What is Tumor Bacterial Immunotherapy?
- EPA Announces First-Ever Regulation for “Forever Chemicals” in Drinking Water
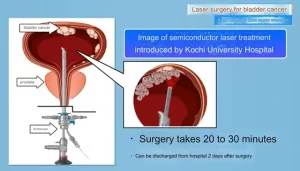
- Kochi University pioneers outpatient bladder cancer treatment using semiconductor lasers
- ASPEN 2024: Nutritional Therapy Strategies for Cancer and Critically Ill Patients
- Which lung cancer patients can benefit from neoadjuvant immunotherapy?
- Heme Iron Absorption: Why Meat Matters for Women’s Iron Needs
- “Miracle Weight-loss Drug” Semaglutide Is Not Always Effective
What is Tumor Bacterial Immunotherapy?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What is Tumor Bacterial Immunotherapy?
In recent years, immunotherapy using drugs to reactivate or enhance immune surveillance has emerged as a new and promising cancer treatment strategy. In 2011, ipilimumab, a CTLA-4 blocking antibody, was approved for advanced melanoma, ushering in a new era of immunotherapy.
Antibodies against a series of other checkpoints, such as PD-1, PD-L1, and LAG-3, are also widely developed and approved for various cancer treatments, which have significantly improved the survival rate of advanced cancer patients in some clinical practices.
However, the “cold” tumor microenvironment ( TME ) characterized by the absence or depletion of infiltrating immune cells impairs immune checkpoint blockade therapies, necessitating the development of improved immunotherapy strategies.
Bacteria have long been used as drugs to treat cancer, dating back to the origins of modern immunotherapy.
William Coley injected heat-killed Streptococcus and Serratia marcescens ( known as Coley’s toxin ) into malignant tumor tissue in the nineteenth century and observed tumor regression.
Therefore, William Coley is known as the father of immunotherapy.
Another successful example of bacterial immunotherapy is Bacillus Calmette-Guerin ( BCG ), an attenuated mutant strain of Mycobacterium bovis, originally designed as a tuberculosis vaccine and approved by the FDA in 1990 for the treatment of bladder cancer.
In recent years, studies have also demonstrated the presence of intratumoral bacteria and the immunomodulatory role of the microbiota, suggesting that tumor tissue is a complex of bacteria interacting with tumor cells and the host.
Bacteria are involved in almost all biological aspects of cancer. Today, with the in-depth understanding of TME and the rapid development of microbiology, nanotechnology and recombinant DNA technology, the realization of reprogrammed bacteria makes bacterial therapy a new hot spot in current cancer research and treatment .
Bacteria’s natural advantage
Bacteria have tumor-targeting properties, and their surface structures or metabolites can also activate the immune system to exert anti-tumor effects.
Therefore, bacteria have inherent advantages as therapeutic agents or carriers in tumor immunotherapy.
Tumor targeting of bacteria
The vasculature in tumor tissue is often chaotic and irregular, resulting in insufficient diffusion of oxygen and nutrients.
Therefore, the central region of the tumor often presents a hypoxic environment.
The study found that this central area could provide a site for the colonization and proliferation of some obligate and facultative anaerobic bacteria after systemic administration.
It has been reported that 3 days after intravenous injection of Salmonella typhimurium, the ratio of bacterial counts in tumor sites to normal organs in mice exceeded 10000:1.
In contrast, traditional chemotherapeutics, which rely only on passive distribution and limited penetration, are difficult to access these sparsely vascular necrotic regions through systemic administration, which often leads to tumor recurrence.
As a result, the bacteria are able to colonize the tumor core, an area that is most difficult to target for other types of drugs.
Immune activating properties of bacteria
Hypoxia, a hallmark of the TME, also leads to functional suppression of local immune cells. As tumors progress, the uncontrolled proliferation of cancer cells deprives immune cells of oxygen and nutrients.
As a result, immune cells tend to become exhausted, assume a suppressive phenotype by secreting cancer-promoting cytokines and chemokines, and fail to respond to anticancer signals.
However, bacteria-derived molecules such as peptidoglycan, lipopolysaccharide ( LPS ), and lipoteichoic acid can provide powerful immunostimulatory signals.
They mainly bind to pattern recognition receptors ( PRR ) expressed by innate immune cells, such as dendritic cells ( DC ) and macrophages, to induce the migration of immune cells and stimulate the immune system to recognize and kill tumor cells.
For example, Salmonella LPS can increase the expression of IL-1β and exert anti-tumor effects through inflammasome and Toll-like receptor 4 ( TLR4 )-mediated signaling pathways.
As the structure of some Gram-negative bacteria, flagella can promote the expression of various pro-inflammatory cytokines, NO, H2O2 and chemokines by binding to Toll-like receptor 5 ( TLR5 ) on dendritic cells , and enhance the expression of CD8 + T cell-mediated tumor killing, and down-regulate the suppressive function of Treg cells.
In addition, certain components of bacteria can mediate phenotypic transformation of immune cells.
For example, flagellin can mediate the transformation of tumor-promoting macrophages into anti-tumor macrophages, converting an immunosuppressive microenvironment into an immunocompetent environment.
The study found that Listeria can infect MDSCs, reduce the content of MDSCs in the blood, and promote the secretion of IL-12 by the remaining MDSCs, transforming into an immune active phenotype.
Reduced tumor growth was observed in Listeria-treated animal models, suggesting that Listeria can suppress tumors by acting on MDSCs.
Engineered bacteria
Chemotactic colonization of tumor sites by bacteria and their immunogenicity make them ideal candidates for immunotherapy.
It has been reported that several bacteria were detected in tumor tissues, and intratumoral delivery of probiotics can promote anti-tumor immunity, providing a theoretical basis for the application of microorganisms in tumor therapy.
Bacterial engineering has become possible in recent years with the development of synthetic biology, materials science, and gene editing tools. Through different modification and transformation methods, the targeting, therapeutic effect and safety of tumors can be further improved.

Engineering to improve tumor propensity
Construction of auxotrophic mutants is a strategy to improve bacterial targeting. Based on the differences in the nutrients contained in normal tissue and tumor sites, mutants can be engineered to colonize and survive only in tumor tissue.
Among them, Salmonella A1 and SF104 are examples of successful application. Salmonella A1 is an auxotrophic strain for leucine and arginine, while Salmonella SF104 exhibits a requirement for aromatic amino acids with a mutation in the gene aroA, both of which prevent the bacteria from enriching in normal tissues, However, it can specifically accumulate at tumor sites.
In addition, synthetically engineered adhesins, specifically designed to bind specific cancer-expressed molecules, such as neoantigens or other molecules abundant in cancer cells, could enhance the natural affinity of certain bacteria for tumors.
Bereta et al. observed increased bacterial accumulation at tumor sites by expressing a specific single-chain antibody fragment of carcinoembryonic antigen ( CEA ) on Salmonella typhimurium VNP20009 .
In another study, by conjugating an anti-CD20 antibody to the surface of Salmonella, the invasiveness of the bacteria against CD20+ lymphomas was increased while non-specific aggregation was reduced.
Engineering to regulate the immune microenvironment
Several basic components of bacteria are capable of altering the body’s immune system. However, in order to obtain greater immunomodulatory effects, engineered bacteria can be designed to load or express exogenous immunotherapeutic drugs to enhance antitumor efficacy.
Given that bacteria preferentially colonize malignant areas and naturally stimulate innate immune cells, bacteria-based therapy could provide a baseline level of immune activation in tumor tissue.
Cytokines have the ability to promote the activation and proliferation of immune cells, and the delivery of cytokines through engineered bacteria has the characteristics of high specificity and small side effects.
A study synthesized IL-18 by using attenuated Salmonella typhimurium, by increasing the infiltration of CD3+/CD4+ T cells and DX5+ NK cells in the tumor area, IL-1β, TNF-α, IFN-γ, GM-CSF, etc. The expression of cytokines was increased, and an antitumor effect was observed.
Human papillomavirus type 16 oncoprotein E7 ( HPV-16 E7 ) plays a key role in the pathogenesis of cervical cancer and is required for host cellular immunity.
Oral administration of Lactobacillus expressing HPV-16 E7 protein has been reported to lead to a significant delay in the growth of E7-expressing tumors and a significant increase in the number of E7-specific CD4+ T helper cells and CD8+ T cells, suggesting that this bacterium-based vaccine is effective against tumors.
Cell challenge has profound protective effects. The oral vaccine also underwent a Phase 1 clinical trial to verify its safety and immunogenicity.
Engineered to improve safety
Although bacteria possess promising antitumor properties, their potential toxicity is a major obstacle to their application. On the other hand, the safety of live bacterial preparations is the key to its clinical transformation.
In order to make full use of bacteria to fight cancer, researchers have made great efforts to construct a large number of attenuated engineered bacteria to improve their safety performance.
Bacterial surface molecules are responsible for the major virulence of bacteria, and modification of these surface antigens (such as gene knockout) is the main way to evade the virulence of live pathogens.
For example, ppGpp (guanosine 5′-diphosphate-3′-diphosphate) is a signaling molecule involved in the expression of virulence genes.
By knocking out the relA and spoT genes, the synthesis of ppGpp was blocked, resulting in a 10 5 -10 6 -fold increase in its LD50 compared to the wild strain.
Due to the ability to induce the secretion of pro-inflammatory factors IL-1β, IL-18 and TNF-α, bacteria with disordered ppGpp synthesis also exhibited good antitumor activity.
Research status of engineering bacteria in tumor combined immunotherapy
Studies have shown that bacteria can act as immunotherapeutic agents to enhance anti-tumor immunity.
As combination therapy is a widely used strategy to improve overall efficacy, bacterial immunotherapy has also been used as part of combined chemotherapy, radiotherapy, photodynamic therapy, and photothermal therapy.
Combination chemotherapy
Conventional chemotherapy lacks specific delivery to malignant tissues, resulting in significant systemic drug exposure, which often produces dose-limiting toxicities. The use of engineered bacteria as a drug release system for controlled release of drugs and the use of their immunogenicity for immune regulation have become research hotspots.
Ektate et al. attached cryo-sensitive liposomes to Salmonella membranes to mediate the triggered release of doxorubicin in colon cancer cells with the help of high-intensity focused ultrasound ( HIFU ) heating, resulting in the cytoplasm and nucleus of cancer cells achieve efficient drug delivery.
In addition, this strain polarized macrophages to an antitumor M1 phenotype, enriched Th1 cell populations with high levels of TNF-α, and decreased IL-10 expression, thereby showing enhanced efficacy in combination chemotherapy-immunotherapy modalities. treatment effect.
In addition to utilizing live bacteria, bacterial outer membrane vesicles ( OMVs ), which are naturally produced from Gram-negative bacterial membranes during growth, have recently emerged as immunotherapeutic agents for a variety of biomedical applications.
Chen et al. encapsulated drug-loaded polymer micelles into bacterial outer membrane vesicles. Bacterial components can activate immune responses, and loaded drugs can exert chemotherapeutic and immunomodulatory effects to clear cancer cells.
Combined radiotherapy
Bacteria-assisted radiation therapy is a new approach to cancer treatment. In a study by Jiang et al., investigating the therapeutic effect of E. coli in combination with radiation therapy, it was shown that tumors in a colon tumor model shrank significantly in the presence of 21 Gy of radiation and E. coli producing cytolysin a. Cytolysin-a-carrying bacteria combined with radiotherapy resulted in more tumor remissions than bacteria alone.
In addition, after radiotherapy, tumors release large amounts of tumor antigens that can be taken up and presented by dendritic cells, leading to specific adaptive immune responses.
However, in an immunosuppressive TME, the number of DCs is usually low and they are often in a dysfunctional state. Wang et al. injected Salmonella into tumor tissue coated with antigen-adsorbing cationic polymer nanoparticles, which can capture antigens released after radiotherapy and transport them out of the tumor core, thereby activating peripheral DCs in tumor margin tissue.
Studies have observed a large increase in activated DCs in vitro, prolonged survival in multiple tumor mouse models, and demonstrated enhanced systemic anti-tumor effects.
Combined photodynamic therapy and photothermal therapy
Due to the non-specific killing effect and complicated surgical operation of standard tumor therapy, photodynamic therapy and photothermal therapy have become new treatment options due to their non-invasiveness, high specificity, and good spatiotemporal control.
Recently, many studies have attempted to use bacteria as carriers to load therapeutic agents for PDT and PTT to take advantage of the tumor-targeting and immune-activating properties of bacteria.
One study incorporated photosensitizer-coated nanoparticles onto the surface of the photosynthetic bacterium Synechococcus sp.
Under 660nm laser irradiation, photosynthetic bacteria continue to produce oxygen, which ensures the production of active oxygen and enhances the effect of photodynamic therapy.
Synechococcus, as an immunogenic bacterium, also activates local immunity by upregulating the expression of MHC class II molecules and IL-12.
Simultaneously, this therapeutic approach induced immunogenic apoptosis by upregulating cell surface calreticulin, and showed good therapeutic effect in a triple-negative breast cancer model.
Summary
Since the first trials of BCG as a bladder cancer drug, there has been a relentless effort to study the role of BCG in the treatment of cancers other than bladder cancer.
In addition to BCG, other bacterial preparations, such as modified strains of Salmonella typhimurium, are also in preclinical or clinical trials to better verify their safety and therapeutic effects.
Because bacteria are complex and viable therapeutics, some uncontrolled mutations during their proliferation could bring about potential toxicity.
Their inherent virulence can also lead to complicated infections in immunocompromised cancer patients.
However, the rapid development of synthetic biology makes it possible to obtain the desired bacterial behavior through gene editing.
Relying on the precise regulation of the targeting of engineered bacteria, the specific release of drugs at tumor sites can be achieved.
In the future, engineered bacteria will become The strong support of tumor immunotherapy has benefited more cancer patients.
references:
1. Current Status and Future Directions of Bacteria-Based Immunotherapy. Front Immunol. 2022; 13: 911783.
What is Tumor Bacterial Immunotherapy?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.