Advanced NSCLC: Abnormal thyroid function caused by immunotherapy
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Advanced NSCLC: Abnormal thyroid function caused by immunotherapy
Advanced NSCLC: Abnormal thyroid function caused by immunotherapy. Abnormal thyroid function caused by immunotherapy indicates better survival benefit for advanced NSCLC.
While immunotherapy has achieved significant efficacy, immune-related adverse events (irAEs) caused by immunotherapy are also the focus of clinical attention, because irAEs are completely different from those caused by conventional radiotherapy and chemotherapy, such as skin toxicity, enteritis, pneumonia, Endocrine dysfunction, etc.
Immune checkpoint inhibitors represented by anti-PD-1/PD-L1 have become a research hotspot in the field of tumor treatment in recent years, changing the pattern of tumor treatment. In the field of non-small cell lung cancer, immunotherapy can significantly improve the PFS and OS of patients compared with standard platinum-containing dual-drug chemotherapy, and has entered the first-line treatment of non-small cell lung cancer.
While immunotherapy has achieved significant efficacy, immune-related adverse events (irAEs) caused by immunotherapy are also the focus of clinical attention, because irAEs are completely different from those caused by conventional radiotherapy and chemotherapy, such as skin toxicity, enteritis, pneumonia, Endocrine dysfunction, etc. Previous studies have found that patients with immune-related skin toxicity have better tumor response.
The incidence of endocrine toxicity related to PD-1 inhibitors is approximately 12.0%-30%, and the most common endocrine irAEs are thyroid dysfunction (TFA-irAEs). However, whether the occurrence of thyroid dysfunction (TFA) has a predictive value is still controversial. Recently, a retrospective study published in International Immunopharmacology analyzed the relationship between TFA induced by PD-1 inhibitors and the survival of advanced NSCLC.
1 The incidence of TFA-irAEs is 20.9%, most of which are grade 1-2
The study retrospectively analyzed 191 patients with advanced NSCLC treated with PD-1 inhibitors, of which 136 patients had PD-L1 expression detection, and 52 patients (27.2%) had high expression (≥50%). Most patients (40.3%, n = 77) received PD-1 inhibitors as second-line treatment. Nearly half of the patients received immunization combined with chemotherapy, and about 40.3% of patients received radiotherapy before starting immunization.
Among all patients, 106 received K drug treatment and 85 received O drug treatment. Among all patients, 40 cases (20.9%) developed TFA-irAE. It is worth noting that in patients with TFA-irAEs, the positive expression of thyroid peroxidase antibody (TPOAb)/thyroglobulin antibody (TgAb) is significantly higher.
The occurrence time of TFA-irAEs is 3 to 28 weeks after receiving PD-1 inhibitor treatment. The median onset time of subclinical hypothyroidism was 13 weeks, the median onset time of obvious hypothyroidism was 9 weeks, the median onset time of subclinical hyperthyroidism was 7 weeks, the median time of obvious hyperthyroidism The occurrence time is 6 weeks.
Among all patients with TFA-irAEs, 62.5% (n=25) patients had hypothyroidism, and 37.5% (n=15) patients had hyperthyroidism. Thirty-one patients were tested for TPOAb, and 10 were positive (>34 IU/mL). In addition, 31 patients were also tested for TgAb, and 8 were positive (>115 IU/mL). According to CTCAE. v5.0, 60% (24/40) of TFA-irAEs were grade 1, 37.5% (15/40) were grade 2, only 1 case (2.5%) was grade 3, and no patients had grade 4 TFA-irAEs.
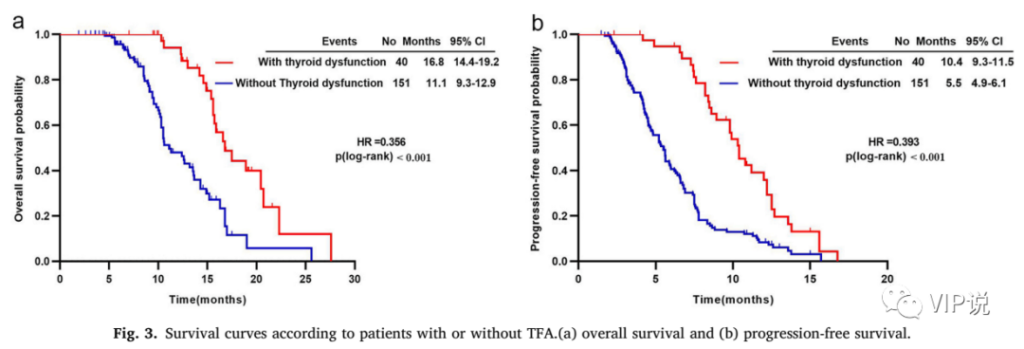
2 Patients with TFA-irAEs have significantly longer OS and PFS
The median OS of patients with and without TFA-irAEs was 16.8 months and 11.1 months, respectively (HR = 0.356; p <0.001), as shown in Fig.3a. In terms of PFS, patients with TFA-irAEs had significantly longer PFS than those without (10.4 months vs 5.5 months, HR = 0.393, p <0.001), as shown in Fig.3b. At the same time, in patients with TFA-irAEs, there was no significant difference in PFS and OS in patients receiving immune combination therapy and immune monotherapy.
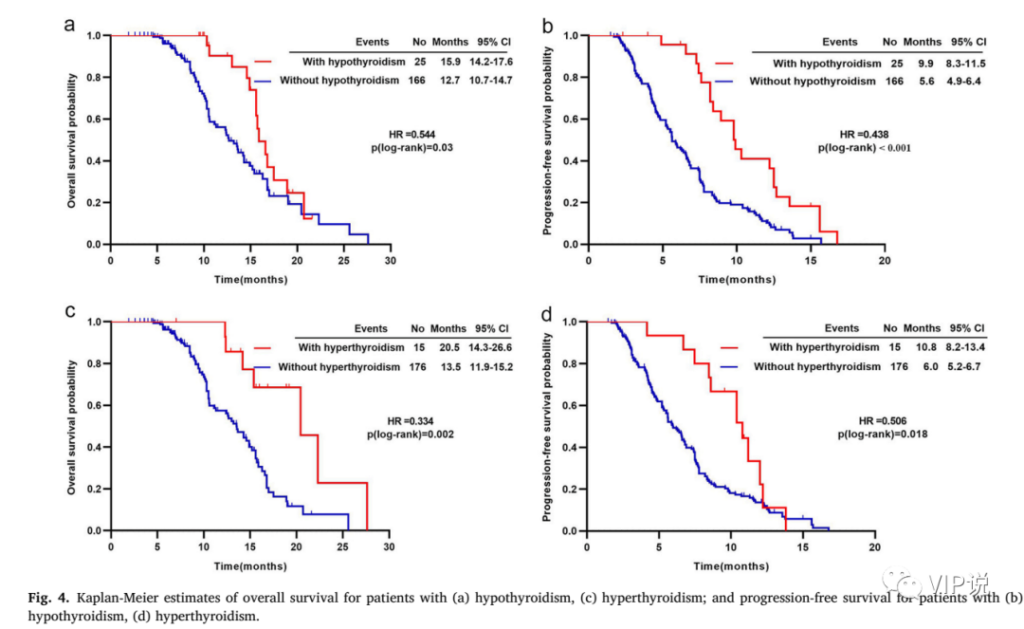
3 Subgroup analysis showed that the hypothyroidism group and the hyperthyroidism group had significantly longer OS and PFS than the non-hypothyroidism and non-hyperthyroidism groups
Subgroup analysis showed that the hypothyroidism group had a significantly longer OS than the non-hypothyroidism group (15.9 months vs 12.7 months, HR=0.544, p=0.03), as shown in Fig. 4a. Compared with the non-hyperthyroidism group, the hyperthyroidism group also had a significantly longer OS (20.5 months vs 13.5 months, HR=0.334, p=0.002), as shown in Fig. 4c. In terms of PFS, similar trends were also observed, as shown in Fig. 4b and Fig. 4d.
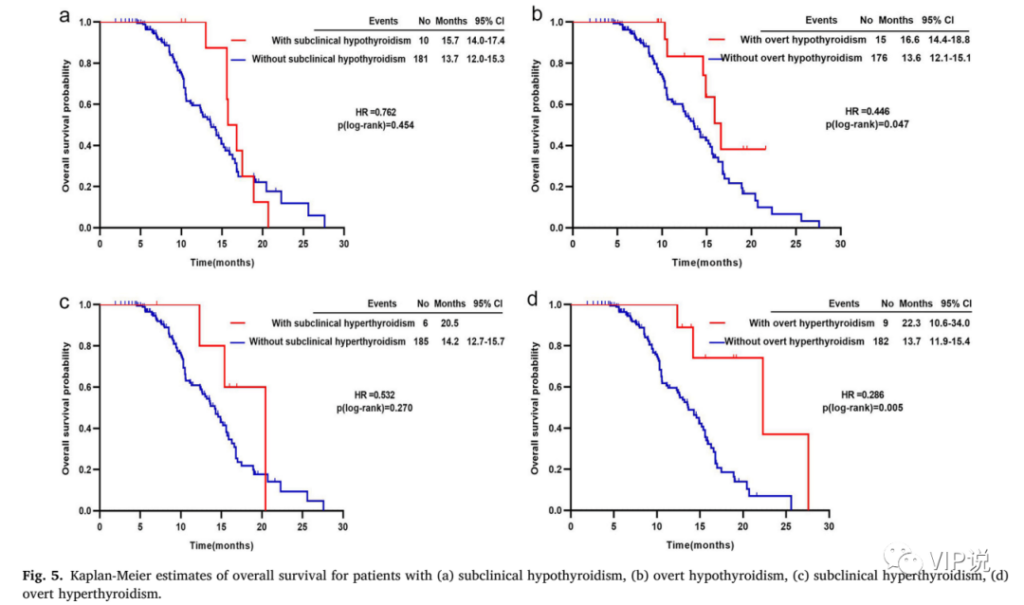
4 Subgroup analysis showed that TFA patients with obvious symptoms had significantly longer OS and PFS than those without TFA
Further analysis of the prognosis of the clinically unobvious (subclinical) group and the obvious TFA group showed that patients with obvious hypothyroidism had a longer OS than patients with unobvious symptoms (16.6 months vs 13.6 months, HR = 0.446, p = 0.047), as shown in Fig. 5b. On the other hand, patients with hyperthyroidism with obvious symptoms also have a longer OS (22.3 months vs 13.7 months, HR = 0.286, p = 0.005), as shown in Fig. 5d. For patients with TFA-irAEs with insignificant clinical symptoms, there is no significant difference in OS compared with those without TFA-irAEs, as shown in Fig. 5a and Fig. 5c.
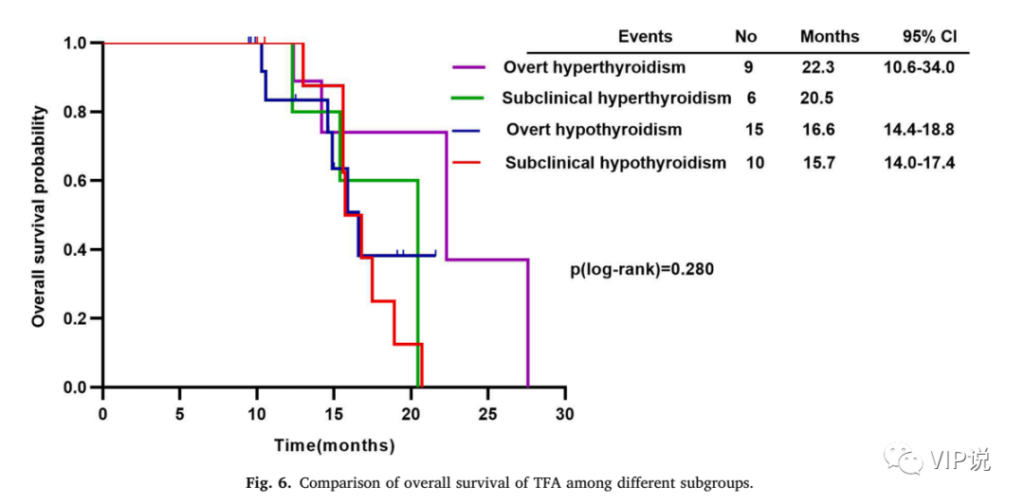
5 Patients with obvious symptoms of hyperthyroidism have the longest OS
Patients with obvious hyperthyroidism have the longest OS. Compared with hyperthyroidism with unobvious symptoms, hypothyroidism with obvious symptoms, and hypothyroidism with unobvious clinical symptoms, as shown in Fig. 6.
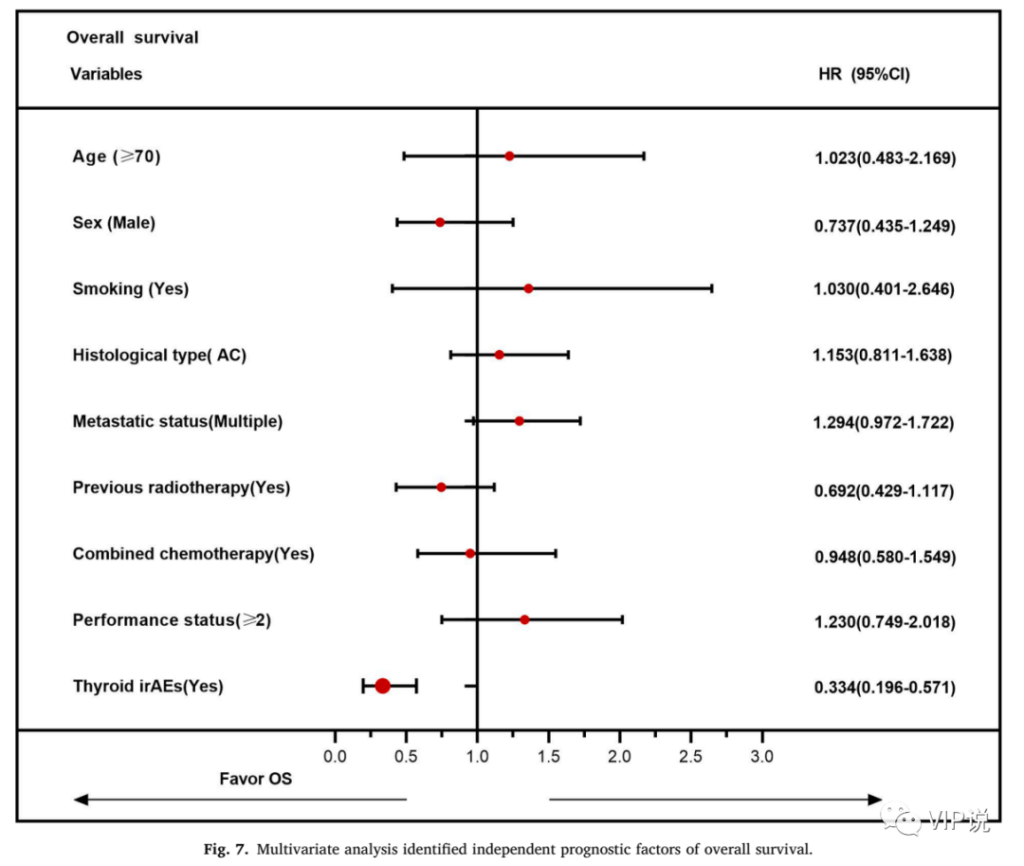
6 Multivariate analysis shows that the occurrence of TFA-irAEs is independently associated with better OS
Multivariate analysis showed that patients with TFA-irAEs were independently associated with better OS (HR = 0.334, 95%CI 0.196–0.571), as shown in Fig. 7.
7 Conclusion
TFA caused by PD-1 inhibitors that appeared in the early stage is relatively mild in clinical practice, and serious AEs rarely occur and can be well controlled. TFA-irAEs are positively correlated with the efficacy of PD-1 inhibitors, and may be used as a predictive biomarker for immunotherapy response.
(source:internet, reference only)
Disclaimer of medicaltrend.org



