How to prevent and respond the sequelae of COVID-19?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
How to prevent and respond the sequelae of COVID-19?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
How to prevent and respond the sequelae of COVID-19? The impacts of the COVID-19 on the human body may be beyond imagination.
On March 8, “Nature” released the important research results of Gwenaëlle Douaud’s team at Oxford University in the form of “accelerated preview” [1].
After analyzing the brain scan data of hundreds of COVID-19 patients, they found that nearly 5 months after infection with the COVID-19 virus, the gray matter thickness of the orbitofrontal cortex and parahippocampal gyrus of the infected patients decreased significantly compared with the uninfected patients, and the overall brain volume was significantly reduced. Decreased, tissue damage in brain regions related to the olfactory cortex occurs even in mildly infected individuals .
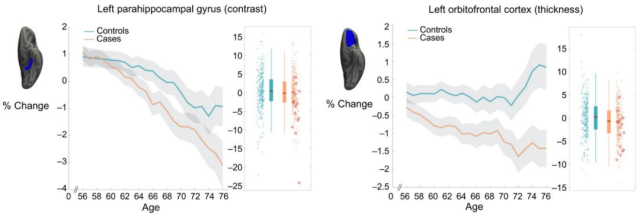
Changes in parahippocampal gyrus and orbitofrontal cortex after infection with new coronavirus[1]
Of course, it should be noted that the infected people included in this study are mainly affected by the alpha and beta mutants. Whether this conclusion is applicable to the Omicron infected people is still inconclusive. In addition, long follow-up is required to determine whether such injuries can recover gradually over time .
On the same day, the team of Professor Wang Yanjiang from Daping Hospital of China Army Medical University published an important research result in the famous journal JAMA Neurology [2], which confirmed the negative impact of the new coronavirus on the brain from a clinical point of view.
Professor Wang Yanjiang’s team analyzed the clinical data of more than 3,000 patients aged 60 and above and more than 400 family members from February to April 2020, and evaluated the cognitive changes of the patients one year after recovery. As a result, they found that after 12 months of recovery, the overall incidence of cognitive impairment in infected patients was as high as 12.45%, of which the incidence of dementia in severe patients was 15%, and the incidence of mild cognitive impairment (MCI) was as high as 26.54% ; In general, the incidence of dementia in non-severe patients is less than 1%, and the incidence of MCI is about 5%.
What is even more surprising is that the long-term impact of the COVID-19 on the nervous system is only the tip of the iceberg of the sequelae of the COVID-19. Some studies have even counted more than 50 long-term effects of the COVID-19 on the human body, and found that more than 80% of the COVID-19 infected people will suffer from at least one sequelae. influence [3]. Other studies have found that the risk of COVID-19 sequelae is much higher than that of seasonal flu [4].
According to the statistics of the World Health Organization (WHO), the number of confirmed infections in the world has exceeded 450 million [5], and this number is still rising. Combining the previous two data, it is not difficult to find that the impact of the sequelae of the COVID-19 on the global public health system may be very far-reaching .
Therefore, it is very necessary for us to fully understand the long-term effects of the new coronavirus on the human body and the human response.
COVID-19 sequelae are common and persistent
Today, the COVID-19 epidemic has been raging for more than two years. With the increase in the number of recovered patients, the long-term impact of the COVID-19 on the human body has gradually become more prominent. Up to now, the sequelae of the COVID-19 has become a major problem that human beings have to face.
Despite this, there is no unified disease definition of the sequelae of the COVID-19 in the academic community. Most institutions consider COVID-19 sequelae to be persistent health problems in recovered individuals four weeks or 30 days after the onset of symptoms [6,7]. The WHO also added “Sequelae of COVID-19” to the International Classification of Diseases code to describe health problems in which symptoms persist for at least two months and cannot be explained by other diagnoses [8].
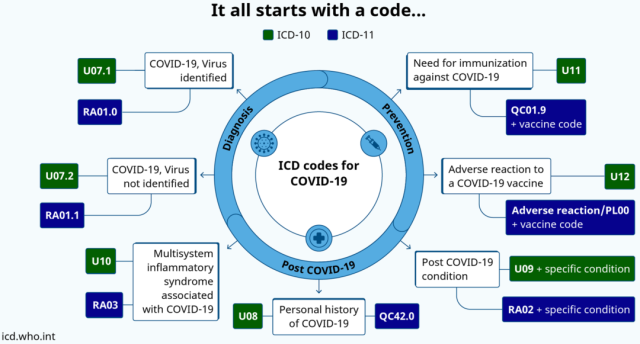
The International Classification of Diseases Code updated by WHO [9]
As early as last August, a research team led by Sonia Villapol of the Houston Methodist Research Institute (HMRI) of Weill Cornell Medical College systematically analyzed research papers on the sequelae of the COVID-19 [3]. They found that there are at least 55 sequelae of the COVID-19, and 80% of those infected have at least one sequelae.
The five most common were fatigue (58%), headache (44%), attention deficit (27%), hair loss (25%), and dyspnea (24%) . Other symptoms include lung disease (cough, chest discomfort, reduced lung diffusing capacity, sleep apnea, and pulmonary fibrosis) , cardiovascular disease (arrhythmia, myocarditis), and neurological and psychiatric disorders (dementia, depression, anxiety, obsessive -compulsive disease) etc.
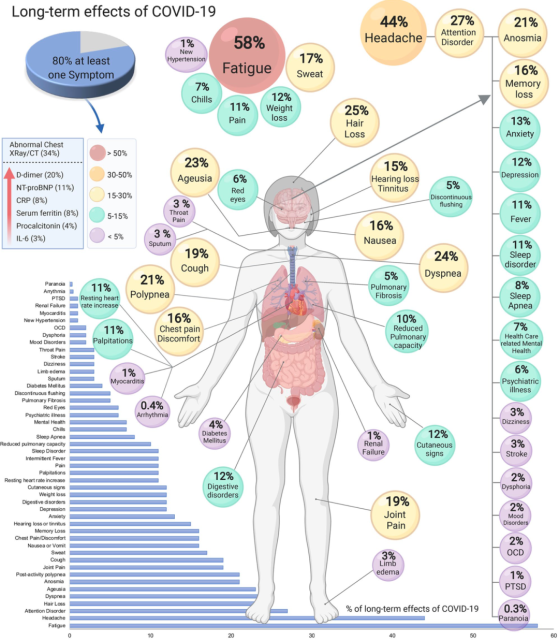
COVID-19 sequelae and proportion [3]
It is not difficult to see from the above picture that the impact of the new coronavirus on the human body affects almost all tissues or organs.
However, the most current concern is the long-term effects of the new coronavirus on the respiratory system, heart and nervous and psychiatric systems. Next, we will introduce them one by one.
The lung is the main organ of the new coronavirus infection, and the new coronavirus infection will damage the lung tissue and lung function to a certain extent, so the COVID-19 sequelae of the respiratory system are very common. In different studies, dyspnea occurred in 42%-66% of patients with a follow-up period of 60-100 days [10].
In a United States study, 6.6 percent of patients each required supplemental oxygen due to persistent hypoxemia at 60-day follow-up [10]. A research paper published by Cao Bin and others from the China-Japan Friendship Hospital showed that the incidence of dyspnea in hospitalized patients was still as high as 30% one year after discharge [11].
In a pulmonary function study , half of the patient population 30 days after discharge from recovery showed decreased lung diffusing function, decreased respiratory muscle strength, and abnormal lung imaging [12].
From the imaging results, a study found that 94% of discharged patients had abnormal lung CT images, mainly ground-glass opacity (GGO) [12]; and the abnormal lung CT images were not limited to hospitalized severe cases, but also in asymptomatic patients. These phenomena are also found in [12].
Another team studied fibrosis 3 months after discharge, and they found that about 25% of mild to moderate cases had fibrosis, and in the cohort with more severe cases, about 65% of those who recovered had pulmonary fibrosis [ 10].
Cao Bin and others followed up the hospitalized patients for one year and showed that 55.1% of the patients had at least one abnormal CT phenotype [11].
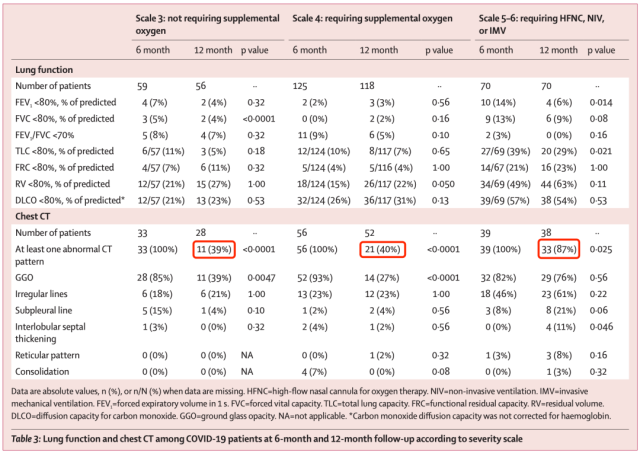
One year after illness, 55.1 percent had at least one abnormal CT phenotype [11]
From the above data, we can find that the impact of COVID-19 pneumonia on the respiratory system is very far-reaching, and the long-term impact on critically ill patients is greater.
Although not the main infection organ of the new coronavirus, the cardiovascular situation is the same as that of the lungs.
In early February this year, a research team led by Ziyad Al-Aly of Washington University School of Medicine published a research paper on the long-term effects of the COVID-19 on the cardiovascular system in the journal Nature Medicine [13]. The findings came as a surprise to some scientists.
The Al-Aly team collected clinical data from 153,760 COVID-19 patients from the U.S. Department of Veterans Affairs, as well as a concurrent control group of up to 5,637,647 participants and a historical control group of 5,859,411 participants, with a median follow-up of nearly one year , to assess the occurrence of 20 cardiovascular diseases including cerebrovascular disease, arrhythmia, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure and thromboembolic disease.
The findings showed that COVID-19 infection was associated with a 63% increase in any cardiovascular outcome and an increase in major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke and all-cause mortality) at up to 1 year of follow- up55 % related . Specifically, the risk of COVID-19 infection and cerebrovascular disease increased by 53%, the risk of arrhythmia increased by 69%, the composite risk of cardiac or pericardial inflammatory disease increased by 102%, the risk of ischemic heart disease increased by 66%, the risk of thromboembolic disease A 139% increase was associated with a 72% increased risk of heart failure.
The Al-Aly team also found that during the 1-year follow-up period, patients with COVID-19 disease who did not require hospitalization also had an increased risk of cardiovascular disease, and cardiovascular disease outcomes were positively correlated with the severity of the patient’s COVID-19 . Therefore, Al-Aly and his colleagues call for cardiovascular disease to be a concern when providing care to people who have recovered from Covid-19.
Image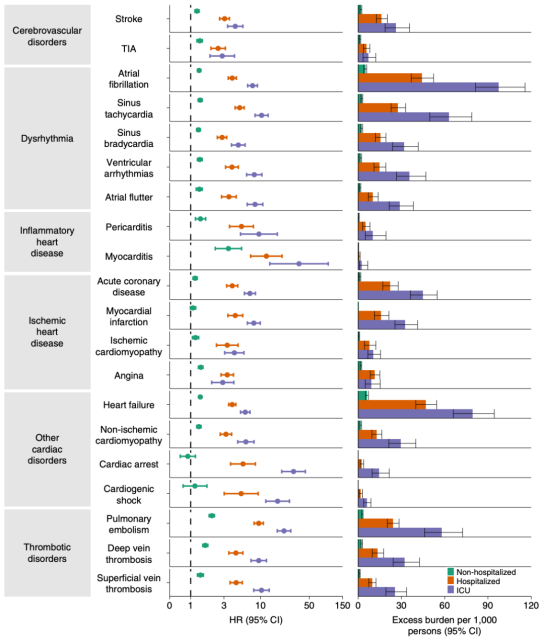 severity and cardiovascular disease risk after 1 year of follow-up [13]
severity and cardiovascular disease risk after 1 year of follow-up [13]
Finally, let’s take a look at the mental health issues that have been getting a lot of attention during the COVID-19 pandemic.
In mid-February this year, the research team led by Ziyad Al-Aly published a research paper on the long-term effects of the COVID-19 on mental health in the British Medical Journal (BMJ).
Like the previous study, this study used data from the U.S. Department of Veterans Affairs, including 153,848 participants who were infected with the COVID-19 for more than 30 days, 5,637,840 non-infected control groups during the same period, and 5,859,251 historical control groups. The follow-up period was 1 year.
From the findings, the COVID-19 group had a 60% increased risk of a diagnosis or prescription of a mental health event compared to the control group . Specifically, the COVID-19 group had a 35% increased risk of anxiety, a 39% increased risk of depression, a 38% increased risk of stress and adjustment disorders, a 55% increased risk of antidepressant use, and a benzodiazepine use. Risk increased by 65%. In addition, the Covid-19 group had an 80% increased risk of cognitive impairment and a 41% increased risk of sleep disturbance.
As with cardiovascular disease risk, non-hospitalized COVID-19 patients also had an increased risk of a diagnosis or prescription of a mental health event, and the risk of a diagnosis or prescription of a mental health event was positively associated with the severity of the patient’s illness . In addition, COVID-19 was associated with an increased risk of mental health outcomes in hospitalized and non-hospitalized patients compared with seasonal influenza.
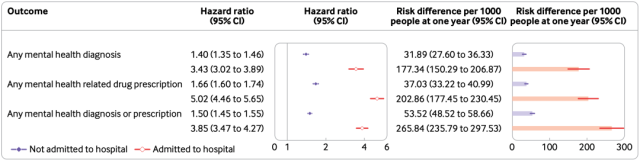
COVID-19 severity and risk associated with mental health events after 1 year of follow-up [14]
The impact of the COVID-19 on the human body is extensive and far-reaching. Whether it is a severe patient who needs to be hospitalized or a mild to moderate patient who does not need to be hospitalized, they are at very high risk of the sequelae of the COVID-19. Therefore, understanding the reasons behind the sequelae of the COVID-19 and the means to avoid the sequelae of the COVID-19 can reduce the disease burden of the recovered patients.
So what is the cause of the COVID-19 sequelae?
Possible causes of COVID-19 sequelae
Actually, we don’t have a definite answer at the moment .
However, based on the results of existing basic research and clinical research, scientists already have a preliminary understanding of the mechanism of the sequelae of the COVID-19.
Before formally introducing various speculated mechanisms, we also need to understand why the new coronavirus can affect almost all tissues or organs in the human body.
Simply put, the new coronavirus can enter a variety of tissues or organ cells through angiotensin-converting enzyme 2 (ACE2) throughout the human body.
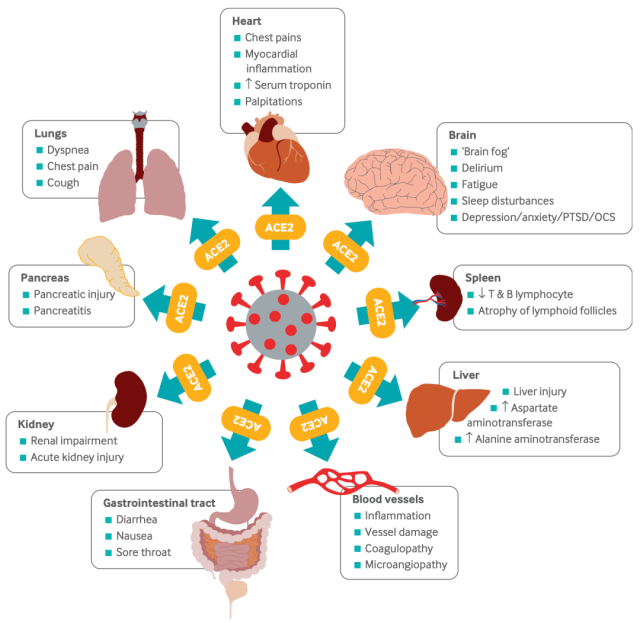
The new coronavirus can enter cells of various tissues or organs through the ACE2 receptor [15]
With the above background, we can look at the possible mechanism of the COVID-19 sequelae.
The first possible mechanism is cell or tissue damage directly caused by SARS-CoV-2 infection .
Some studies have found that in the respiratory system, the replication of the new coronavirus in endothelial cells can cause serious damage to the lungs and respiratory tract [15]; in the cardiovascular system, the new coronavirus directly infects cardiomyocytes and endothelial cells, leading to apoptosis of cardiomyocytes. apoptosis and endothelial cell damage [15,16].
In other tissues and organs, the infection of the new coronavirus will also lead to the death of related cells, which in turn affects the function of the organs and induces the sequelae of the COVID-19.
The second is a potential reservoir of viruses or fragments of non-infectious new coronaviruses that trigger chronic inflammation [12].
Many studies have detected the presence of the new coronavirus in various organs of infected people, so these organs may become potential “virus reservoirs” for the new coronavirus. Some studies exploring the shedding period of the new coronavirus have provided indirect evidence for the existence of virus reservoirs. For example, some patients had viral shedding for longer than 3 months.
In addition to the virus library, there are also studies suggesting that part of the nucleic acid sequence of the new coronavirus can be integrated into the human genome, and the new coronavirus segments integrated into the human genome can be transcribed normally [17].
Perhaps it is the chronic inflammation caused by the persistent existence of virus reservoirs or virus fragments that causes the sequelae of the COVID-19.
The third guess is chronic COVID-19 pneumonia-related immune depletion [12].
It is well known that if immune cells are stimulated by antigens for prolonged periods of time, they can become dysfunctional or even exhausted.
Studies have found that the absolute number of antiviral lymphocytes such as cytotoxic T lymphocytes (CTL) and natural killer cells (NK) in severe COVID-19 patients is significantly reduced and their functions are exhausted .
Studies have also found that during the COVID-19 infection, the expression levels of many immunosuppressive receptors on lymphoid and bone marrow cells are up-regulated.
This immunosuppression and depletion of immune cells may promote COVID-19 infection, which in turn leads to COVID-19 sequelae.
It is worth noting that the T cell receptor (TCR) on T cells may bind to specific epitopes of the new coronavirus S protein, mimicking bacterial superantigens.
If SARS-CoV-2 persists, these antigens may trigger overactivation of the adaptive immune system, triggering low-level chronic inflammation and paving the way for the aftermath of Covid-19.
A fourth potential mechanism is virus-induced autoimmunity [12].
Studies have shown that new coronavirus-specific antibodies can cross-react with mammalian host proteins.
In fact, research teams have already detected anti-neuronal autoreactive antibodies in COVID-19 patients with neurological symptoms . In a study of COVID-19 patients, researchers found that 52 percent of patients had antiphospholipid antibodies.
Antibodies against other human proteins have also been found in other clinical studies .
These evidences suggest that SARS-CoV-2-induced autoimmunity may play an important role in the occurrence of SARS-CoV-2 sequelae.

New coronavirus (Photo source: NIAID-RML)
A fifth possible cause is abnormal immune metabolism and mitochondrial dysfunction [12].
Mitochondria are not only the energy factories of cells, they are also critical for immune homeostasis in the body. Therefore, impaired mitochondrial function will inevitably affect human immunity.
As early as the beginning of the outbreak of the COVID-19 virus, scientists have studied the interaction between the proteins encoded by the new coronavirus and human proteins. Based on these studies, scientists speculate that the non-structural proteins (NSPs) 4 and 8 of the new coronavirus, as well as ORF9c, can interact with mitochondria. Some studies have also found that the new coronavirus can hijack the host’s mitochondria .
From clinical research data, peripheral blood mononuclear cells (PBMCs) of patients with COVID-19 show mitochondrial dysfunction, metabolic changes and high levels of mitochondrial factors . Other studies have found mitochondrial dysfunction in different subsets of T cells, as well as an increased risk of death.
Mitochondrial dysfunction can lead to an imbalance of immune homeostasis on the one hand and metabolic reprogramming of infected cells on the other. The two may be the driving force behind the sequelae of the COVID-19.
The last possible mechanism is the imbalance of the renin-angiotensin system (RAS) [12].
RAS plays an important role in maintaining the physiological balance of the body, and it affects the function of multiple organ systems. Studies have found that RAS is unbalanced during COVID-19 infection, and this imbalance is associated with multiple organ damage associated with COVID-19.
Therefore, scientists speculate that RAS imbalance during COVID-19 infection may lead to end-organ damage such as the lungs, heart, kidneys, and small intestine , which may be the cause of COVID-19 sequelae.
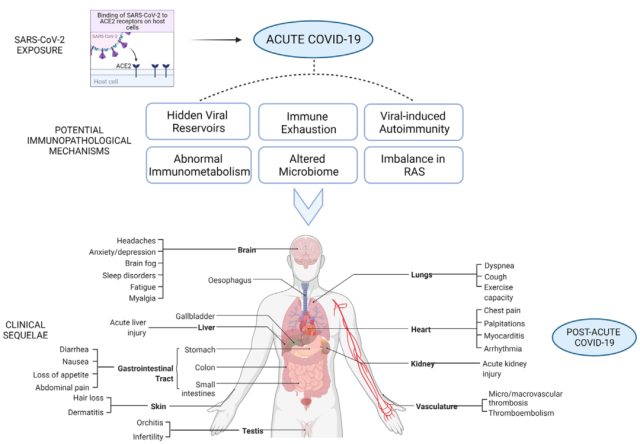
Potential mechanisms of COVID-19 sequelae[12]
In general, there may be many reasons for the sequelae of the COVID-19, and these mechanisms may overlap to varying degrees , and ultimately lead to the occurrence and development of the sequelae of the COVID-19.
However, the above six possible mechanisms are speculations made by researchers based on basic or clinical research. As for the true pathogenesis of COVID-19 sequelae, more research needs to be conducted by researchers.
Do a good job in the prevention and management of COVID-19 sequelae
Summarizing all the above, it can be seen that the COVID-19 sequelae affects many tissues or organs, with various forms and complex mechanisms, and it has a far-reaching impact (can last for more than 1 year) and has a high incidence (severely ill patients are more affected).
With the emergence and prevalence of new mutant strains, the number of COVID-19 infections will continue to rise, and the sequelae of the COVID-19 will inevitably become a new global public health problem, bringing a huge disease burden to human society (of course, for the weakened virulence ) Whether the Omicron variant will also cause the above-mentioned COVID-19 sequelae still needs to be further confirmed by clinical research) .
Therefore, it is necessary for us to formulate reasonable prevention and treatment strategies based on the existing research results to minimize the impact of COVID-19 sequelae on humans.
Judging from recent research results, the most important strategy for preventing the sequelae of the COVID-19 is vaccination .
As long as you are not infected with the COVID-19 virus, there will be no COVID-19 sequelae.
At present, a variety of vaccines have been approved for marketing around the world, no matter which vaccine can effectively prevent the COVID-19, or prevent the infection from progressing to severe disease. This reduces the risk of COVID-19 sequelae.
Recent studies have found that even if a breakthrough infection occurs after vaccination, the risk of COVID-19 sequelae is lower than that of unvaccinated infected people [4].
High-risk groups can do pre-exposure prophylaxis . Not long ago, the FDA has approved the combination of a higher dose of long-acting neutralizing antibody Evusheld for pre-exposure prophylaxis of the COVID-19 [18].
As long as the risk of contracting the COVID-19 can be greatly reduced, the risk of COVID-19 sequelae can be reduced.
For already infected patients, if the risk of progression to severe disease is relatively high, they can receive small molecule antiviral drugs (such as Paxlovid, etc.) or monoclonal neutralizing antibodies (such as ambavirumab/romisevirumab, etc.) treatment , reducing the risk of progression to severe disease [19-21].
This may also reduce the risk of COVID-19 sequelae. After all, several studies have found that compared with severe or hospitalized patients, mild patients have a relatively lower risk of COVID-19 sequelae [13,14].
In addition, some studies have shown that early application of antiviral drugs can accelerate virus clearance in the body [21,22]. However, it is still unclear whether early treatment of infection can reduce the risk of COVID-19 sequelae.
Long-term follow-up data or real-world studies of approved therapeutic drugs in phase III clinical studies may give us a clear answer.
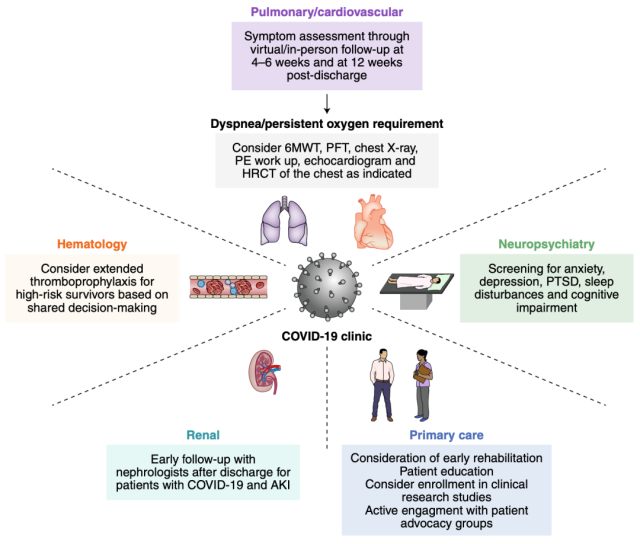
Multidisciplinary nursing strategies for COVID-19 sequelae[10]
Even those who have recovered from the COVID-19 have potential ways to reduce the aftermath of the COVID-19.
At the end of last year, a research team led by Daniel Ayoubkhani of the Office for National Statistics of the United Kingdom found that one dose of the COVID-19 vaccine after recovery from the COVID-19 was associated with a 13% reduction in the risk of COVID-19 sequelae; if two doses were vaccinated, this benefit will be expanded [ twenty three].
Of course, whether vaccination can reduce the incidence of COVID-19 sequelae in recovered patients still requires rigorous clinical research.
Unfortunately, there is no clear and effective method for treating the sequelae of the COVID-19 .
Therefore, on the basis of optimizing the vaccination of the COVID-19, doing a good job in the COVID-19 and prevention, researchers also need to explore the mechanism of the COVID-19 sequelae, and have an in-depth understanding of the causes of the COVID-19 sequelae in order to Find effective treatments.
In addition, in terms of the care of recovered patients, a multidisciplinary and collaborative outpatient clinic needs to be established to minimize the impact of COVID-19 sequelae on recovered patients.
Consequently we still have a long way to go to deal with the sequelae of the COVID-19.
References:
[1].Douaud, G., Lee, S., Alfaro-Almagro, F. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature (2022). https://doi.org/10.1038/s41586-022-04569-5
[2].Liu YH, Chen Y, Wang QH, et al. One-Year Trajectory of Cognitive Changes in Older Survivors of COVID-19 in Wuhan, China: A Longitudinal Cohort Study. JAMA Neurol. 2022; doi:10.1001/jamaneurol.2022.0461
[3].Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. Preprint. medRxiv. 2021;2021.01.27.21250617. doi:10.1101/2021.01.27.21250617
[4].Al-Aly Z, Bowe B, Xie Y. Long Covid after Breakthrough COVID-19: the post-acute sequelae of breakthrough COVID-19[J]. 2021.
[5].https://www.who.int/emergencies/diseases/novel-coronavirus-2019
[6].Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022;23(2):194-202. doi:10.1038/s41590-021-01104-y
[7].Cohen K, Ren S, Heath K, et al. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2022;376:e068414. doi:10.1136/bmj-2021-068414
[8].Deuel J W, Lauria E, Lovey T, et al. Persistence, prevalence, and polymorphism of sequelae after COVID-19 in young adults[J]. medRxiv, 2022.
[9].https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak
[10] .Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021; 27 (4): 601-615. doi: 10.1038 / s41591-021-01283-z
[11].Huang L, Yao Q, Gu X, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021;398(10302):747-758. doi:10.1016/S0140-6736(21)01755-4
[12].Ramakrishnan RK, Kashour T, Hamid Q, et al. Unraveling the Mystery Surrounding Post-Acute Sequelae of COVID-19. Front Immunol. 2021;12:686029. doi:10.3389/fimmu.2021.686029
[13.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;10.1038/s41591-022-01689-3. doi:10.1038/s41591-022-01689-3
[14].Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ. 2022;376:e068993. doi:10.1136/bmj-2021-068993
[15].Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. Published 2021 Jul 26. doi:10.1136/bmj.n1648
[16].Siripanthong B, Asatryan B, Hanff TC, et al. The Pathogenesis and Long-Term Consequences of COVID-19 Cardiac Injury: State-of-the-Art Review. JACC Basic Transl Sci. doi:10.1016/j.jacbts.2021.10.011
[17].Zhang L, Richards A, Barrasa MI, et al. Reverse-transcribed SARS-CoV-2 RNA can integrate into the genome of cultured human cells and can be expressed in patient-derived tissues. Proc Natl Acad Sci U S A. 2021;118(21):e2105968118. doi:10.1073/pnas.2105968118
[18].https://www.fda.gov/drugs/drug-safety-and-availability/fda-authorizes-revisions-evusheld-dosing
[19].Teresa Evering. Oral presentation. IDWeek 2021 Virtual Conference, Sep 29 – Oct 3
[20]. Instructions for Ambavirumab Injection / Instructions for Romisvirumab Injection (December 8, 2021)
[21].Hammond J, Leister-Tebbe H, Gardner A, et al. Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19[J]. New England Journal of Medicine, 2022.
[22].Weinreich DM, Sivapalasingam S, Norton T, et al. REGEN-COV Antibody Combination and Outcomes in Outpatients with Covid-19. N Engl J Med. 2021;385(23):e81. doi:10.1056/NEJMoa2108163
[23].Ayoubkhani D, Bermingham C, Pouwels K B, et al. Changes in the trajectory of Long Covid symptoms following COVID-19 vaccination: community-based cohort study[J]. medRxiv, 2021.
[24].https://www.cell.com/cell/issue?pii=S0092-8674(21)X0006-2#fullCover
How to prevent and respond the sequelae of COVID-19?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



