Unexplained acute hepatitis in children may be related to COVID superantigens
- Did Cloud Seeding Unleash a Deluge in Dubai?
- Scientists Identify Gut Bacteria and Metabolites that Lower Diabetes Risk
- OpenAI’s Model Matches Doctors in Assessing Eye Conditions
- UK: A Smoke-Free Generation by Banning Sales to Those Born After 2009
- Deadly Mutation: A New Monkeypox Variant Emerges in the DRC
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
Unexplained acute hepatitis in children may be related to COVID superantigens
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
The Lancet: Unexplained acute hepatitis in children may be related to COVID superantigens.
Recently, at least 348 cases of severe acute hepatitis of unknown cause in children have been reported in the UK, EU, US, Israel and Japan.
Most children present with early gastrointestinal symptoms, which later develop jaundice and, in some cases, acute liver failure. To the confusion of scientists, the hepatitis A, B, C, D and E viruses were not found in these children.
The current figures may be just the tip of the iceberg, as many countries are just beginning to ramp up surveillance for this unexplained childhood case of acute hepatitis.
The United Kingdom is the country reporting the most cases of acute hepatitis of unknown cause in children this time.
According to the survey information of the UK Health Security Agency (UKHSA) : all the children have undergone nucleic acid testing for the COVID-19, but most of the children have not done serological testing for the COVID-19.
What caused more than 300 cases of acute hepatitis of unknown etiology in more than 20 countries and regions around the world?
On May 13, 2022, a new article published in The Lancet Gastroenterology & Hepatology, a sub-journal of The Lancet, believes that this may be related to the super-high disease caused by the new coronavirus. Antigen related.
Unexplained acute hepatitis in children may be related to COVID superantigens
The authors are Petter Brodin , Professor, Department of Immunology and Inflammation, Imperial College London , and Moshe Arditi , Department of Paediatrics, Infectious Diseases and Immunology, Cedars Sinai Medical Center, Los Angeles, California, USA .
What are superantigens?
The aforementioned studies have shown that children infected with the new coronavirus can lead to the formation of virus reservoirs in the body.
Specifically, the persistent presence of SARS-CoV-2 in the gastrointestinal tract of children can lead to the repeated release of viral proteins in intestinal epithelial cells, resulting in immune activation.
This repeated immune activation may be mediated by a superantigen motif in the spike protein of 2019-nCoV, which is similar to staphylococcal enterotoxin B and triggers broad and nonspecific T cell activation.
This superantigen-mediated activation of immune cells has been suggested to be the mechanism behind Multisystem Inflammatory Syndrome in Children (MIS-C) .
The so-called super antigen (SAg) is a kind of substance that can activate a large number of T cell clones and generate a strong immune response with only a very low concentration (≤10-9 times M).
Compared with ordinary antigens, superantigens do not require conventional intracellular antigen presentation and have no MHC restriction.
According to the different activated cells, superantigens can be divided into T cell superantigens and B cell superantigens, and according to their different sources, T and B cell superantigens are divided into endogenous (viral) superantigens and exogenous ( viral) superantigens. bacterial type) superantigens.
Multisystem inflammatory syndrome in children began to receive widespread attention as early as April 2020. At that time, the world had just entered the COVID-19 pandemic, and many countries successively reported a “strange disease of children”, which was highly related to the COVID-19 virus infection.
Most patients had fever, rash, vomiting, swollen neck lymph nodes, chapped lips and Symptoms such as diarrhea, which are similar to those of Kawasaki disease, are also known as Kawasaki-like disease.
Multisystem inflammatory syndrome in children mostly occurs 2-6 weeks after COVID-19 infection, and the age of onset children is concentrated between 3-10 years old.
Multisystem inflammatory syndrome in children is different from Kawasaki disease, and the disease is more severe in children who are serosurveilled positive for COVID-19s.
Multisystem inflammatory syndrome in children can cause inflammation of multiple organs including the heart, lungs, kidneys, brain, skin, eyes or stomach, liver, etc.
In severe cases, it can lead to multiple organ failure, and then lead to the death of children.
Acute hepatitis has also been previously reported in children with multisystem inflammatory syndrome, but co-infection with other viruses has not been investigated , the team said .
The researchers analyzed that the recent acute hepatitis of unknown cause in children may have been infected with the new coronavirus first, and the children were infected with adenovirus after the virus reservoir appeared in the intestine.
Specifically, as shown in the following figure
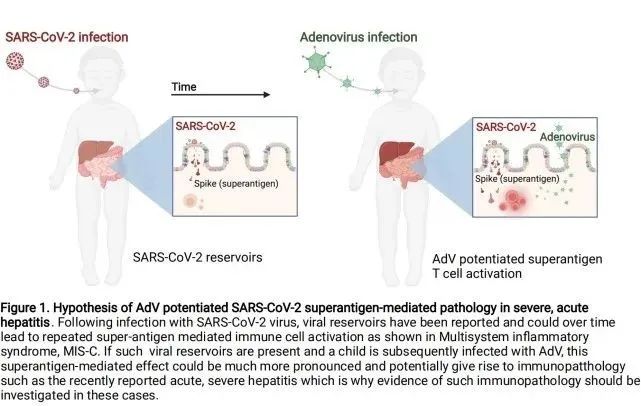 Schematic illustration of the pathology of adenovirus (AdV) enhancing SARS-CoV-2 superantigen-mediated severe acute hepatitis
Schematic illustration of the pathology of adenovirus (AdV) enhancing SARS-CoV-2 superantigen-mediated severe acute hepatitis
Following infection with 2019-nCoV, the viral reservoir may lead to repeated superantigen-mediated activation of immune cells over time, such as multisystem inflammatory syndrome (MIS-C) .
If such reservoirs exist and children are subsequently infected with adenovirus (AdV) , this superantigen-mediated effect may be more pronounced and may lead to immunological abnormalities, as recently reported in acute severe hepatitis, which is why in these Cases should be investigated for evidence of this immunopathology.
The researchers report a similar situation in mouse experiments: Adenovirus infection triggers staphylococcal enterotoxin B-mediated toxic shock, leading to liver failure and death in mice.
This result could be explained by an adenovirus-induced type 1 immune bias, resulting in excess IFN-γ production and IFN-γ-mediated hepatocyte apoptosis following subsequent staphylococcal enterotoxin B administration.
Brodin said that based on the current situation, continuous SARS-CoV-2 surveillance is recommended in the stool of children with acute hepatitis and investigation of T-cell receptor bias and IFN-γ upregulation in children, as this can provide information on SARS-CoV-2 superantigens.
Evidence and mechanisms by which adenovirus 41F sensitizes hosts.
If evidence of SARS-CoV-2 superantigen-mediated immune activation is found, immunomodulatory therapy should be considered in children with severe acute hepatitis.
Adenovirus alone is not enough to cause acute hepatitis in healthy children
The United Kingdom is the country reporting the most cases of acute hepatitis of unknown cause in children this time.
According to the survey information of the UK Health Security Agency (UKHSA) : all the children have undergone nucleic acid testing for the COVID-19, but most of the children have not done serological testing for the COVID-19.
It is worth noting that nucleic acid testing can only determine whether the child was infected with the COVID-19 at the time, and serological testing is required to see whether the child has been infected with the COVID-19 in the past.
The patient also received a whole blood test for adenovirus. However, most children did not do liver biopsy.
In the absence of key information, the UK Health Security Agency put forward the adenovirus-first pathogenic hypothesis.
The British Health Security Agency also stated that the prevention and control of the epidemic in the United Kingdom may reduce the exposure of some young children to common pathogens, resulting in their immune systems developing differently from children of the same age before the COVID-19 epidemic, so the children were easily knocked down by adenovirus.
The hypothesis has been widely questioned by doctors and virologists.
There are two major doubts: first, why no adenovirus inclusion bodies were found in the liver biopsy of the British child; second, why the child’s adenovirus load was so low that the virus samples were not enough for adenovirus genome-wide detection.
Regarding the information currently disclosed in the United Kingdom, Isabella Eckerle , head of the Center for Emerging Infectious Diseases at the University of Geneva, Switzerland, said recently that adenovirus was not detected in liver biopsies of children with acute hepatitis.
If it is caused by adenovirus, the liver should have adenovirus-related pathology.
Deepti Gurdasani , an epidemiologist at Queen Mary University of London, also said that no child in the UK has yet had a liver biopsy showing adenovirus inclusions.
This is the most basic requirement if the hypothesis that adenovirus causes acute hepatitis is true.
The so-called inclusion body refers to the small body visible under the light microscope formed in the host cell after the virus infects the host cell.
In healthy children and adults, adenovirus is generally a self-limiting disease that can cause respiratory, gastrointestinal or conjunctival inflammation, said Farid Jalali , Ph.D., an internist and UC Irvine.
But conditions severe enough to lead to acute liver failure and even death have never been seen in immunocompetent people.
This occurs in people with severe immune deficiency, such as those receiving organ transplants and chemotherapy.
Isabella Eckerle questioned that even if adenovirus was detected in the blood samples presented by the UK Health Security Agency, there was a problem with the low viral load in the blood.
In some cases, the patient’s adenoviral DNA was only present in whole blood and not in plasma. “If acute hepatitis is caused by adenovirus, the virus replicating in the liver should be everywhere: in plasma, serum, biopsies, not just whole blood in most children.”
In fact, the adenovirus Ct values of the children are relatively high, which means that the viral load is relatively low.
Isabella Eckerle said that’s why only some children were able to test for adenovirus gene fragments and found it to be adenovirus type 41.
None of the cases had a viral load high enough for adenovirus genome-wide testing.
Isabella Eckerle wondered: The virus that usually causes hepatitis is abundant in the blood. In clinical hepatitis A, B, and E, the viral load is very high: the situation is relatively different for hepatitis C, but the possibility of hepatitis C virus has been ruled out in all children. Other hepatotropic viruses , such as yellow fever , also have high viral loads.
Viral hepatitis with clinically apparent but low viral load is absent.
“From my perspective as a clinical virologist, there are many arguments against adenoviruses causing acute hepatitis,” says Isabella Eckerle , which has important implications for treatment. Why? This means that whether antiviral therapy or immunosuppressive therapy (eg, cortisol) should be used can have very different effects on a patient’s clinical outcome.
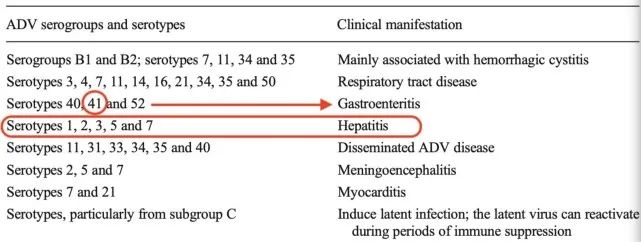
Available data show that the highly suspected adenovirus type 41 mostly causes gastroenteritis, and its main tissue tropism is the gastrointestinal tract, not the liver.
Without showing any abnormal complete genome of adenovirus type 41, Isabella Eckerle said it was hard to believe that the virus would suddenly and completely change tropism, causing severe liver disease in immunocompetent children, something that had never been done before.

Unexplained acute hepatitis in children may be related to COVID superantigens
It is not uncommon to find adenoviruses in healthy children, says Farid Jalali . In 30% of healthy children, the adenovirus can persist for months or even years after being infected with it.
As many as 11% of healthy children have persistent detection of adenovirus in their tonsils and adenoids.
Available data show that the highly suspected adenovirus type 41 mostly causes gastroenteritis, and its main tissue tropism is the gastrointestinal tract, not the liver.
Isabella Eckerle believes that the possibility of acute hepatitis in children after infection with the COVID-19 cannot be ruled out.
COVID-19 serological test shows that 73.7% of children have been infected with COVID-19
Compared with the sloppy testing in the UK, Israel conducted a COVID-19 serological survey on children. The results showed that most of them were infected with the COVID-19.
According to Israel’s “Ha’aretz” and “Jerusalem Post” reports, the country recently reported 12 unidentified cases of hepatitis in children.
Seven cases were reported at Schneider Children’s Medical Center and five cases were reported at Sharazedek Medical Center.
The above cases came from different locations across the country and did not show the characteristics of clustered infection.
The main symptoms are severe liver infection and marked elevation of liver enzymes, usually accompanied by jaundice, and gastrointestinal symptoms in some cases.
At present, these cases have all been discharged.
Among them, 2 cases at Schneider Children’s Hospital underwent liver transplantation due to liver failure, and the remaining cases improved rapidly after receiving steroid drug treatment.
Of the 12 cases identified in Israel, 11 had contracted the virus within a year.
Although there is no clear evidence that the unidentified hepatitis is related to the new coronavirus, several Israeli medical experts have expressed doubts in interviews with the media that there is a link between the two.
Glasberg, director of the Pediatric Liver Transplant Center at Schneider Children’s Medical Center, said that after ruling out all possibilities, all the cases found had in common that they were infected with the new coronavirus about three and a half months before the onset of hepatitis.
Severe COVID-19 infection is known to damage the liver, so this unidentified hepatitis may be one of the long-term symptoms of COVID-19.
The WHO Regional Office for Europe reported on May 13 that unexplained acute hepatitis cases in children aged 16 and under in the region also showed that more than 70% had been infected with the new coronavirus.
A total of 229 children with acute unexplained hepatitis were reported in 14 countries in Europe, including 12 cases in Belgium, 2 cases in Cyprus, 6 cases in Denmark, 2 cases in Greece, 6 cases in Ireland, 24 cases in Italy, 6 cases in the Netherlands, 5 cases in Norway, 1 case in Poland, 1 in Serbia, 1 in Slovenia, 26 in Spain, 9 in Sweden and 131 in the UK.
75.9% of cases were younger than 5 years old. Of the 143 cases with relevant medical progress information, 22 are in the intensive care unit, accounting for 15.4%.
Six of the 98 cases with transplant-related information received liver transplantation, a rate of 6.1%. 1 person has died.
Of the 151 children who were tested for adenovirus in all samples, 90, or 59.6%, tested positive. Among them, the positive rate of whole blood samples was the highest at 68.9%.
Of the 173 children who received the nucleic acid test for the new coronavirus, 20 were positive, accounting for 11.6%.
Only 19 children had serological tests for the new coronavirus, of which 14 were positive, or 73.7%. Of the 56 cases for which COVID-19 vaccination data were available, 47 (83.9%) were not vaccinated.
In fact, with the global pandemic of the Omicron variant, a large number of children overseas have been infected with the COVID-19.
According to Nature ‘s report, as of February 2022, nearly 70% of children aged 1-4 in the United States were positive for COVID-19 antibodies.
Most children aged 1-4 have not been vaccinated, so the high probability of antibody positivity is caused by infection with the COVID-19.
Isabella Eckerle expressed concern that allowing a new virus like Covid-19 to spread uncontrollably in children, especially young children who are largely unvaccinated, and that research on the long-term sequelae of Covid-19 is not clear, this kind of laissez-faire infection is a very dangerous idea.
Reference:
https://www.thelancet.com/journals/langas/article/PIIS2468-1253(22)00166-2/fulltext
Unexplained acute hepatitis in children may be related to COVID superantigens
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



