COVID-19 patients: 1/3 worsened and 1/2 symptoms presisted after discharge
COVID-19 patients: 1/3 worsened and 1/2 symptoms presisted after discharge
COVID-19 patients: 1/3 worsened and 1/2 symptoms presisted after discharge. One-third of patients with COVID-19 reported that their condition worsened after discharge, and more than half had persistent symptoms.
On March 22, Nature’s sub-Journal Nature Medicine published an online review titled Post-acute COVID-19 syndrome, which comprehensively counted the sequelae of various new coronavirus pneumonia.

More than half of patients still have symptoms after recovery
The researchers included a number of papers on the sequelae of new coronaviruspneumonia, including clinical studies in France, Italy, the United Kingdom, Spain, the United States, and China. The number of participants in each study ranged from 100 to 1733.
The new coronavirus infection can be divided into two periods: the “acute infection period” and the “chronic recovery period.” During the acute infection period, patients may have symptoms such as fever, cough, and pneumonia, or they may not show any obvious symptoms. During the chronic recovery period, because the virus infection can cause damage to human tissues and organs, some uncomfortable symptoms will occur, which is the “COVID-19 sequelae” that this review focuses on.
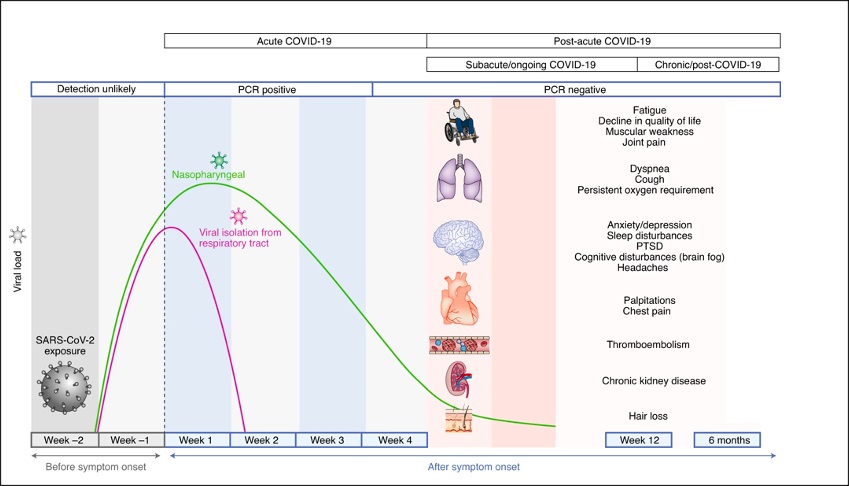
Possible post-infection possible observational symptomatology
(Source: Nature Medicine)
The possible pathophysiological mechanism of new coronavirus sequelae:
- Virus-specific pathophysiological changes, that is, viral infections can cause damage to human tissues and organs;
- The immune response and inflammatory response produced by acute viral infection refer to the possible excessive immune response in the body when the virus is cleared;
- Some critically ill patients can expect incidental sequelae.
A survey of 38 hospitals in Michigan, the United States studied the prognosis of 1,250 recovered patients with new coronavirus pneumonia 60 days after discharge. During the study period, 6.7% of the patients died and 15.1% of the patients required re-admission to the hospital.
In addition, of the 488 patients who completed the survey, 32.6% reported persistent symptoms, of which 18.9% developed new or worsening symptoms.
Among these symptoms, difficulty breathing when going upstairs (22.9%) was the most common. Other symptoms included coughing (15.4%) and continued loss of taste and/or smell (13.1%).

Similar findings also appeared in the European survey of COVID-19 patients.
According to related surveys in Italy, during the 60-day follow-up period after discharge, 87.4% of 143 discharged patients with new coronavirus pneumonia had persistent symptoms, including fatigue (53.1%), dyspnea (43.4%), and joint pain (27.3%) ) And chest pain (21.7%) are the most common symptoms. Among them, 55% of patients have three or more of the above symptoms at the same time, and 44.1% of patients believe that their quality of life has decreased.
A study of 150 French patients also showed that during the 60-day follow-up, two-thirds of patients had persistent symptoms, and one-third of them believed that their current state was worse than when they were sick.
In a study from Wuhan, China, researchers investigated the condition of 1733 patients with new coronavirus disease 6 months after the onset of the disease. The results also showed that patients with new coronavirus disease still had persistent symptoms after being discharged from the hospital. Fatigue and muscle weakness were the most common (63 %), followed by difficulty sleeping (26%), and about 23% have anxiety/depression.
Inventory of the sequelae of COVID-19 in each system
01. Lung sequelae
Similar to other patients with acute respiratory distress syndrome, dyspnea is the most common persistent symptom (42 to 66%) of patients with new coronavirus pneumonia;
A follow-up study from China also found that decreased exercise capacity is also a very common symptom. The 6-minute walk distance of 25% of patients is lower than the normal reference value, which is very similar to SARS and MERS patients; there are also some patients (6.6~ 6.9%) reported symptoms of persistent hypoxia.
It is worth mentioning that in the follow-up of 349 patients recovering from COVID-19, researchers found that half of the patients had abnormalities in the lungs, such as bilateral ground-glass opacity in the lungs and organ damage such as lung fibrosis.
02. Sequelae of Thrombosis
At present, I tend to believe that COVID-19 may bring vascular diseases, and there are data indicating that venous thromboembolism (VTE, the incidence rate is less than 5%) may occur after the recovery of COVID-19.
03. Cardiovascular sequelae
According to reports, in the 60-day follow-up survey of COVID-19 patients, up to 20% of patients reported chest pain symptoms. In the Chinese study, 9% and 5% of patients reported persistent heart palpitations and chest pain during the 6-month follow-up period. In addition, researchers found that the incidence of stress cardiomyopathy increased during the epidemic compared to before the COVID-19 pandemic.
04. Nervous system sequelae
Similar to the sequelae of SARS patients, patients with new coronavirus disease reported a series of neurological symptoms after being discharged from the hospital, including post-traumatic stress disorder, anxiety, depression, inattention and abnormal sleep, headaches and so on. Other neurological symptoms include migraine, delayed headache, loss of taste and smell, and even memory loss.
05. Kidney sequelae
About 5% of COVID-19 patients and 20-31% of COVID-19 patients (especially severely infected patients requiring mechanical ventilation) have severe acute kidney injury (AKI) and require renal replacement therapy (RRT).
06. Endocrine sequelae
In the weeks to months after COVID-19 patients recover, symptoms of diabetic ketoacidosis (DKA) have been observed in patients who are known to have no diabetes. Similarly, subacute thyroiditis and thyrotoxicosis have also been reported in patients with COVID-19.
07. Gastrointestinal and hepatobiliary sequelae
Severe gastrointestinal and hepatobiliary sequelae have not been found in COVID-19 patients, but the COVID-19 virus may have an impact on the gut microbiota.
08. Skin sequelae
In a study of 716 patients with COVID-19, most skin diseases appeared after other symptoms. The most common symptom was alopecia (about 20% of patients reported alopecia symptoms), which may be caused by a stress response due to viral infection. 3% of patients developed a rash during the 6-month follow-up.
COVID-19 patients discharge ≠ complete recovery
Researchers suggest: For many COVID-19 patients, being discharged from the hospital just means that they have passed the “acute infection period”, not that they have fully recovered, and there is a long chronic recovery period.

Specifically, for the recovery of the patient’s lungs, the patient’s blood oxygen saturation can be measured at home as appropriate, and high-resolution computed tomography and computed tomography of the chest can be performed 6 months and 12 months after discharge. Pulmonary angiography. As a drug to suppress excessive immunity, glucocorticoid therapy can reduce the risk of death in some patients.
For possible blood system sequelae after contracting COVID-19, including problems such as coagulation disorders, the researchers suggest that in some high-risk patients, oral anticoagulants and low molecular weight heparin can be considered to prevent thrombosis. At the same time, the researcher also recommends that all patients get out of bed and exercise when appropriate.
Finally, for some endocrine sequelae, the researchers said that in the case of no risk of developing type 2 diabetes, patients with diabetes symptoms should be tested by laboratory to rule out other possible causes of related symptoms, such as hyperthyroidism. , And promptly refer to relevant departments.
(source:internet, reference only)
Disclaimer of medicaltrend.org



