Why did the immunity against Omicron of people infected with the original strain decrease?
- Did Cloud Seeding Unleash a Deluge in Dubai?
- News draftScientists Identify Gut Bacteria and Metabolites that Lower Diabetes RiskNews draft
- OpenAI’s Model Matches Doctors in Assessing Eye Conditions
- UK: A Smoke-Free Generation by Banning Sales to Those Born After 2009
- Deadly Mutation: A New Monkeypox Variant Emerges in the DRC
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
Why did the immunity against Omicron of people infected with the original strain decrease?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Why did the immunity against Omicron of people infected with the original strain decrease? The study is becoming more controversial!
Science published a paper titled Immune boosting by B.1.1.529 (Omicron) depends on previous SARS-CoV-2 exposure.
After the release of this study, it caused a lot of professional discussions and concerns
Among them, an uncommon immunological concept is repeatedly mentioned – antigenic SIN.
What the latest research says?
Before talking about “Original Sin”, let’s take a look at what the latest research from Science has to say.
Researchers from the UK followed a group of medical workers who had received three doses of the mRNA Covid-19 vaccine and monitored their immune responses.
The research content is roughly divided into two parts.
In the first part, the researchers followed individuals who had no natural history of infection, were infected with the original strain (Wuhan Hu-1, the same below) , were infected with the Alpha mutant, and were infected with the Delta mutant. These people were all vaccinated with three doses of the mRNA COVID-19 vaccine.
Source: Reference 1
The researchers then observed the immune recognition of different mutant strains in the four populations: at different time points, such as after the second dose and after the third dose, blood samples were drawn to analyze the neutralization of each virus strain. In the case of immune recognition such as antibodies, memory B cells, and T cells.
The results showed that after three injections of the vaccine, Omicron had the weakest immune recognition of each mutant strain, such as the lowest neutralizing antibody titer.
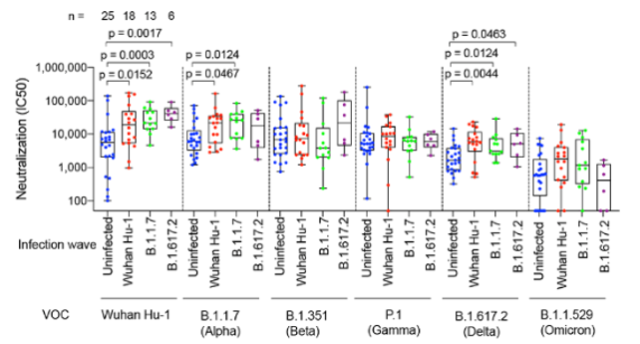
Source: Reference 1
This finding is not unexpected. In fact, due to the serious immune escape, many previous studies have shown that Omicron has always been the lowest titer in the serum neutralization of each mutant strain by vaccine recipients.
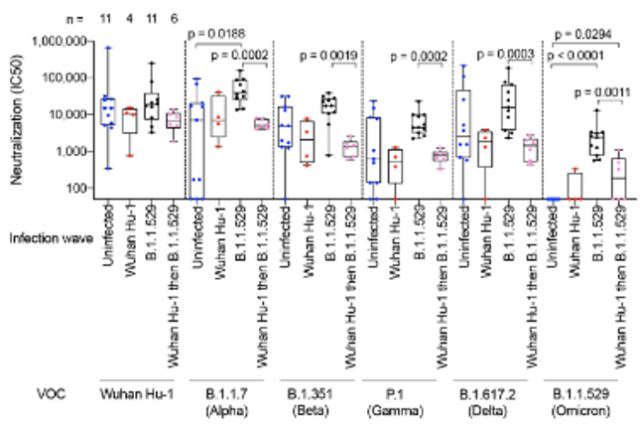
More innovative is the second part of the study : The researchers looked at people who had a history of infection with various mutant strains and received three shots of the vaccine and were eventually infected by the Omicron breakthrough to see how different immune backgrounds affected Omicron infection. immune response.
 Source: Reference 1
Source: Reference 1
Why did the immunity against Omicron of people infected with the original strain decrease?
And the result that worries many people also comes from this part.
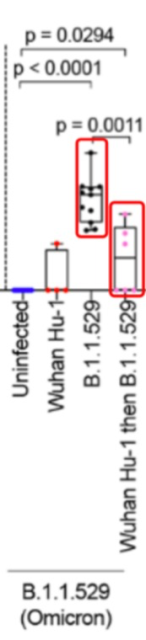
 Source: Reference 1
Source: Reference 1
Why did the immunity against Omicron of people infected with the original strain decrease?
The study compared four different immune backgrounds: the first was uninfected, the second was infected with the original strain, the third was infected with Omicron, and the last was infected with the original strain in the past and then re-infected with Omicron Infect.
All groups were vaccinated with three doses of the mRNA COVID-19 vaccine.
According to the results of the study, the neutralizing antibodies against Omicron were significantly improved after inoculation with three doses of mRNA COVID-19 vaccine and re-infection with Omicron . strains to increase.
However, after the three-needle mRNA COVID-19 vaccine, people who had been infected with the original strain in the early stage, after re-infection with Omicron, had a certain increase in neutralizing antibodies against Omicron compared with those who were uninfected or only infected with the original strain, but they still need to be infected. significantly lower than those who had not been infected with the original strain and were only infected with Omicron.
Source of some screenshots of the
above image: Reference 1
The infection history of the original strain appears to “interfere” with the induction of the body’s normal immune response to Omicron infection.
After the paper was published, this phenomenon immediately sparked a lot of discussions and concerns: Could it be that a person who has been infected with the COVID-19 not only did not acquire a certain degree of immunity when facing Omicron, but the immune response was even stronger than that of a person who had not been infected? weak?
New antigens activate old immunity
Why is there such a situation? Here we will return to the immunological concept we mentioned at the beginning.
Original antigenic sin (original antigenic sin), also known as immune imprinting, refers to the preferential activation of the immune system when it encounters a similar but slightly different neoantigen after establishing an immune memory for an antigen. Immune response to the original antigen.
However, there are still some differences between the new antigen and the original antigen itself. Therefore, such an immune response “influenced” by the original antigen is not “optimal” when dealing with the new antigen, so there is a saying of “original sin”.
The concept of antigenic sin was first proposed in influenza.
Influenza is also a virus with a very high mutation rate. In the 1960s, some scientists proposed that the human body’s antibodies against influenza mainly depend on the influenza virus strain that was first contacted.
When re-infected later, even if the virus strain has been mutated due to ” Antigen drift”, which is different from the original virus strain, and the immune response generated by the human body is still mainly directed against the first contacted influenza virus strain.
The origin of antigenic sin phenomenon is rooted in the characteristics of immune memory itself.
Take antibodies as an example. Antibodies are produced by B cells against a specific antigen after maturation. If an antigen is completely new and the human body has never been exposed to, naive B cells (Naive B cells) are stimulated, and the latter, by recognizing the antigen, are finally transformed into mature B cells that can produce specific antibodies, as well as memory B cells.
Memory B cells do not produce antibodies, but they can recognize this antigen. Once they encounter the antigen again, they can rapidly differentiate into plasma cells and produce a large number of specific antibodies.
Stimulation of memory B cells was faster and stronger than stimulation of naive B cells, both in terms of the speed of the immune response (e.g., the time it took from exposure to the antigen to the production of antibodies) and the strength of the immune response (e.g., the total amount of antibodies produced).
This is why, after the immune memory is established, the body can clear it faster when it encounters pathogens again, because at this time, memory B cells are mainly activated, and naive B cells are no longer stimulated from scratch.
However, if the antigens encountered again are different from the antigens that established the immune memory in the first place, then the immune memory may be “disadvantaging”.
For example, after encountering a neoantigen, if the original memory B cells are preferentially stimulated at this time, the antibodies produced are not so effective against the neoantigen, but because a large number of antibodies have been formed, the neoantigen cannot effectively stimulate the naive B cells.
Therefore, the final effect of the immune response may not be as good as the direct stimulation of naive B cells to form more targeted antibodies without prior immune memory.
Not only the humoral immunity represented by B cells, but also the cellular immunity represented by T cells also has the phenomenon of antigenic original sin.
The actual effects of antigenic sin vary by pathogen : are only memory B cells stimulated, or are memory B cells preferentially stimulated but a fraction of new naive B cells can be activated? Are antibodies against past antigens completely ineffective against new antigens, or are they still useful? These differences will affect the ultimate impact of the original sin.
Up to now, antigenic sin has been considered to be related to dengue virus, influenza virus, and HIV virus.
A possible example is the H1N1 Spanish flu pandemic of 1918, when age-specific mortality rates peaked in the 28-year-old.
The corresponding birth year for this age group was 1980, which was the time of the H3Nx Russian flu pandemic.
It is speculated that the peak mortality rate at age 28 is due to the strong immune memory of H3Nx in this age group in early childhood, and after more than two decades, when exposed to H1N1 again, the new antigen Old immunity is activated, but the resulting immune response is not well protected against H1N1, thus increasing the risk of death.
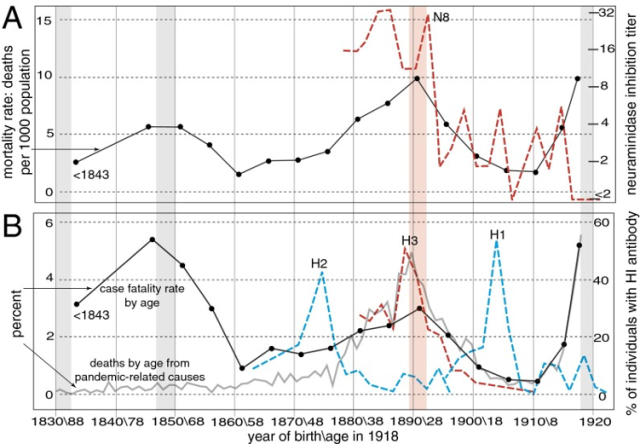 Source: Reference 14
Source: Reference 14
Why did the immunity against Omicron of people infected with the original strain decrease?
Another more specific example is dengue fever.
There are four main serotypes of dengue virus. As long as you have been infected with one of these serotypes, or if you are vaccinated with a virus of one serotype, the antigenic sin response is strong enough to encounter any other serotype in the future, and the antibodies produced are directed against the original serotype. , but not for other serotypes.
Not only that, dengue virus also has a phenomenon called ADE. That is, when there are antibodies against one serotype in the body, these antibodies are not only ineffective against other serotypes of dengue virus, but the latter can also use these ineffective antibodies to infect immune cells and cause more damage.
Because of the original sin and ADE, the development of dengue vaccine has been difficult, and only a vaccine that can target all four serotypes at one time can protect.
While successful vaccines are now available, they are limited to target populations who have laboratory confirmed previous dengue infection and who live in endemic areas.
After the latest study of Science has attracted attention, some people have also proposed that such data results do not mean the original sin of the antigen but point to ADE?
In fact, this view does not correspond to reality.
In principle, ADE requires that viruses can use non-neutralizing antibodies to invade human cells and cause more damage after entering cells in this way.
So far, this phenomenon has not been observed with new coronaviruses.
More importantly, we have observed that after secondary infection and vaccination, even if encountering a new mutant strain, the immune memory still brings a very good anti-severe effect.
If ADE occurs, reinfection should lead to more severe disease.
Decreased immune response ≠ immune failure
What changes will the original sin of antigen bring to the COVID-19? What impact will it have on us?
In fact, an antigenic sin phenomenon like dengue is very extreme.
After the publication of this latest study by Science , some interpretations on the Internet also mistakenly regard the extreme phenomenon of dengue fever as common, and mistakenly believe that as long as there is evidence that the COVID-19 has an antigenic sin, it means that all previous infections and vaccinations are ineffective.
In fact, as we mentioned earlier, antigenic sin may vary in degree between different pathogens, and it may only affect the degree of immune response, rather than make the immune response completely ineffective.
A study that analyzed the immune response to the 2009 H1N1 pandemic influenza vaccine found that the increase in antibodies to H1N1 influenza was smaller if the seasonal influenza vaccine was received within three months before the vaccine was given ——This is also a certain degree of antigenic sin effect.
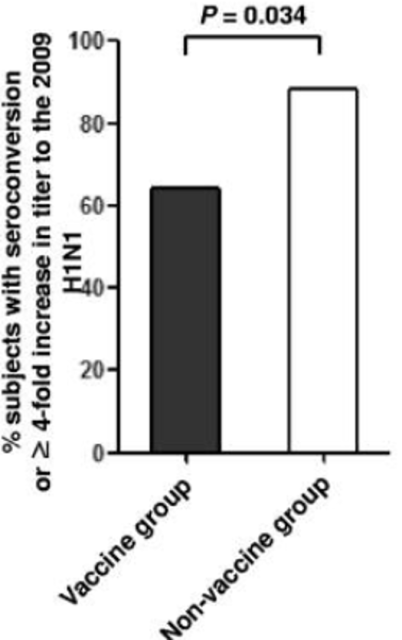 Source: Reference 5
Source: Reference 5
However, the study also showed that more than 60% of subjects who received the seasonal flu vaccine also had a more than four-fold increase in antibodies against the H1N1 strain after receiving the H1N1 vaccine.
Although it is not as good as more than 80% of those who have not received the seasonal flu vaccine, it does not mean that the H1N1 vaccine is ineffective because of the seasonal flu vaccine.
The same is true for the latest paper in Science . From the results of the study, past natural infections did lead to differences in the immune recognition of each mutant strain after the same three doses of vaccines, especially for Omicron, which is different from the previous virus strains.
Mutant strains with particularly large differences. And this situation does point to the fact that past infection of the COVID-19 may have a potential antigenic sin phenomenon.
However, what we cannot ignore is that there is more evidence that the severe protection of Omicron from past infection and vaccination is still good.
For example, a study in Qatar found that the protective effect of past infection on symptomatic Omicron was 46.1%, On the basis of past infections, the three-injection mRNA vaccine was administered, and the effectiveness increased to 77.3%.
At the same time, some studies have shown that the breadth of the body’s immune recognition of the COVID-19 is also increased after vaccination, and this process will continue for several months after vaccination.
A paper on Cell showed that although the neutralizing antibody titer decreased over time after inoculation with two mRNA vaccines, the neutralizing ability of the neutralizing antibody itself increased over time .
After the third booster injection, those memory B cells that can recognize various mutant strains, including Omicron, are rapidly activated again, producing a large number of antibodies with very high neutralization efficiency:
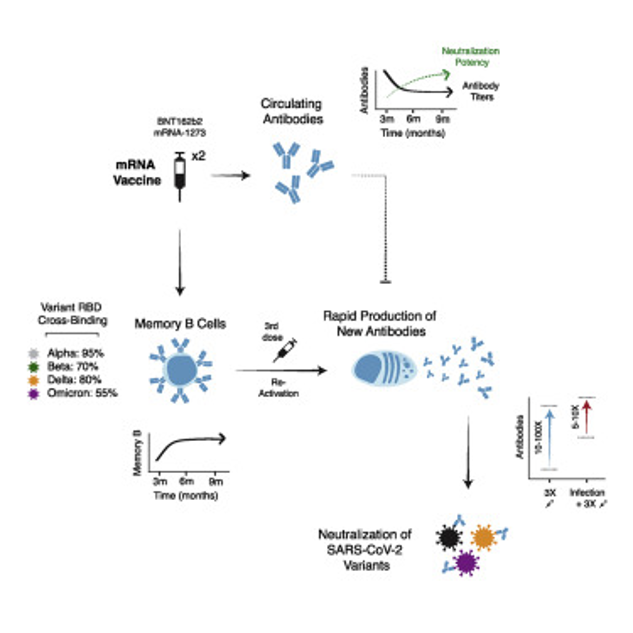 Source: Reference 7
Source: Reference 7
Another paper studying the changes of memory B cells after breakthrough infection in Omicron found that after breakthrough infection, the response of memory B cells is also very particular about “strategy”, mainly expanding those that recognize the conserved regions of each mutant strain. memory B cells.
The above studies corroborate each other: the human body’s immune recognition of the COVID-19 is highly flexible, and even if the initial contact antigen is the original virus strain or a mutant strain, the final immune memory can have a good breadth.
Therefore, it would be an exaggeration to say that the COVID-19 vaccine is therefore ineffective or that previous infections have no immune protection at all.
Will a vaccine against Omicron still work?
Some people also expressed concern: if the original virus is infected with Omicron after infection, and the human body is immune to the phenomenon of antigenic sin, then, if people who have been vaccinated with the original strain are vaccinated against the vaccine designed for Omicron, will there be similar Happening? Will the Omicron vaccine still protect?
To discuss this issue, we must first define what the so-called “protective effect” is? Is it to prevent infection or reduce severe disease?
It is indeed difficult to prevent infection, and it does not even need to involve the concept of antigenic sin. Judging from the replacement of multiple mainstream mutants, one of the characteristics of the new dominant mutants is that the infectivity is getting stronger and the incubation period is getting shorter and shorter.
A shorter incubation period means that the time from exposure to the virus to infection is shorter, and the time left for the body to activate immune memory is also shorter.
The median incubation period of Omicron is 3 to 4 days. With such a short incubation period, preventing infection requires very high titers of neutralizing antibodies in the body’s first line of contact with the virus, such as the respiratory tract.
But at present, this may not be possible or long-term maintained by existing vaccines or natural infections, because antibody titers will naturally decline over time.
For protection against severe disease, current evidence suggests that even a vaccine designed against the original strain still has very good or even very durable protection against severe immune evasion mutants such as Omicron.
So, can the Omicron version of the vaccine be further improved on this basis?
Judging from some of the latest vaccine development progress, Omicron as an antigen can still further improve the immune response.
In mouse trials, the Omicron version of Moderna’s COVID-19 vaccine induced more neutralizing antibodies against Omicron than the original version.
Interestingly, the Omicron version of the vaccine does not have many neutralizing antibodies against other mutants if it is used as a basic immunization, but it does not have this problem as a booster.
Before Moderna’s Omicron vaccine had no advantage over the original version in rhesus monkeys, many people also suggested that this was the original sin of the antigen.
However, in follow-up mouse experiments, the researchers found that the Omicron version did not have an advantage when using high-dose vaccines, but at low doses, the Omicron version of the vaccine as a booster showed better recognition breadth.
This actually reminds us that each study has its own special experimental conditions, and the conclusions of a study should not be overstated.
Combining the conclusions in animal models, for unvaccinated people, direct use of the Omicron version of the vaccine to deal with Omicron may be OK, but it may not provide better protection for other mutant strains.
This means that a multivalent vaccine may be a better option, such as combining the Omicron version with the original vaccine.
Recently, Moderna announced the results of a booster clinical trial of such a bivalent vaccine. The test showed that using the bivalent vaccine of the “original version + Omicron version” as a booster, Omicron had significantly more neutralizing antibodies than the original vaccine:
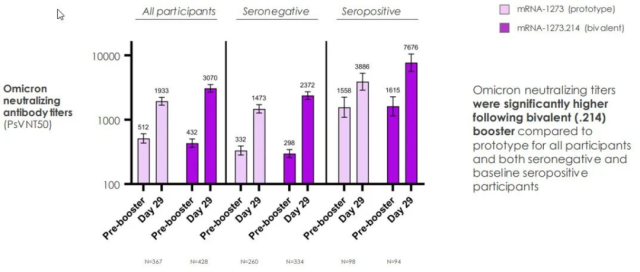 Source: Reference 12
Source: Reference 12
Note that for those with a history of past infection (ie, seropositive in the figure), the neutralizing antibody against Omicron also increased significantly after receiving the bivalent vaccine, and due to the enhanced vaccination effect of the original vaccine.
Therefore , the Omicron version of the vaccine now has a lot of evidence that it is feasible, and even if there is a history of past infection, it does not affect its effect.
On June 17, the WHO recommended that after the basic immunization of the existing vaccine is completed, the Omicron version of the vaccine can be used as a booster after studying the data of Omicron infection and the development of the Omicron version of the vaccine.
Returning to the latest Science research itself, the main question this paper attempts to explore is actually “how past infections and vaccinations shape an individual’s immune response.”
Concerning phenomena such as antigenic sin, we should not magnify a single study to the overall real-world vaccine effectiveness and protection from natural infection.
At the same time, the study has a limited sample size and limited persuasiveness.
Moreover, in the level of neutralizing antibodies against Omicron, although the former infected with the original strain and re-infected with Omicron were weaker than those infected with only Omicron, they were also higher than those without a history of infection or only infected with the original strain.
Taken together, vaccination with Omicron may provide additional protection against Omicorn, regardless of previous infection history.
Does the COVID-19 really exist antigenic sin? What is the degree of antigenic original sin and what are the effects? It also requires a large number of immunological studies, vaccine effectiveness tracking and other data to verify.
These studies will help us gain a more nuanced understanding of how the immune system responds to the new coronavirus, which in turn will inspire the design of broader and more effective vaccines.
References:
[1] https://www.science.org/doi/10.1126/science.abq1841
[2] https://www.nejm.org/doi/full/10.1056/NEJMoa2203965
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3014204/
[4] https://www.fda.gov/vaccines-blood-biologics/dengvaxia
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3165229/
[6] https://www1.racgp.org.au/newsgp/clinical/how-does-omicron-compare-with-delta
[7] https://www.cell.com/cell/fulltext/S0092-8674(22)00456-1
[8] https://www.science.org/doi/10.1126/sciimmunol.abq2427
[9] https://www.cell.com/cell/fulltext/S0092-8674(22)00329-4
[10] https://www.cell.com/cell/fulltext/S0092-8674(22)00387-7
[11] https://www.sciencedirect.com/science/article/pii/S0092867421014057
[12] https://s29.q4cdn.com/435878511/files/doc_presentations/2022/06/08/Master-Final-Bivalent-Omicron-Data-Update-0608.pdf
[13] https://www.who.int/news/item/17-06-2022-interim-statement-on–the-composition-of-current-COVID-19-vaccines
[14] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4050607/
Why did the immunity against Omicron of people infected with the original strain decrease?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



