Common special staining and histochemical techniques
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Common special staining and histochemical techniques
Common special staining and histochemical techniques. Special staining refers to the staining technique of tissue sections as opposed to ordinary (conventional) staining, namely hematoxylin and eosin (HE) staining.
Basic theory
Knowledge point 1: The meaning of special dyeing
Special staining refers to the staining technique of tissue sections as opposed to ordinary (conventional) staining, namely hematoxylin and eosin (HE) staining. It mainly uses the differences in the physical properties of tissues and cells to dye dyes, uptake and loss rate, to stain tissues, so as to show certain specific components in normal and pathological tissues and cells, such as connective tissue, muscle tissue, and nerve tissue. , Lipids, carbohydrates, proteins and nucleic acids, pigments, amyloids, inorganics, neuroendocrine cell cytoplasmic granules and other organelles, pathogenic microorganisms, blood and lymph tissues, bone and cartilage tissues, etc.
Knowledge point 2: The meaning of histochemical technology
Histochemistry technology mainly refers to the technology of displaying some special chemical components in tissues and cells on tissue sections, using colorless reagents to chemically react with a certain component in tissues and cells to generate colored precipitated products in situ.
Application of indications and analysis and judgment
Knowledge point 1: Application of three-color dyeing
At present, the most commonly used method is Masson’s three-color dyeing method.
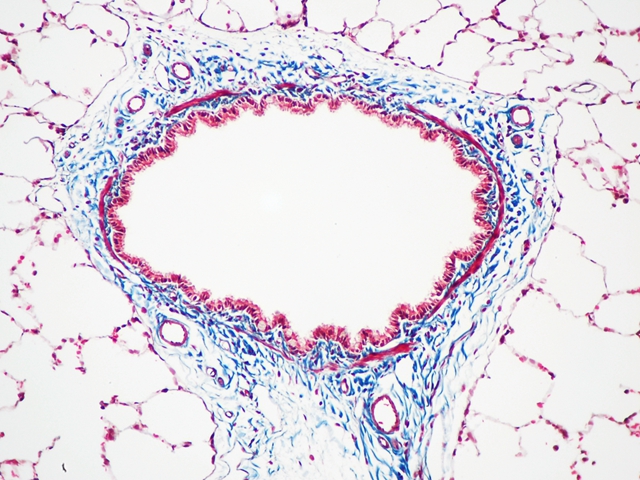
Three-color staining is mainly used to distinguish collagen fibers from muscle fibers and other components, including the following aspects:
⑴ Differentiate scar tissue from amyloid or cellulose.
(2) Differentiate whether the spindle cell tumor is fibrous, myogenic or neurogenic.
⑶ It was confirmed that there was a small amount of proliferating collagen fibers between the lobules of early liver cirrhosis.
⑷ The scar in myocardial infarction was confirmed at autopsy.
Knowledge 2: Application of Reticulate Fiber Dyeing
Reticulate fiber dyeing can be used to confirm the reticulated fiber and base membrane. The diagnosis and application of reticular fiber staining in pathology are shown in the table.
| Serial number | Differential diagnosis | content |
| 1 | Cancer and Sarcoma | Reticulum fibers surround the nest of cancer cells, and in most sarcomas they surround each tumor cell |
| 2 | Hemangioendothelioma and Hemangiopericytoma | The former tumor cells are located in the reticular fiber stent of the blood vessel wall, and the latter are located outside the reticular fiber stent of the blood vessel wall, and the reticular fibers are radially surrounding the tumor cells |
| 3 | Benign and malignant lymph node lesions | The reticular fiber scaffold of benign lesions can be clearly retained, while the reticular fiber scaffold of malignant lymphoma is squeezed or destroyed and disappears, and the reticular fiber surrounding the cancer nest can be seen in lymph node metastatic cancer. |
| 4 | Central Nervous System Tumors | There are no reticular fibers in the tumor cells and glial of astrocytoma. The reticular fibers are scattered in the tumor in meningioma, while the proliferating reticular fibers are located around the cancer nest or between the tumor cells in metastatic cancer or sarcoma. |
| 5 | Carcinoma in situ and early invasive carcinoma | The former basement membrane is intact, the latter basement membrane breaks through and disappears. It is easier to judge if PAS dyeing is done at the same time |
| 6 | Tuberculosis and Sarcoidosis | Proliferative tuberculosis has no obvious caseous necrosis, but the reticular fibers in the lesion are reduced or disappeared, while the reticular fibers inside and outside the sarcoid granuloma remain or increase |
| 7 | Liver disease | Chronic active hepatitis has mild fibrosis and increased reticular fibers, while the reticular fiber scaffold is destroyed and disintegrated in the necrotic area, and collagen fibers increase; chronic congestive liver cirrhosis can show the proliferation of reticular fibers around the central vein and the inferior lobular vein |
| 8 | other | Kidney biopsy in chronic kidney disease or diabetes can confirm significant thickening of the basement membrane |
Knowledge point 3: Application of elastic fiber dyeing
The diagnosis and application of elastic fiber staining in pathology are shown in the table.
| Serial number | Differential diagnosis | content |
| 1 | Elastic fibroids | It is not easy to distinguish between elastic fibers and collagen fibers on HE slices. Elastic fiber staining can clearly show dark blue-black spherical, thick fiber, beaded and granular elastic fibers in the tumor. |
| 2 | Early Invasion of Ductal Carcinoma of Breast | In ductal carcinoma in situ, there is no elastic fiber hyperplasia around the duct and blood vessel wall, and elastic fiber hyperplasia appears in the early infiltration |
| 3 | Fibrosis elastin, pseudotumor elastin, lichen atrophic sclerosing disease, skin laxity and scleroderma | The hyperplasia, crimping, denaturation and disintegration of elastic fibers in the dermis of certain skin diseases are found in hyperelastin, elastin pseudotumor, atrophic lichen sclerosus, skin laxosis and scleroderma, etc. |
| 4 | Endocardial and Coronary Artery Fibrosis | Endocardial and coronary artery elastic fibrosis abnormally increase elastic fibers, and the level of elastic fibers in the renal blood vessels of hypertensive nephropathy increases |
| 5 | Atherosclerosis and syphilitic aortitis | In atherosclerosis and syphilitic aortitis, the elastic fibers of the arterial wall are focally damaged, broken and disintegrated, and the rupture of the elastic plate in the blood vessel during kidney transplantation indicates rejection of the graft |
| 6 | Chronic bronchitis, emphysema, bronchiectasis | It is confirmed that certain diseases such as chronic bronchitis, emphysema, bronchiectasis, and elastic fibers show degeneration and destruction when the ligamentum flavum is injured |
Knowledge point 4: Application of periodic acid-Schiff (PAS) dyeing
PAS staining method can be used to confirm glycogen, neutral mucus, basement membrane, certain fungi and parasites.
(1) Tumors that are confirmed to contain glycogen: such as hepatocellular carcinoma, renal clear cell carcinoma, lung glycogenoma, ovarian clear cell carcinoma, clear cell hidradenoma, Brenner tumor, skeletal sarcoma and Ewing sarcoma.
⑵ Confirmed glycogen: confirmed glycogen accumulation in the liver, myocardium, skeletal muscle, kidney and mononuclear macrophage cell system during glycogen accumulation.
(3) It shows the deposition of glycogen particles: It shows the deposition of glycogen particles in multiple organs (liver, myocardium and renal convoluted tubules) in diabetes.
⑷ Confirm some PAS-positive fungi: such as Candida albicans, histoplasma capsularis, cryptococcus and blastomycetes.
⑸ Identify glycogen, lipid, etc. in vacuole cells: Identify glycogen, lipid or other substances in vacuole cells by combining fat staining.
⑹ Confirmation of basement membrane breakthrough in early cancer: combined with silver staining method to confirm whether there is basement membrane breakthrough in early cancer and the obvious thickening of glomerular capillary basement membrane in some nephropathy.
⑺Diagnosis and identification of PAS-positive tumors: combined with other carbohydrate staining methods to diagnose and identify PAS-positive tumors.
⑻It is confirmed that myocardial ischemia leads to a significant reduction of glycogen in the myocardium: a significant reduction of glycogen in myocardium caused by myocardial ischemia can also be confirmed by PAS staining.
Knowledge point 5: Application of phosphotungstic acid hematoxylin (PTAH)
Phosphotungstic acid hematoxylin staining is mainly used to confirm intracytoplasmic microfilaments, such as those found in muscle fibers and glial cells. Glia, muscle fibers, cellulose, and nucleus are all purple-blue. The horizontal stripes of skeletal muscle are clearly visible. Reticulum fibers, collagen fibers, cartilage and bone are rose red or yellow, and elastic fibers are slightly purple.
Knowledge point 6: the application of mucus dyeing
The application of mucus staining in pathology is shown in the table.
| Serial number | Differential diagnosis | content |
| 1 | Mucinous epithelial tumor | Gastric cancer PAS-positive indicates gastric-type gastric cancer, when PAS-negative and AB-positive, it indicates intestinal-type gastric cancer that occurs on the basis of intestinal metaplasia |
| 2 | Chromophobe renal cell carcinoma | Chromophobe renal cell carcinoma is positive for Hale colloidal iron (blue) and can be distinguished from other types of renal cell carcinoma, which are all negative reactions |
| 3 | Mucinous mesenchymal tumor | The mucus in myxoma, myxoid liposarcoma, and myxofibrosarcoma is hyaluronic acid, AB staining is positive, but first digestion with hyaluronidase, the staining reaction turns negative, the mucus of extraosseous mucoid chondrosarcoma is strong sulfate mucus , This method cannot be used to eliminate the positive reaction of AB staining |
| 4 | Chordoma, synovial sarcoma and mucoepidermoid carcinoma, mucinous adenocarcinoma | Combining PAS staining and other mucus staining can confirm that some tumors such as chordoma and synovial sarcoma contain both mucus and glycogen, and other tumors such as mucoepidermoid carcinoma and mucinous adenocarcinoma contain only mucus but no glycogen |
Knowledge point 7: the application of neutral fat staining
(1) Diagnosis and differential diagnosis of liposarcoma and sebaceous gland tumors.
⑵ Differentiate follicular membrane tumor and ovarian fibroma, the former is positive for neutral fat staining, and the latter is negative.
⑶Diagnosis and differential diagnosis of other lipid-containing tumors, such as xanthomas, adrenal cortex tumors, malignant fibrous histiocytoma.
⑷ Shows that in lipid storage diseases (such as Gaucher’s disease, Nieman Pick’s disease, H-S-C disease) tissue cells deposit a large amount of lipids.
⑸ Confirm intravascular embolism caused by fat (fat embolism).
⑹ Confirm the fatty degeneration in certain organs (such as heart, liver, kidney).
Knowledge point 8: the application of amyloid staining
⑴ Confirm some chronic inflammation, such as amyloid deposition in chronic osteomyelitis and tuberculosis lesions.
(2) To confirm the presence of amyloid in some tumors to make the diagnosis and differential diagnosis, such as myeloma, heavy chain disease, Waldensrom macroglobulinemia, medullary thyroid carcinoma, lung small cell carcinoma and islet cell tumor.
⑶ confirmed certain genetic diseases (such as familial Mediterranean fever, familial amyloid deposition neurological disease), allergic diseases (such as rheumatoid arthritis, dermatomyositis, scleroderma and segmental enteritis), Hemodialysis and the deposition of amyloid in the heart and brain of the elderly.
⑷Diagnosis and differential diagnosis of localized amyloidosis (amyloidoma). Amyloidomas in the throat, tongue, lungs, skin, eyes and bladder can be displayed by amyloid staining to compare with other tumors and tumors. -Like lesions (such as vocal cord polyps, granulosa cell tumors, calcified epithelioma and inflammatory pseudotumor, etc.).
Knowledge point 9: the application of pro-galaxy argyrophil staining
Silver-philic and silver-philic cell staining is mainly used to confirm neuroendocrine cells and related tumors.
Most of the gastrointestinal neuroendocrine tumors (carcinoid) are positive for silverophilic staining, while a few are positive for silverophilic staining (mainly carcinoids originating in the midgut, a few originating in the hindgut), neuroendocrine tumors in other parts, such as medullary thyroid Carcinoma, pituitary adenoma, pancreatic islet cell tumor, Merkel cell carcinoma and small cell carcinoma of the skin mostly stained positively for silverophilia. In addition, these silver staining methods can also be used to verify network fibers and melanin.
Knowledge point 10: the application of pigment dyeing
The most commonly used staining methods in pathological diagnosis are hemosiderin and melanin staining. Pigment dyeing is mainly used for:
⑴Identify the pigment as hemosiderin, melanin or other pigments (such as lipofuscin, wax-like pigment, formaldehyde pigment, charcoal, etc.).
⑵The Prussian blue method can confirm that a large amount of hemosiderin is deposited in the tissue cells in hemochromatosis, and it can show that the heart failure cells in the alveoli during chronic pulmonary congestion, and the hemosiderin deposited in the tissue cells in the liver, spleen, and lymph nodes can also be confirmed. It shows bleeding in the tissue, especially the bleeding zone of old bleeding and infarction.
⑶Melanin staining can confirm malignant melanoma and other melanin-containing diseases (such as Bednar tumor, clear cell sarcoma, infant melanotic neuroma, dermatological lymphadenopathy, melanosis, acanthosis nigricans, basal cell carcinoma and seborrheic Keratosis, etc.).
⑷ Combining with other staining methods, distinguish melanosis from pseudomelanosis (colon melanosis) and hemochromatosis. Melanosis is positive for melanin staining, and pseudomelanosis and hemochromatosis are both negative for melanin staining. Prussian blue staining was weakly positive, PAS staining was positive, the latter Prussian blue staining was strongly positive, and PAS staining was negative.
Knowledge point 11: the role of enzyme histochemistry
⑴ Diagnosis of acetylcholinesterase in Hirschsprung disease.
(2) Confirm the skeletal muscle related enzymes of various myopathy.
⑶ Confirm the acid phosphatase in giant cell tumor of bone and other osteoclast giant cells (Duray acid phosphatase method), this method can also be performed on paraffin sections.
⑷ Confirm the chloroacetate esterase of myeloid cells and mast cells (Leder method). This enzyme can be confirmed on paraffin sections fixed in formaldehyde solution, and the positive reaction is red.
⑸ Confirm the tyrosinase (DOPA reaction) of melanocytes and their tumors.
⑹Prostate cancer and metastatic prostate cancer can be confirmed by prostatic acid phosphatase (PAP).
(source:internet, reference only)
Disclaimer of medicaltrend.org



