How does the virus vaccine work?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
How does the virus vaccine work?
How does the virus vaccine work? Vaccines work by inducing or training the host’s immune system. Vaccines enable the immune system to recognize similar viruses and produce corresponding immune responses for years or even longer after the first exposure to the virus.
This function of the immune system is also called immune memory. A qualified virus vaccine can build immunity and memory, and prevent the occurrence of typical pathogenic consequences after natural infection. The success of immunization in stimulating long-term immune memory is one of the greatest scientific and medical achievements of mankind.
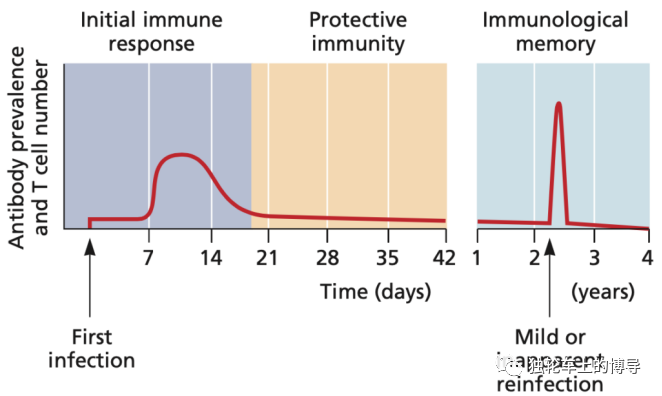
1. The response of immune memory cells to infection and subsequent reinfection. (Note: First infection, first infection. Mild or inapparent reinfection, mild or inapparent reinfection. Antibody prevalence and T cell number, antibody titer and T cell number.)
Immune memory is maintained by specialized T and B lymphocytes, these lymphocytes still exist after the infection is resolved, and most activated immune cells will gradually die. These memory cells can respond quickly to subsequent infections (see picture above). Ideally, an effective and durable vaccine is one that can induce and maintain a large number of memory cells. If the host is infected with the same virus again, memory B cells and T cells will quickly control the virus before the disease occurs. This model is applicable to most human viruses that have corresponding vaccines, including measles, mumps, varicella-zoster virus, and polio virus. In some cases, the virus is prone to antigenic mutation, such as influenza virus. The mutated virus can eliminate the complete protection of the memory immune response and requires re-vaccination with a newer vaccine.
Protection against infection or disease
The memory response caused by most human virus vaccines does not prevent re-infection, but only prevents the development of the disease. A person may be repeatedly exposed to the virus without realizing it, because the memory response eliminates the virus before the symptoms appear. For example, after being vaccinated with an inactivated polio vaccine, the virus can still replicate in the intestine, but it can effectively prevent the development of polio. On the other hand, the human papillomavirus (HPV) vaccine is more than 90% effective in blocking infection (Reference 1). Therefore, it is believed that the HPV vaccine can induce sterilizing immunity.
Whether the COVID-19 (New coronavirus Pneumonia) vaccine can stop the infection is unclear, as vaccinated people have not yet been tested systematically on a large scale. The results of some small-scale studies have shown that some vaccines can prevent infection. However, these studies are not conclusive, because they were only conducted shortly after vaccination, when the serum antibody level was much higher than the level after 6 months. Only after at least 6 months can we accurately measure the extent to which vaccination can prevent SARS-CoV-2 (new coronavirus) infection. It is possible that no COVID-19 vaccine can completely prevent the infection, but it can sufficiently reduce the propagation of the virus to prevent the spread of the virus in the population.
Herd immunity
An effective vaccine must be able to induce protective immunity in a large part of the population. Not everyone in the population needs to be vaccinated to stop the spread of the virus, but enough people must be vaccinated to stop the spread of the virus. When the possibility of infection drops below a critical value, human-to-human transmission ceases. This effect is called herd immunity.
The formula for calculating the herd immunity threshold is 1-1/R0. R0 is the average number of non-immune individuals that will be infected when encountering active infected individuals. As the number of copies R0 increases, the value of 1/R0 decreases, and 1-1/R0 is closer to 1, or 100%. For variola virus, the herd immunity threshold is 80-85%, and for measles virus with higher R0, the herd immunity threshold is 93-95%. In the early stage of the COVID-19 outbreak, the R0 of SARS-CoV-2 was calculated as 2-3, which would require reaching a herd immunity threshold of 50-70%.
Herd immunity only works when the vaccine prevents infection or sufficiently reduces the propagation of the virus in the host to prevent human-to-human transmission. As mentioned above, there is no reason to believe that the COVID-19 vaccine cannot sufficiently reduce transmission and thus achieve herd immunity.
No vaccine is 100% effective in inducing human immunity. Therefore, the level of immunity does not equal the number of people vaccinated. For example, when 80% of the population is vaccinated against measles, only about 76% of the population is actually immune, far below the 93-95% required for herd immunity.
What role do T cells play?
For many viral infections, antibodies are the key to preventing infection. However, the complete elimination of infection often requires the action of cytotoxic T cells, which can kill virus-infected cells. For vaccines that cannot produce sterile immunity, T cells are likely to play a role in destroying virus-infected cells and preventing disease development.
When discussing the COVID-19 vaccine, this division of labor between B cells and T cells has been largely ignored. Most research involves the induction of antibodies and their ability to neutralize viral infections. The COVID-19 vaccine does induce virus-specific T cells, which are likely to clear the infection from the vaccinated individual.
It is reported that the amino acid changes of SARS-CoV-2 variants will not affect T cell epitopes, and the T cell response of people who have recovered from infection or been vaccinated will not be affected by these changes .
Therefore, it seems that even if the worried mutations can escape the previous antibody immunity to some extent, they will be cleared by the T cell response, avoiding serious illness and death. The results of the Phase III trial of Johnson & Johnson’s COVID-19 vaccine support this hypothesis.
(source:internet, reference only)
Disclaimer of medicaltrend.org



