stage IV disease were associated with a 321% increased risk of atrial fibrillation .
Notably, new-onset atrial fibrillation after breast cancer diagnosis was also associated with a 200% increased risk of cardiovascular-related death within 1 year of cancer diagnosis .
The study was published in the European Heart Journal .

Let’s take a look at how the Guha team did it.
They used data from the SEER database from 2007 to 2014.
Patients with breast cancer were included if they were diagnosed with any grade of breast cancer between 2007 and 2013, and were 66 years of age and older.
The last follow-up date was December 31, 2014.
The diagnosis of breast cancer was based on the ICD-O-3 standard. Exclusion criteria were cancer diagnosis based on autopsy, month of cancer diagnosis was unclear, other cancers previously diagnosed, or precancerous lesions.
In addition, the investigators matched noncancer control participants with breast cancer patients by year of birth, ethnicity, SEER-registered geographic location, and the Charlson comorbidity index.
Ultimately, the study included 85,423 breast cancer patients and 412,557 non-cancer participants.
Among breast cancer patients, 9425 (11%) had AF diagnosed before breast cancer diagnosis, and their median age was 81 years. One year after breast cancer diagnosis, 2993 (3.3%) were newly diagnosed with atrial fibrillation .
The incidence of newly diagnosed atrial fibrillation within 30 days and 6 months after breast cancer diagnosis was 0.6% and 2.1%, respectively. Corresponding AF rates in breast cancer patients after diagnosis are consistently higher than in non-cancer controls.
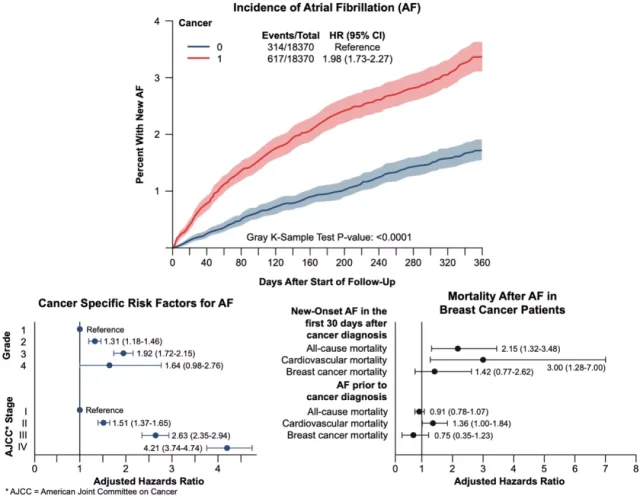
The incidence of AF after diagnosis in breast cancer patients has been consistently higher than in non-cancer controls. Red and blue correspond to breast cancer patients and non-cancer controls, respectively, the horizontal axis is time (days), and the vertical axis represents the proportion of newly diagnosed atrial fibrillation cases to the total number.
Let’s look at the corresponding risk factors for atrial fibrillation.
The Guha team found that age, ethnicity, and some socioeconomic factors were highly associated with newly diagnosed atrial fibrillation in breast cancer populations.
For example, age 70-80 years was associated with a 31% increased risk of atrial fibrillation, compared with age younger than 70 years.
Many cardiovascular-related risk factors are highly associated with newly diagnosed atrial fibrillation in the breast cancer population.
For example, high blood pressure was associated with a 46% increased risk of newly diagnosed atrial fibrillation in breast cancer patients, diabetes was associated with a 55% increased risk of newly diagnosed atrial fibrillation in breast cancer patients, and a history of stroke was associated with a 70% increased risk of newly diagnosed atrial fibrillation in breast cancer patients.
Notably, depression was associated with a 21% increased risk of newly diagnosed AF in the breast cancer population, while anemia was associated with a 46% increased risk of newly diagnosed AF .
And as outlined in our abstract, the stage of the cancer is also associated with the risk of newly diagnosed AF in the breast cancer population.
According to the AJCC stage, compared with stage I , stage II is associated with a 51% higher risk of AF, and stage III is associated with a 51% higher risk of AF. was associated with a 163% increase, and stage IV was associated with a 321% increased risk of atrial fibrillation .
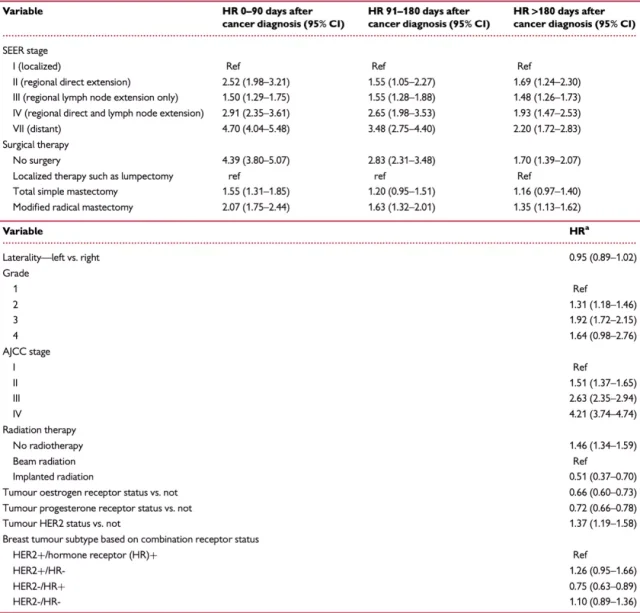
Guha’s team also did other analyses on the association between cancer grade and atrial fibrillation risk.
They used another set of staging methods called individual breast cancer staging (stages 1-3).
In the group with lower cancer stage, the group not receiving hormone therapy had a higher chance of developing atrial fibrillation than the group receiving hormone therapy.
For example , in patients with stage 1 breast cancer, no hormone therapy was associated with a 1018% increased risk of atrial fibrillation compared with patients receiving hormone therapy;
in patients with stage 2 breast cancer, no hormone therapy compared with patients receiving hormone therapy was associated with a 732% increased risk of atrial fibrillation;
in stage 3 patients, no hormone therapy was associated with a 528% increased risk of atrial fibrillation compared with those who received hormone therapy .
Cardiovascular drugs (beta-blockers, angiotensin-converting enzyme (or receptor) inhibitors, spironolactone, eplerenone) can reduce the likelihood of atrial fibrillation in all breast cancer grade groups; However, the degree of risk reduction by these drugs did not differ significantly across breast cancer grades.
For example, among patients with stage 3 breast cancer, beta-blockers were associated with a 73% lower risk of atrial fibrillation compared with those who did not.
Risk factors associated with new-onset atrial fibrillation in breast cancer patients
In addition, different treatments received after breast cancer diagnosis were also associated with a different risk of newly diagnosed atrial fibrillation.
Breast cancer patients who did not receive surgery and radiation as first-line therapy were associated with an increased risk of newly diagnosed AF .
Specifically, no surgery was associated with a 339% higher risk of newly diagnosed AF compared with simple resection .
Compared with radiotherapy, no radiotherapy was associated with a 46% higher risk of newly diagnosed AF .
Let’s look at the outcomes of atrial fibrillation-related death among breast cancer patients.
Patients with new-onset atrial fibrillation within the first 30 days after breast cancer diagnosis had a 1-year survival rate of 62.2% .
Patients who have had atrial fibrillation before the diagnosis of breast cancer have a 1-year survival rate of about 80% .
In conclusion, this study found that breast cancer patients were nearly twice as likely to have new-onset atrial fibrillation within 1 year of diagnosis as those without cancer (3.3% vs 1.8%) .
Moreover, the risk of developing atrial fibrillation varies significantly with different grades of breast cancer. New-onset atrial fibrillation after breast cancer diagnosis increases all-cause and cardiovascular-related deaths.
Therefore, it is very important to introduce an interdisciplinary collaboration between cardiology and oncology to manage or prevent the associated risk of atrial fibrillation after breast cancer is diagnosed.
Interventions to manage the risk of atrial fibrillation in breast cancer patients can strongly improve their cardiovascular-related and overall outcomes.
references:
1. Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the US adult population. Am J Cardiol. 2013;112(8):1142- 1147. doi:10.1016/j.amjcard.2013.05.063
2. Guha A, Dey AK, Jneid H, Addison D. Acute Coronary Syndromes in Cancer Patients. Eur Heart J. 2019;40(19):1487-1490. doi:10.1093/eurheartj/ehz267
3. Piccini JP, Hammill BG, Sinner MF, et al. Clinical course of atrial fibrillation in older adults: the importance of cardiovascular events beyond stroke. Eur Heart J. 2014;35(4):250-256. doi:10.1093/ eurheartj/eht483
4. Guha A, Dey AK, Jneid H, Ibarz JP, Addison D, Fradley M. Atrial Fibrillation in the Era of Emerging Cancer Therapies. Eur Heart J. 2019;40(36):3007-3010. doi:10.1093/eurheartj /ehz649
5. Guha A, Fradley MG, Dent SF, et al. Incidence, risk factors, and mortality of atrial fibrillation in breast cancer: a SEER-Medicare analysis [published online ahead of print, 2021 Nov 14]. Eur Heart J. 2021 ;ehab745.doi:10.1093/eurheartj/ehab745
Atrial fibrillation risk doubles after breast cancer diagnosis? !
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



