What is TAM-targeted tumor nano-immunotherapy?
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
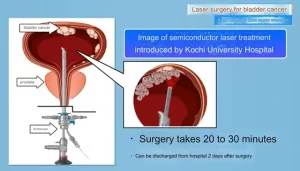
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
What is TAM-targeted tumor nano-immunotherapy?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What is TAM-targeted tumor nano-immunotherapy?
Cancer immunotherapy has emerged as a breakthrough approach in cancer treatment by activating the innate and adaptive immune systems to eliminate tumors.
Despite exciting results in clinical trials, several issues remain to be addressed, such as limited durable response rates, immune-related side effects, and abnormal clinical responses.
The tumor microenvironment ( TME ) has been shown to be an important cause of tumor immune escape and treatment failure.
Tumor-associated macrophages ( TAMs ), an important component of the TME, are often associated with poor prognosis and drug resistance, and have emerged as very promising targets in cancer immunotherapy.
Nanotechnology is a multidisciplinary field of scientific research that focuses on various types of nanomaterials.
With the development of nanobiotechnology, nanomaterials have received extensive attention in tumor immunotherapy due to their advantages in targeted drug delivery, precise localized drug release, simple surface functionalization, and biological activity.
Nano-immunotherapy is a treatment method based on nanomaterials, which improves the therapeutic effect of immunotherapy by modulating the immunosuppressive microenvironment, thereby activating the immune system by interacting with other immune cells.
In fact, targeted drug delivery systems based on a variety of nanomaterials have greatly changed the field of TAM-related immunotherapy.
Tumor-associated macrophages
TAMs are functionally heterogeneous and are divided into two major subpopulations, M1 and M2 macrophages.
In response to lipopolysaccharide ( LPS ), IFN-γ and GM-CSF, M1 macrophages undergo classical activation and preferentially secrete antimicrobial molecules and pro-inflammatory cytokines, including reactive oxygen species ( ROS ), nitric oxide ( NO ) and IL-6.
M1 macrophages are the first line of defense against microbial infection. M1 macrophages also maintain a strong antigen-presenting capacity, inducing a strong Th1 response.

In contrast, M2 macrophages undergo selective activation by IL-4, IL-13, IL-10, and CSF-1, and preferentially secrete anti-inflammatory cytokines, including transforming growth factor beta ( TGF-β ), IL- 10 and proteases ( such as arginase-1 and MPPs ).
M2 macrophages play a key role in limiting immune responses, inducing angiogenesis, and tissue repair.
Thus, the presence of M2-like TAMs is associated with pro-tumor activity, while the presence of M1-like TAMs is associated with antitumor activity.
Immunosuppressive effects of TAMs
TAMs suppress antitumor immune responses through multiple mechanisms. First, TAMs can inhibit T cell function by directly engaging with T cell suppressor and apoptosis receptors.
TAMs express B7-1/CD80 and B7-2/CD86, which can bind to the co-inhibitory receptor CTLA-4 expressed by T cells with higher affinity than the CD28 co-stimulatory receptor, thereby inhibiting T cell activation.
In addition, PD-L1 and PD-L2 are also overexpressed on TAMs of various cancer tissues, and TAMs can also directly promote T cell apoptosis through the expression of their Fas ligand ( FasL ) and TRAIL.
TAMs also express nonclassical human leukocyte antigen ( HLA ) class I molecules such as HLA-E and HLA-G.
Both HLA-E and HLA-G are HLA class Ib molecules that inhibit the activity of different immune cell types by interacting with specific inhibitory receptors expressed on the surface of immune cells.
Similar to many other immunosuppressive cell types present in the tumor microenvironment, TAMs suppress antitumor immune responses by producing inhibitory cytokines such as IL-10 and TGF-β1.
Together, these cytokines inhibit activation, differentiation, proliferation and function of effector T cells.
At the same time, IL-10 and TGF-β1 also promote the expansion of suppressor T cells.
TAMs can also indirectly suppress antitumor immune responses through the production of chemokines ( such as CCL2, CCL5, CCL20 and CCL22 ) and immunosuppressive metabolites ( such as kynurenine and ROS ).
These chemokines are involved in the recruitment of regulatory T cells ( Tregs ) to the tumor microenvironment, which in turn inhibit the activity of effector T cells, NK cells, and antigen-presenting cells ( APCs ) through a variety of mechanisms.
The presence of kynurenine and its derivatives inhibited the proliferation and activity of effector T cells and NK cells, and promoted the differentiation of Tregs.
TAMs also promote tumor immune evasion by expressing signal regulatory protein alpha ( SIRPα ).
SIRPα is a receptor for CD47, which is frequently overexpressed on tumor cells and plays a key role in tumor escape by binding to SIRPα to send a “don’t eat me” signal to macrophages.
Potential therapeutic strategies for targeting TAMs with nanotechnology
Nanotechnology holds great promise for improving the efficacy of tumor immunotherapy.
Given the role of TAMs in suppressing antitumor immunity, various nanotechnological approaches have been developed to target TAMs, including termination of macrophage recruitment, interference with TAM survival, and reprogramming of M2-type TAMs to M1-type.
Recent advances in the specific enhancement of antitumor immune responses by targeting TAMs with nanomaterials have shown great potential.

Termination of macrophage recruitment
Multiple studies have shown that macrophage recruitment of chemokines ( CCL2, CCL3, CCL4, and CCL5 ), CSF-1, and VEGF are possible therapeutic targets that can prevent the spread of malignancies by blocking prometastatic TAMs.
To block the CCL2-CCR2 axis, the researchers designed siRNA-CCR2-coated cationic nanoparticles ( CNP-siCCR2 ) to inhibit tumor growth and metastasis by blocking the CCL2-CCR2 axis and remodeling the TME, thereby inhibiting monocytes Expression of CCR2.
In a recent study, researchers designed ultra-small copper nanoparticles targeting CCR2 ( Cu@CuOx ) as nanocarriers for gemcitabine for PET-guided drug delivery into pancreatic ductal adenocarcinoma tumors.
These nanoparticles specifically target CCR2 on monocytes/macrophages and successfully inhibit TAM recruitment to tumors, which synergizes with the therapeutic effect of gemcitabine, ultimately inhibiting tumor growth and prolonging the survival of PDAC tumors time.
In addition, these ultra-small nanoparticles showed rapid clearance rates with reduced toxicity.
Clearance of TAM
Given the importance of CSF-1R in macrophages, studies have shown that nanoparticles loaded with CSF-1R inhibitors can effectively deplete TAM and inhibit tumor growth and metastasis.
The researchers also designed dual-targeting nanoparticles ( M2NPs ) composed of α-peptide combined with M2-pep ( M2 macrophage-binding peptide ) and loaded with anti-CSF-1R siRNA to precisely block M2-type TAMs.
Survival signal that enhances T cell function and inhibits tumor growth in melanoma. In addition, Tian et al. synthesized pegylated calcium diphosphate ( CaBP-PEG ) nanoparticles containing calcium chloride and diphosphate , which scavenge TAM, normalize the vasculature, and reduce angiogenesis, thereby reducing hypoxia, Inhibits tumor growth in breast cancer.
Surface markers of macrophages, such as CD206, can also be used as therapeutic targets. Based on this concept, Zang et al. developed nanotherapeutics of lipid-encapsulated calcium zoledronate nanoparticles ( CaZol@pMNPs ), externally covered with pH-sensitive materials, to increase cellular internalization and zoledronic acid in low pH TMEs The delivery of salts to TAMs, resulting in clearance of TAMs, reduction of angiogenesis and removal of immunosuppression, significantly reduced tumor growth.
Phosphatidylserine ( PS ) on the outer surface of cell membranes has also been used as a targeting ligand in nanoparticles. In view of MMP-2 overexpression in cancer cells and PS-induced phagocytosis of apoptotic cells, Liu et al. recently developed MMP-2-sensitive nanoparticles with PS-coated surfaces and loaded with dasatinib. In the present study, PS on the surface of nanoparticles was externalized by MMP-2 secreted by tumor cells and sent an “eat me” signal to TAMs. Studies have shown that these nanoparticles exhibit comparable accuracy and efficiency in TAM targeting and drug delivery in various biological and tumor-bearing mouse models.

Furthermore, radiation therapy can ionize DNA or generate reactive oxygen species ( ROS ), release tumor-associated antigens ( TAAs ), and induce the production of damage-associated molecular patterns within the TME, leading to ICD.
Recently, Huang et al. constructed self-assembled bifunctional nanoparticles ( ZGd-NRs ) based on zoledronic acid and gadolinium , which can efficiently deposit X-rays and generate a large number of hydroxyl radicals to stimulate ICD.
Ultimately, ZGd NRs can specifically deplete TAM, reprogram the immunosuppressive TME by inhibiting TGF-β, IL-10, and VEGF, enhance CD8+ T cell infiltration, and significantly enhance primary, distant, and metastatic tumors Immune response to anti-PD-L1 therapy.
Reprogram M2 to M1
Toll-like receptor ( TLR ) agonists are thought to be drugs that polarize M2-type TAMs to M1-type, Rodell et al. designed β-cyclodextrin nanoparticles ( CDNPs ) encapsulating R848 ( TLR-7/8 agonist ), a potent driver of the M1 phenotype.
Rapid uptake of these nanoparticles effectively improved drug delivery to TAMs, shifted them towards the tumoricidal M1 phenotype, inhibited tumor growth in colorectal cancer, and enhanced anti-PD-1 antitumor immune responses.

To improve the efficacy and specificity of macrophages, Zhang et al. recently prepared TLR agonist-loaded nanoparticles to modulate the TME.
Here, they encapsulated R848 into polylactic-glycolic acid ( PLGA ) and then covered the B16-OVA cancer cell membrane ( to avoid removal by the reticuloendothelial system ), which was further modified with M2-pep and named PNP@ R@MT.
Studies have demonstrated that PNP@R@MT can specifically deliver drugs to M2 macrophages and repolarize them to the M1 type significantly, activate anti-tumor immune responses, reduce tumor size and prolong animal survival.
Summary
TAMs are innate immune cells residing in the TME, which promote the occurrence and development of tumors and inhibit anti-tumor immunity.
Drugs that clear TAMs, prevent their recruitment or activate their repolarization to the antitumor M1 type have shown great potential for clinical application.
Recent advances in nanobiotechnology have focused attention on targeting TAMs.
Nanotechnology has improved the stability and localization of TAM-targeted drugs and reduced drug toxicity in healthy tissues.
Meanwhile, after uptake of nanoparticles, TAM distributes them throughout the tumor, including hypoxic regions, which enhances the distribution and permeability of nanoparticles and their loads in tissues.
However, despite some successes of TAM-targeted nanoparticles in cancer immunotherapy and drug delivery, there are still many problems and obstacles to overcome.
Due to the specific heterogeneity of TAMs, the time course of macrophage recruitment and polarization state is unclear, and macrophage infiltration also depends on disease severity and stage.
In addition, some targets have similarities in normal cellular receptors that may lead to side effects and toxicity.
In addition, the immune environment in tumors is complex, and TAM-based cancer immunotherapy alone is not sufficient to eliminate tumors.
It needs to be combined with other immunotherapies such as checkpoint inhibitors, CAR-T cell therapy or chemotherapy and radiation.
To generate synergistic effects and avoid significant adverse effects, combination therapies must be carefully designed based on the properties of nanoparticles and TMEs.
If these obstacles can be addressed and better targeted nanoparticles can be designed, macrophages are expected to be a powerful weapon in overcoming the problems associated with solid tumors for the benefit of cancer patients.
references:
1.Heterogeneous Myeloid Cells in Tumors. Cancers(Basel). 2021 Aug; 13(15): 3772.
2. Tumor-associated macrophages in cancer:recent advancements in cancer nanoimmunotherapies. J Exp Clin Cancer Res. 2022;41: 68.
What is TAM-targeted tumor nano-immunotherapy?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.