How about the superimposed effects when shingles virus + HIV?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
How about the superimposed effects when shingles virus + HIV?
How about the superimposed effects when shingles virus + HIV? When shingles virus encounters HIV, what kind of superimposed effect will occur?
AIDS, the pathogen is human immunodeficiency virus (HIV). After the virus infects the human body, it mainly invades the immune system, including CD4+ T lymphocytes, mononuclear macrophages and dendritic cells, etc., mainly manifested by the continuous number of CD4+ T lymphocytes Decrease, and ultimately lead to defects in human cellular immune function, causing a variety of opportunistic infections and tumors.
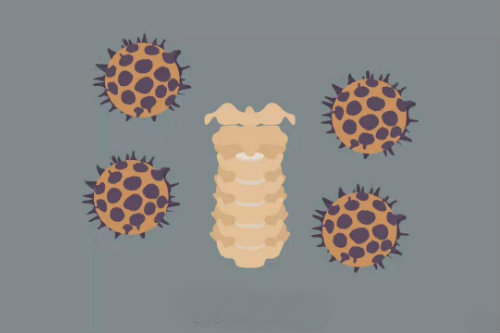
Herpes zoster (HZ) is an infectious disease caused by the varicella-zoster virus. After the first infection, the virus lurks in the dorsal root ganglia. When the age grows or the immunity declines, the virus reproduces and replicates. The virus has neurotrophic and skin characteristics, mainly manifested as skin erythema and blisters accompanied by different degrees of neuralgia.
There are data showing that the probability of HZ in HIV-positive people will increase by 7 times. Therefore, when the herpes zoster virus encounters HIV, which is compatible with human immunity, what kind of superimposed effect will occur?
generally
In the ratio of males to females, the incidence of males is often more than that of females, and the age of onset is about 40 years old. The age of onset of males is more than that of females. This shows that HIV combined with HZ infection is closely related to sexually active young and middle-aged men; in addition, the incidence is more frequent in spring and summer than in autumn and winter The season is different from the season when shingles occurs.
Clinical manifestations
Most patients have extensive skin lesions, often manifested as severe inflammation and exudation. The number of blisters can reach hundreds of thousands, which can easily cause bullae, blood blisters and combined skin infections, local ulcers, and obvious pain and itching in the affected area. (As shown below).
Onset characteristics
The first attack accounted for about 83%, and the relapsed patients accounted for about 17%. The recurrence of HZ was related to the decrease in the level of specific T cell immunity in the body after HIV infection. The proportion of people with fever is 65%, mainly with moderate to low fever. 57% of the patients were admitted to hospital with herpes zoster as the main symptom, and 43% were rashes that occurred during hospitalization with AIDS. About 25% had blood blister, about 33.3% had bullae, and about 26.1% had bacterial infection.
Nerve segment distribution
The damage to a single nerve segment is 87.8%, of which the intercostal nerve area and the lumbosacral nerve area are the main ones, and the rest are basically involving 2 nerve areas, and the cellular immune damage is more obvious.
Neuralgia
|
Without pain |
— |
6% |
|
Mild pain |
Pain is tolerable, daily life is not significantly affected, sleep is not disturbed |
35% |
|
Moderate pain |
Pain is obvious, need to take painkillers, sleep is disturbed to some extent |
39% |
|
Severe pain |
The pain is severe and unbearable, analgesics must be used, and sleep is severely affected |
20% |
Laboratory examination
According to the HIV/AIDS clinical classification standards of the US Centers for Disease Control and Prevention, according to the number of CD4+ and clinical manifestations, the disease stages of patients are mainly B2 (11.6%), B3 (21.7%), and C3 (63.1%), which indicates that the more severe the AIDS condition , The higher the incidence of shingles.
From the count trend, the lower the CD4+ count, the higher the incidence of herpes zoster. It is inferred that the inhibition of CD4+ T cell function may be the main reason for the resurrection and replication of the herpes virus that has been latent in the nerves for a long time. However, HIV load and CD8+ cell count have no significant effect on the incidence of shingles.
Skin histopathological examination
Eosinophilic inclusions can be seen in the nucleus of the blister epithelium, and vasodilatation, edema, and infiltration of perivascular lymphocytes and polynuclear leukocytes can be seen in the upper dermis.
Prognostic outcome
A very small number of MODS died due to multiple infections, and most of them can recover, but the skin lesions disappear for a relatively long time, and it is easy to leave scars and develop postherpetic neuralgia (PHN).
The incidence of PHN is about 15%, and the general course of treatment is 7-14 days. Analgesia and nerve nutrition are similar to those of common herpes zoster infections, and those with large erosion ulcers or co-infected patients need to apply antibiotics systematically. Considering AIDS, glucocorticoids are not recommended to avoid more serious opportunistic infections.
Special Note
With herpes zoster as the first symptom, extensive skin lesions, combined with blood blister bullae, or obviously incompatible with age, it is necessary to check for HIV.
For young and middle-aged patients with recurrent shingles, such as non-tumor or long-term immunosuppressive patients, HIV screening is necessary.
The reactivated VZV infection may occur at any stage of HIV infection, and special attention should be paid to whether there is HIV infection in genital herpes.
Herpes zoster is not only used as a clinical indicator of HIV infection, the appearance of herpes zoster in HIV-infected persons is also a precursor to the onset of AIDS.
If the patient has a history of intravenous drug use, the effect of general analgesics is poor, and there may be acyclovir resistance.
Treatment measures
-
Local skin shingles: famciclovir 500 mg, oral, bid or valacyclovir 1 g, oral, tid, course of treatment for 7-10 days.
-
Severe skin and mucosal lesions: Acyclovir 10 mg/kg, 8 hours/time, intravenous drip, valacyclovir 1 g, tid after the condition is stable, until all the lesions disappear.
The data in the article are only based on the analysis and summary of the literature case review data, not a large-scale epidemiological investigation, and are for reference only.
(source:internet, reference only)
Disclaimer of medicaltrend.org



