The lung toxicity caused by immunotherapy may lead to fatal events!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
The lung toxicity caused by immunotherapy may lead to fatal events!
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
The lung toxicity caused by immunotherapy may lead to fatal events!
In recent years, immune checkpoint inhibitors (ICIs) have been widely used in cancer treatment, but the toxic side effects of immune-related pneumonia (CIP) are increasingly concerning, requiring further understanding of its clinical manifestations and treatment effects.
Introduction
This article reviews and analyzes the clinical manifestations, pulmonary imaging, and treatment regimens of 36 patients with locally advanced and metastatic NSCLC complicated by CIP.
ICIs are widely used in the treatment of melanoma and locally advanced and metastatic lung cancer without surgery, but their immune-related side effects pose certain risks to patients.
Among them, CIP, as the most common and fatal immune-related adverse event, has its unique clinical manifestations and imaging features, requiring early diagnosis and treatment.
Research Methods
The study included 704 patients with NSCLC diagnosed by postoperative histopathology, CT-guided lung biopsy, or bronchoscopic bronchial mucosal biopsy.
The patients’ clinical data included gender, age, smoking history, baseline health status, allergy history, tumor location, pathological type, differentiation degree, clinical stage, clinical symptoms, treatment methods, and prognosis.
The CT data of 704 cases were from the Picture Archiving and Communication System (PACS).
The CT manifestations of ILD were classified into various patterns according to the International Multidisciplinary IP Classification of the American Thoracic Society/European Respiratory Society.
The grading criteria of CIP were based on clinical data and imaging manifestations. The diagnosis of CIP was determined by the attending oncologist and confirmed by a multidisciplinary team.
Clinical Features of Patients
After screening 704 patients, only 36 were included in the study.
The average age of the included patients was 64.6 years, with a minimum age of 43 years and a maximum age of 82 years. Clinical important (CIP) occurred in 5.1% of patients.
The incidence rate was 80.6% in male patients and 19.4% in female patients.
Most patients (77.8%) had a history of smoking. Adenocarcinoma accounted for the largest proportion in the study (58.3%), followed by squamous cell carcinoma (33.3%).
44.4% of patients used ICIs as first-line treatment.
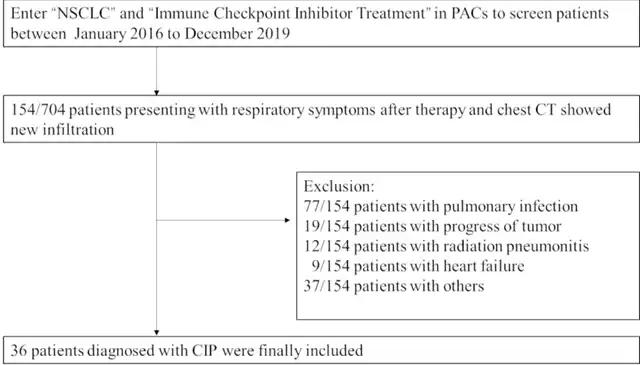
Figure 1 Diagram of screening CIP patients
Clinical Manifestations
The onset time of the 36 patients ranged from 0.1 to 17 months, with an average onset time of 3.5 months.
According to the NCCN grading criteria, there was 1 case of CIP G1 (2.8%), 11 cases of G2 (30.6%), 16 cases of G3 (44.4%), and 8 cases of G4 (22.2%). There were 24 cases (66.7%) of severe CIP G3-4.
The most common clinical symptoms were cough in 30 cases (83.3%), shortness of breath or difficulty breathing in 28 cases (77.8%), and fever in 10 cases (27.8%).
Four cases had rash (11.1%), three cases had hypothyroidism, and two cases had enteritis. One case had sudden cardiac arrest.
CT Imaging Features of CIP
The CT manifestations of the 36 CIP patients included ground-glass opacities, reticular shadows, consolidation shadows, nodular shadows, and bronchitis.
Among the CT manifestations, ground-glass opacities appeared in 32 cases, reticular shadows in 17 cases, consolidation shadows in 13 cases, nodular shadows in 8 cases, and bronchitis in 7 cases.
The CT manifestations of the 36 CIP patients were summarized as OP-like, NSIP-like, HP-like, DAD-like, and atypical imaging manifestations.
Among them, OP-like appeared in 14 cases, NSIP-like in 14 cases, HP-like in 2 cases, DAD-like in 1 case, and atypical imaging manifestations in 5 cases.
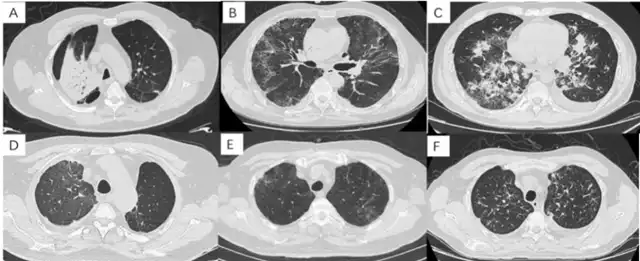
Figure 2 CT features of CIP: A: OP type: extensive consolidation in the right upper lobe; B: NSIP type: GGO and reticular shadows in both lungs; C: AIP type: multiple consolidations in both lungs, reticular shadows with GGO; D: HP type: GGO in the right upper lobe; E: HP pattern: GGO, nodular shadows in both upper lobes; F: Atypical changes: bronchial changes in both upper lobes
Treatment
After CIP occurred during ICI treatment, all patients discontinued or permanently discontinued ICI treatment.
Most patients received specific doses and courses of corticosteroid therapy, and some patients received intravenous immunoglobulin or tocilizumab therapy.
The average duration of drug use was 1.9 months, and the average initial dose of corticosteroids was 85.7 mg.
There were differences in the dose and duration of corticosteroid therapy among different CIP G2 patients, and there were differences in the dose and duration of corticosteroid therapy among different CIP G3 patients.
The corticosteroids used included prednisone, methylprednisolone, and dexamethasone.
Among the 36 patients with pneumonia, 7 died, with a mortality rate of 19.4%, while 29 patients improved.
Further results showed that there were no deaths in CIP G1-2 patients, while there were 7 deaths in CIP G3-4 patients.
Survival analysis showed that the survival rate of CIP G1-2 patients was significantly higher than that of CIP G3-4 patients.
In addition, the study also observed that the prognosis of HP-like and OP-like patients seemed to be better than that of NSIP-like and DAD-like patients.
For different imaging groups, the treatment effects were also different, with better treatment effects in G1-2 patients than in G3-4 patients, although the statistical difference was not clear due to the small number of cases.
Among the 4 patients who received ICI treatment again, 1 showed absorption, and no CIP recurrence occurred.
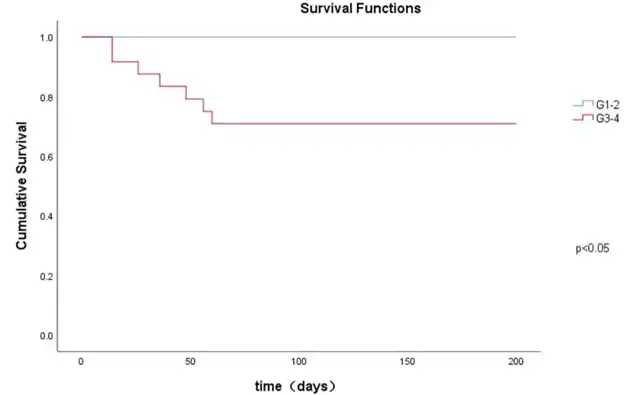
Figure 3 Kaplan-Meier analysis of survival of patients with CIP G1-2 and G3-4
Discussion
PD1 inhibitors and PD-L1 inhibitors are the most widely used drugs in ICI treatment. However, CIP is a common side effect of ICI treatment, with an incidence rate of about 3% to 5%. CIP G2-3 is more common, while the incidence of G4 is lower. The probability of pneumonia (CIP) with the use of PD-L1 inhibitors is lower than that with PD-1 inhibitors. When PD-1 or PD-L1 is used in combination with CTLA-4, the incidence of CIP increases significantly. Most of these data come from previous clinical trials of various cancers, but there is a lack of actual research analysis for locally advanced and metastatic NSCLC.
According to the research data, most patients belong to CIP G2-3. Common symptoms include cough, shortness of breath or difficulty breathing, fever, and productive cough, as well as respiratory system-related symptoms. Inflammatory markers in CIP patients, such as C-reactive protein, erythrocyte sedimentation rate, high white blood cell count, and neutrophil count, also increase. Bronchoscopy can assist in the diagnosis of CIP, and the lymphocyte count and neutrophil ratio in BALF are important for the diagnosis and prognosis. Therefore, bronchoscopy is necessary to differentiate between pulmonary infection and CIP.
The imaging manifestations of CIP lung injury are atypical and diverse. The basic imaging manifestations of CIP include GGO, consolidation, reticular shadowing, interstitial thickening, traction bronchiectasis, nodular shadowing, and reticular shadowing. The imaging findings combined with pathology are most commonly OP-like, followed by NSIP-like, DAD-like,
HP-like, etc. In most patients, CIP involves both lungs, and in a few cases, only one side of the lung is affected. Different imaging manifestations often indicate different degrees of disease severity, sensitivity to corticosteroid therapy, and prognosis. Patients with HP-like and OP-like patterns often have a good prognosis after corticosteroid therapy, while those with DAD-like patterns progress rapidly and are less sensitive to corticosteroid therapy. In this study, patients with HP-like patterns had a good prognosis, while those with OP-like patterns had worsening conditions. Three NSIP-like pattern patients died, and one DAD-like pattern patient died within one month of corticosteroid therapy.
For the treatment of patients with combined immune-related CIP, discontinuation of the relevant ICI drugs may alleviate symptoms in some G1 patients, but for G2 and above patients, discontinuation alone cannot improve the condition. The symptoms of most patients can be relieved by corticosteroid therapy, but the dose and duration of corticosteroid therapy are not clear. Domestic experts recommend corticosteroid therapy, with a specific dose of 1 mg/kg/day to 2 mg/kg/day prednisone. Severe patients need to permanently discontinue ICIs and recommend higher doses of prednisone for more than 8 weeks. For patients who are not sensitive to corticosteroid therapy, early combination with immunosuppressive agents may help reduce the mortality rate.
In this study, 4 patients received ICI retreatment, including 1 CIP G1 patient, 2 CIP G2 patients, and 1 CIP G3 patient, but no obvious CIP symptoms were observed. Among the 452 patients with available data who were analyzed, 28.8% of patients experienced the same irAE again. Among the 101 CIP patients who received ICI treatment again, 34% of patients experienced CIP recurrence. For patients who are rechallenged with immunotherapy, caution should be exercised. There are currently no clear guidelines for rechallenging, but it is suggested that the target population for rechallenge should be patients with stable conditions, low severity of initial CIP onset, and good response to corticosteroid therapy. After using ICIs, strict monitoring of irAE-related symptoms is necessary. If CIP recurs, the drug should be stopped promptly and corticosteroids should be used, and if necessary, immunosuppressive agents can be used in combination.
CIP is one of the common side effects of immune checkpoint inhibitor therapy. Studies have found that the grading of CIP is significantly related to the prognosis of patients, with a good prognosis in CIP G1-2 patients and a relatively high mortality rate in CIP G3-4 patients. Therefore, early detection and treatment of CIP are particularly important for reducing mortality. Regular follow-up chest CT scans can effectively detect CIP early. However, there is currently no effective, non-invasive detection method for asymptomatic CIP patients. Studies have shown that the levels of IL-6 and PLR in CIP patients are elevated, and close monitoring of these blood indicators can help to detect CIP patients early.
Conclusion
With the widespread use of ICIs in the treatment of NSCLC and other cancers, related (CIP) has become a challenging problem for clinical physicians, directly affecting whether patients can continue treatment. Further research on the clinical characteristics, treatment regimens, and prognosis of CIP will help improve the prognosis of patients and win more treatment time for cancer patients.
The lung toxicity caused by immunotherapy may lead to fatal events!
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9983156/
(source:internetHHR7nf1XD5yy7EF7Njc5tw, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



