Neurology: Tenecteplase vs Alteplase in the treatment of basilar artery occlusion
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Neurology: Tenecteplase vs Alteplase in the treatment of basilar artery occlusion
Neurology: Tenecteplase vs Alteplase in the treatment of basilar artery occlusion. The authors believe that compared with the use of alteplase before EVT, the use of TNK is associated with a higher reperfusion rate.
Randomized controlled trials comparing TNK and alteplase in the treatment of BAO patients are worthwhile.
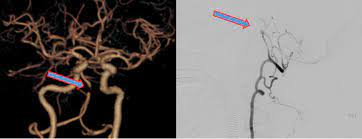
Basilar artery occlusion (BAO) is a large vessel occlusion (LVO) ischemic stroke subtype with high disability and high mortality. Although the efficacy of alteplase has been proven, only 4% of patients use it for BAO to achieve rapid reperfusion.
Tenecteplase (TNK) is a genetically modified variant of alteplase, which has higher fibrin specificity and longer half-life, allowing intravenous bolus administration.
It is better than alteplase in most countries cheaper. The EXTEND-IA-TNK trial showed that compared with alteplase, patients with LVO ischemic stroke who used TNK before endovascular treatment (EVT) had a higher reperfusion rate and a better clinical prognosis. At the first angiogram, the reperfusion rates of TNK and alteplase were 22% and 10%, respectively.
It is not clear whether this finding can be extended to BAO patients, because the study included only 6 BAO patients, and there was no difference in the primary endpoint (1/3 in each treatment group).
In March 2021, Fana Alemseged from Australia and others announced their research results on Neurology, aiming to explore the efficacy of TNK before endovascular treatment in patients with BAO.
This study retrospectively analyzed the clinical and surgical data of continuous BAO patients in the BATMAN (Basilar Artery Treatment and Management) registration study and the EXTEND-IA TNK trial, and evaluated that the reperfusion during the first angiography was >50% and no thrombus was seen. In order to compare the reperfusion rate of BAO patients using TNK before EVT, the reperfusion rate is better than alteplase.
110 BAO patients (mean age 69 [SD 14] years; median NIHSS 16 [interquartile range (IQR) 7–32]) who received IV thrombolysis before EVT were included. TNK (0.25 mg/kg or 0.40 mg/kg) thrombolysis was used in 19 patients, and alteplase (0.9 mg/kg) was used in 91 patients.
The proportion of reperfusion> 50% in the TNK group was 26% (n=5/19) and 7% (n=6/91) in the alteplase group (RR 4.0, 95% CI 1.3-12; p=0.02) Although the TNK group (48[IQR 40-71] minutes) vs the alteplase group (110[IQR 51-185] minutes; p=0.004), the time from thrombolysis to arterial puncture was shorter.
There was no difference in symptomatic intracranial hemorrhage (0/19 [0%] TNK, 1/91 [1%] alteplase; p=0.9).
In the end, the author believes that the use of TNK is associated with a higher reperfusion rate than the use of alteplase before EVT. Randomized controlled trials comparing TNK and alteplase in the treatment of BAO patients are worthwhile.
(source:internet, reference only)
Disclaimer of medicaltrend.org



