Post-resuscitation Care: 2021 ERC and ESICM guidelines
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Post-resuscitation Care: 2021 ERC and ESICM guidelines
Post-resuscitation Care: 2021 ERC and ESICM guidelines. Post-resuscitation Care: 2021 guidelines of the European Resuscitation Council and the European Society of Intensive Care Medicine.
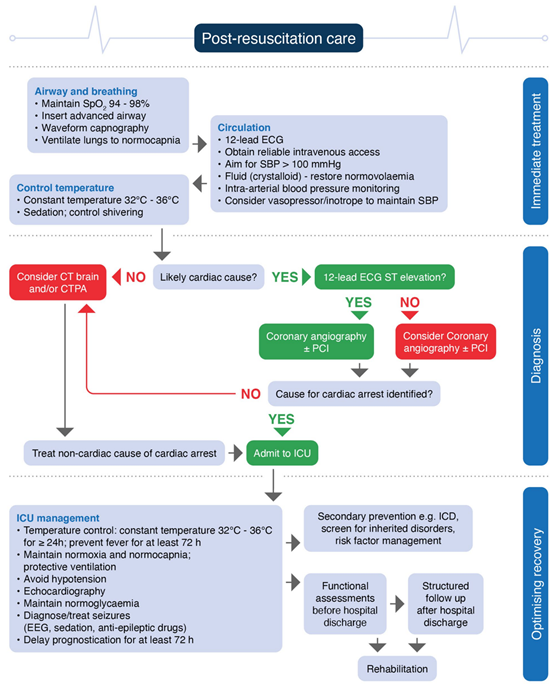
Treatment after cardiopulmonary resuscitation: 2021 ERC and ESICM guidelines. Treatment after cardiopulmonary resuscitation: 2021 guidelines of the European Resuscitation Council and the European Society of Intensive Care Medicine. Immediate treatment after cardiopulmonary resuscitation.
Summary
Based on the 2020 international scientific consensus on cardiopulmonary resuscitation and treatment recommendations, the European Resuscitation Committee (ERC) and the European Society of Intensive Care Medicine (ESICM) have jointly developed guidelines for the treatment of adults after cardiopulmonary resuscitation. The topics covered by this guide include post-cardiac arrest syndrome, diagnosis of the cause of cardiac arrest, patient oxygenation and ventilation control, coronary artery reperfusion, hemodynamic monitoring and management, epilepsy control, body temperature control, general severe illness A series of issues such as guardianship management and prognosis judgment.
1. Immediate treatment after cardiopulmonary resuscitation
Treatment after resuscitation should start immediately after continuous ROSC (recovery of spontaneous circulation), regardless of whether the patient is pre-hospital or in-hospital (below).
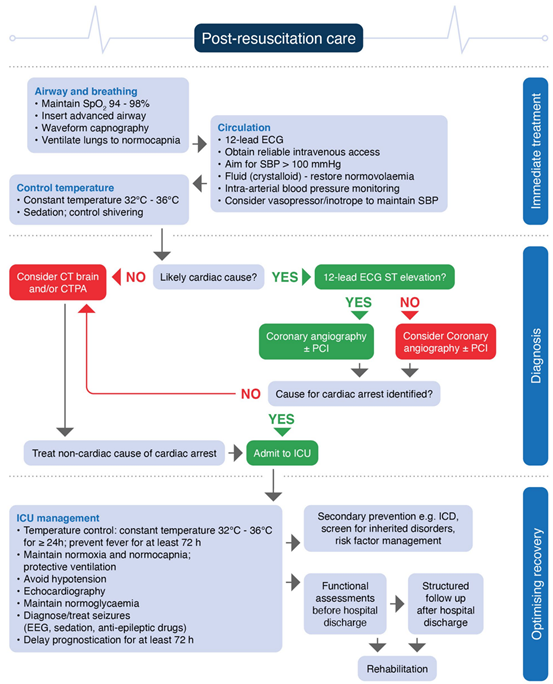
For out-of-hospital cardiac arrest, transfer to a cardiac arrest center should be considered.
2. Diagnosis of the cause of cardiac arrest
2.1 If there is clinical (for example, hemodynamic instability) or ECG evidence of myocardial ischemia, coronary angiography should be performed. If coronary angiography cannot determine the cause, CT brain and/or CT pulmonary angiography can be performed next.
2.2 When the patient is admitted to the hospital, before or after coronary angiography, CT examination of the brain and lungs shall be performed to identify the cause of the respiratory or nervous system.
2.3 If the patient has signs or symptoms that indicate neurological or respiratory causes (for example, the patient has previous headaches, epilepsy, neurological dysfunction; or has a clear record of respiratory disease with shortness of breath or hypoxemia), brain CT and/ Or CT pulmonary angiography.
3. Airway and breathing
3.1 Airway management after ROSC
3.1.1. After achieving the return of spontaneous circulation (ROSC), airway and ventilatory support should be continued.
3.1.2. The patient has a short-term cardiac arrest and the brain function returns to normal immediately. Tracheal intubation may not be required when breathing is normal. However, if the patient’s arterial blood oxygen saturation is lower than 94%, mask oxygen should be given.
3.1.3. If the patient has not yet been intubated during CPR, is still in a coma after ROSC, or has other clinical indications of sedation and mechanical ventilation, endotracheal intubation should be given.
3.1.4. Tracheal intubation should only be performed by experienced operators, who have a higher success rate.
3.1.5. The correct placement of the tracheal tube must be confirmed by capnography.
3.1.6. In the absence of experience in tracheal intubation, the reasonable method is to insert the supraglottic airway (SGA) or maintain the airway with basic techniques until a skilled tracheal intubation staff arrives.
3.2 Oxygenation control
3.2.1. After ROSC, 100% (or the maximum available) oxygen concentration should be used to give oxygen until the arterial blood oxygen saturation or arterial oxygen partial pressure can be reliably measured. (Weak recommendation, very low certainty evidence)
3.2.2. We recommend that under any circumstances, adult patients with ROSC after cardiac arrest should avoid hypoxemia (strong recommendation, very low certainty evidence).
3.2.3. After the patient’s ROSC, once the SpO2 can be reliably measured or the arterial blood gas value can be obtained, the inspired oxygen concentration should be titrated so that the patient’s oxygen saturation reaches 94–98% or the arterial arterial blood oxygen partial pressure (PaO2) reaches 10 –13 kPa or 75–100mmHg.
3.2.4. We recommend that in any case, adult patients with ROSC after cardiac arrest should avoid hyperoxemia (weak recommendation, low certainty evidence).
3.3 Ventilation control
3.3.1. For mechanically ventilated patients, arterial blood gases should be obtained and monitored with end-tidal CO2.
3.3.2. In patients who require mechanical ventilation after ROSC, ventilation should be adjusted so that the arterial partial pressure of carbon dioxide (PaCO2) reaches normal (ie 35-45mmHg).
3.3.3. We oppose routine targeted hypocapnia treatment in adult patients with ROSC after cardiac arrest (weak recommendation, low certainty evidence).
4. Loop
4.1 Coronary artery reperfusion
4.1.1. For adult ROSC patients, emergency coronary angiography evaluation should be performed for patients with cardiac arrest with suspected cardiac origin and ST elevation on the ECG (PCI should be performed immediately if necessary).
4.1.2. In patients with no ST elevation on ECG after out-of-hospital cardiac arrest (OHCA), if there is a high probability of acute coronary occlusion (for example, hemodynamic and/or electrophysiological instability), they should Consider urgent coronary angiography evaluation.
4.2 Hemodynamic monitoring and management
4.2.1. All patients should use arterial catheters for continuous blood pressure measurement, and reasonably monitor the cardiac output of patients with hemodynamic instability.
4.2.2. Early (as soon as possible) echocardiography is performed on all patients to detect any underlying cardiology and to quantify the degree of myocardial dysfunction.
4.2.3. Avoid hypotension (MAP<65mmHg). Target mean arterial pressure (MAP) to achieve sufficient urine output (>0.5mL/kg/h) and normal or decreased lactic acid.
4.2.4. We recommend that hemodynamic goals (such as MAP, systolic blood pressure) be considered during post-resuscitation treatment as part of post-resuscitation clustering interventions (low recommendation, low quality of evidence).
4.2.5. When the body temperature of TTM (targeted body temperature management) is 33°C, if blood pressure, lactic acid, SCVO2 or SvO2 are sufficient, bradycardia does not require treatment. If the above goals cannot be achieved, consider raising the target body temperature, but it should not be higher than 36°C.
4.2.6. According to the needs of individual patient’s vascular volume, vasoconstriction or positive muscle strength, use infusion, norepinephrine and/or dobutamine to maintain patient perfusion.
4.2.7. There is insufficient evidence to recommend specific hemodynamic goals. Hemodynamic goals should be considered according to the patient’s specific situation, and may be affected by the state and comorbidities after cardiac arrest (low recommendation, low quality of evidence).
4.2.8. Hormones should not be routinely used after cardiac arrest (weak recommendation, low-certainty evidence) until there is higher certainty evidence to support use.
4.2.9. Avoid hypokalemia, which is related to the occurrence of ventricular arrhythmia. We recommend administering potassium to maintain the patient’s serum potassium concentration between 4.0 and 4.5 mmol/L (best practice instructions).
5. Nerve function (optimize nerve recovery)
5.1 Control of seizures
5.1.1. We oppose the preventive treatment of epilepsy for adult survivors of cardiac arrest (the strength of recommendation is low, and the definitive evidence is very low).
5.1.2. We recommend antiepileptic treatment for adult survivors of cardiac arrest when they have seizures (low recommendation rate and very low definitive evidence).
5.1.3. We recommend using electroencephalogram (EEG) to diagnose whether patients with clinical convulsions have epileptiform seizures and to monitor the effect of treatment.
5.1.4. In order to treat seizures after cardiac arrest, we recommend the use of levetiracetam or sodium valproate as the first-line antiepileptic drugs in addition to sedatives.
5.2 Body temperature control
5.2.1. For patients undergoing target temperature management, we recommend selecting and maintaining a constant body temperature between 32 and 36°C as the target temperature (strong recommendation, moderate quality evidence). Whether certain subgroups of cardiac arrest patients may benefit from lower body temperatures (32–34°C) or higher temperatures (36°C) needs further research to clarify.
5.2.2. We recommend target temperature management for adult patients who initially had shockable heart rhythms with OHCA (out-of-hospital cardiac arrest), but did not respond after ROSC (strong recommendation, low quality of evidence).
5.2.3. We recommend that adult patients with OHCA who have an initial non-shockable rhythm and who still do not respond after ROSC should undergo target temperature management instead of not performing target temperature management (weak recommendation, very low-quality evidence).
5.2.4. We recommend that patients with IHCA (in-hospital cardiac arrest) who still do not respond after ROSC should undergo target temperature management instead of not performing target temperature management (weak recommendation, very low-quality evidence).
5.2.5. We recommend that if TTM is used, the duration should be at least 24 hours (weak recommendation, very low-quality evidence).
5.2.6. We oppose the routine and immediate rapid infusion of large amounts of cold saline for prehospital cooling of ROSC patients (strong recommendation, moderate quality evidence).
5.2.7. We recommend the prevention and treatment of fever in adult patients with persistent coma after the completion of TTM at 32 to 36°C (low recommendation strength, low quality of evidence).
6. General intensive care management
6.1 Use short-acting tranquilizers and opioids.
6.2 In patients receiving TTM, avoid the routine use of neuromuscular blockade drugs, but in the case of severe tremors during TTM, the use of this drug can be considered.
6.3 Routinely give preventive treatment of stress ulcer to patients with cardiac arrest.
6.4 Give preventive treatment of deep vein thrombosis.
6.5 The target blood glucose is 7.8-10mmol/L, if necessary, use insulin infusion; avoid hypoglycemia (<4.0mmol/L).
6.6 Start enteral feeding at a low rate during TTM (nourishment feeding), and increase the rate if there is a pointer after rewarming. If a TTM of 36°C is used as the target body temperature, the gastric feeding rate may increase earlier during TTM.
6.7 We do not recommend routine use of preventive antimicrobial therapy (weak recommendation, low certainty of evidence).
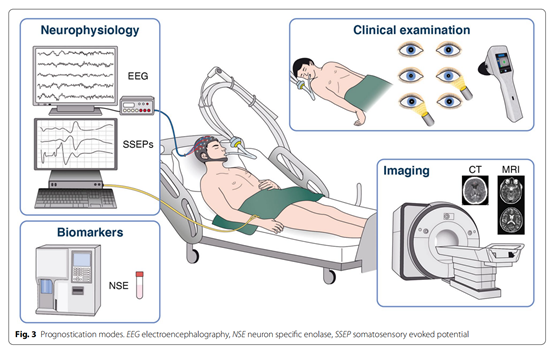
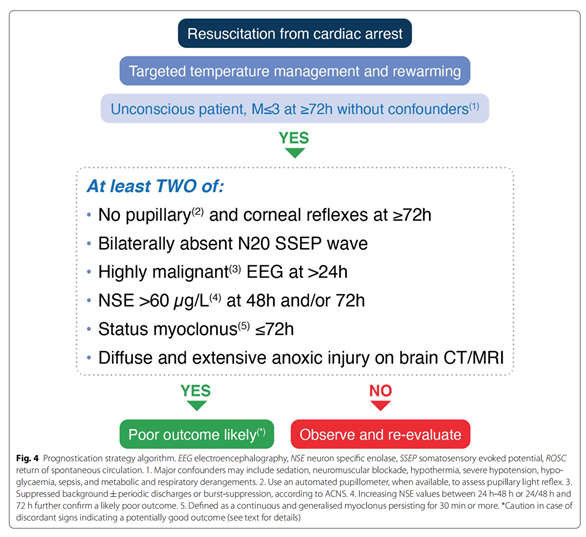
7. Prediction of neurological prognosis
7.1 Physical examination
7.1.1. We recommend using pupillary reflex at 72 hours or later after ROSC to predict the neurological outcome of adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence).
7.1.2. We recommend the use of quantitative pupillary measurements at 72 hours or later after ROSC to predict the neurological outcome of adult patients with coma after cardiac arrest (weak recommendation, low certainty evidence).
7.1.3. We recommend that the loss of bilateral corneal reflex be used 72 hours or later after ROSC to predict adverse neurological outcomes in adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence).
7.1.4. We recommend using myoclonus or myoclonus status within 96 hours after ROSC, in combination with other tests, to predict adverse neurological outcomes in adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence) ). We also recommend recording EEG during myoclonic seizures to characterize the phenotype of myoclonus.
7.2 Neurophysiology
7.2.1. We recommend the use of multimodal methods for neuroprognosis assessment, because no single test is specific enough to eliminate false positives (strong recommendation, very low evidence).
7.2.2. We recommend using the bilateral N20 wave loss of somatosensory evoked potentials (SSEP) combined with other indicators to predict the adverse outcome of adult patients with coma after cardiac arrest when ROSC ≥ 24 hours (weak recommendation, very low certainty evidence) ).
7.2.3. We recommend not to use the absence of background reactivity in EEG alone to predict adverse outcomes in adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence).
7.2.4. We recommend using EEG seizures in combination with other indicators to predict the adverse outcome of adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence).
7.2.5. We recommend using the sudden suppression of EEG when ROSC ≥ 24 hours in combination with other indicators to predict the adverse outcome of unsedated adult patients who are unsedated after cardiac arrest (weak recommendation, very low certainty evidence) .
7.3 Biomarkers
7.3.1. We recommend the use of neuron-specific enolase (NSE) within 72 hours after ROSC, in combination with other tests, to predict the neurological outcome of adults who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence) . There is no consensus on the threshold.
7.3.2. We oppose the use of S-100B protein to predict the neurological outcome of adult patients who are unconscious after cardiac arrest (weak recommendation, low certainty evidence).
7.3.3. We oppose the use of serum glial fibrillary acidic protein (GFAP), serum tau protein, or neuroflagella light chain (Nf) to predict adverse neurological outcomes in adult patients who are unconscious after cardiac arrest (weak recommendation, very low certainty evidence) ).
7.4 Imaging
7.4.1. We recommend using brain imaging studies to predict the neurological prognosis of patients only in centers with specific experience (weak recommendation, very low-quality evidence).
7.4.2. We recommend that within 72 hours after ROSC, the gray/white matter (GM/WM) ratio on cranial CT is significantly reduced, or there is extensive diffusion limitation in cranial MRI 2-7 days after ROSC, and combined Other predictive indicators to predict adverse neurological outcomes in patients who are comatose after cardiac arrest and those receiving TTM therapy (weak recommendation, very low-quality evidence).
-THE END-
(source:internet, reference only)
Disclaimer of medicaltrend.org



