Nature: A breakthrough in cancer nutrition therapy!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Nature: A breakthrough in cancer nutrition therapy!
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Nature: A breakthrough in cancer nutrition therapy! Scientists have discovered that intestinal bacteria metabolite 3-indoleacetic acid is an “amplifier” of cancer chemotherapy response, and may improve chemotherapy effect through dietary intervention
Pancreatic cancer is called the “King of Cancer” because of its super lethality.
Judging from the 2020 global cancer data released by the International Agency for Research on Cancer (IARC)[1], the incidence of pancreatic cancer ranks 14th, but the number of deaths has rushed to the 7th .
According to research data released by the American Cancer Society last year, the 5-year survival rate of pancreatic cancer patients is 11%, and if metastasis occurs, the 5-year survival rate is only 3% [2].
This lethality is largely due to the fact that most patients are detected at an advanced stage and less than half of patients respond to commonly used treatments [3]. What is even more regrettable is that, with the development of molecular biology technology today, scientists have discovered that it is impossible to explain why patients respond differently to treatment from a genetic perspective [4].
We all know that cancer is the result of the joint action of genes and the environment. Since genes cannot explain it, we should start with the environment.
In 2019, researchers at the University of Texas MD Anderson Cancer Center took a critical step when they discovered that the survival time of patients with early-stage pancreatic cancer is closely related to the microbiome [5].
The ensuing question is whether the microbiome or the patient’s eating habits will affect the treatment effect of patients with advanced pancreatic cancer ?
On Feb. 23, a research team led by Nicola Gagliani and Samuel Huber of the Eibendorf Medical Center of the University of Hamburg, Germany , published an important research result in the famous journal “Nature” [6], pointing out a feasible solution for dietary intervention in cancer .
They found that 3-indoleacetic acid (3-IAA), produced by gut microbes metabolizing tryptophan, turned out to be an “amplifier” of chemotherapy .
It will increase the level of reactive oxygen species in the tumor, resulting in weakened autophagy of cancer cells, thereby promoting the killing effect of chemotherapy on cancer cells . If you block the 3-IAA-related pathway, the chemotherapy regimen will not work.
More importantly, short-term dietary intake of tryptophan or direct oral administration of 3-IAA can increase the chemotherapy effect of humanized mouse models of pancreatic cancer; and 3-IAA combined with different chemotherapy regimens, or treat different cancers have similar effects . This means that this new finding has broad applicability.
Screenshot of paper homepage
As mentioned at the beginning of the article, the goal of Gagliani’s team is very clear, which is to find out the extrinsic factors that affect the response of pancreatic cancer patients to chemotherapy. Gut microbes are, of course, the biggest suspects .
They recruited 23 patients with advanced pancreatic cancer, 11 of whom responded to treatment with chemotherapy (R group) and 12 who did not respond to chemotherapy (NR). There is no doubt that the prognosis of the two groups of patients is very different; similarly, the gut microbes of the two groups of patients are also very different.
To clarify the relationship between differences in gut microbes and chemotherapy responsiveness, they transplanted fecal bacteria from patients who responded to chemotherapy and those who did not respond to chemotherapy to germ-free mice, and then injected the mice with pancreatic cancer cells.
After the tumor was formed, it was treated with 5-FU, irinotecan and oxaliplatin (FIRINOX). After a period of treatment, it was found that mice transplanted with fecal bacteria from patients who responded to chemotherapy had a smaller tumor burden .
This shows that enterobacteria do affect the chemotherapy effect. However, to the surprise of Gagliani’s team, they found no bacteria in the vast majority of tumors, so they turned their attention to the metabolites of gut microbes .
After analyzing the blood components of pancreatic cancer patients and matched model mice, the tryptophan metabolite 3-IAA surfaced, and patients who responded had higher blood levels of 3-IAA compared with patients who did not respond to chemotherapy .
In addition, they identified two microbes, Bacteroides fragilis and Bacteroides thetaiotaomicron , that were at work.
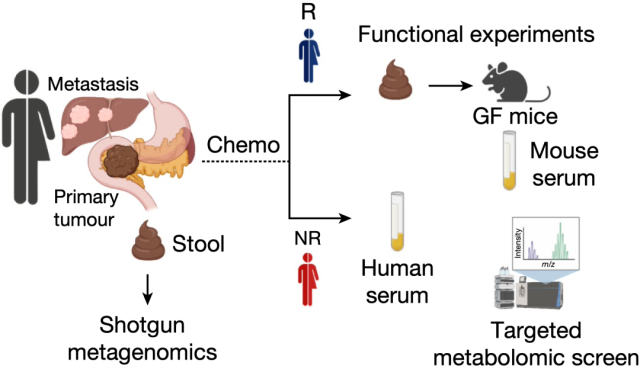
Research flow chart
The experiment has reached here, which means that the key variable has been found—that is, 3-IAA .
It is also very simple to verify the enhancement effect of 3-IAA on chemotherapy. There are two methods to choose from: one is to directly feed mice with tryptophan-rich food, and the other is to directly supplement 3-IAA. Gagliani’s team tried both.
Although the tryptophan diet is easy to implement, there is a problem. Studies have found that tryptophan can impair the anti-tumor immune response, thereby promoting tumor growth [7].
In order to determine the appropriate intervention length of the tryptophan diet, they conducted several sets of experiments, and finally found that 14 days of tryptophan diet did promote tumor growth, while 4-5 days of tryptophan diet did not .
The good news is that a 4-day diet of tryptophan was sufficient to elevate serum 3-IAA levels in mice transplanted with enterobacteria from patients responding to chemotherapy .
They noted that when a tryptophan dietary intervention was combined with FIRINOX, tumor weight decreased in mice and that serum 3-IAA levels were inversely proportional to tumor weight .
This was not the case in mice transplanted with gut bacteria from patients who did not respond to chemotherapy.
Enhancement of chemotherapy effects was also observed if 3-IAA was directly supplemented, whereas other metabolites of tryptophan did not have similar effects .
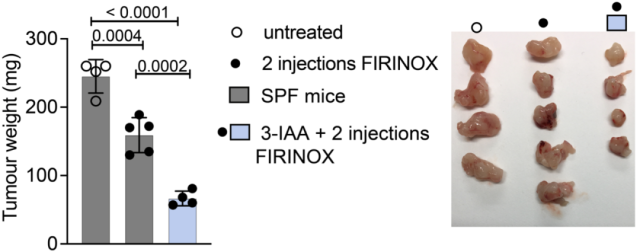
Effects of Direct Supplementation with 3-IAA
At the end of the study, Gagliani’s team examined the anticancer potential of 3-IAA.
They found that neither 3-IAA nor FIRINOX alone could prolong the survival time of mice, but the combination of the two could significantly prolong the survival time of mice .
In addition, 3-IAA combined with FIRINOX showed synergistic effects in colorectal cancer (MC38) or lung cancer (LLC) model mice, and 3-IAA combined with gemcitabine/nab-paclitaxel (GnP) in pancreatic cancer model mice .
Importantly, they found in two clinical cohorts: Serum 3-IAA concentrations were significantly associated with progression-free survival or overall survival . This means that 3-IAA may have a wide range of roles in the clinical treatment of cancer.
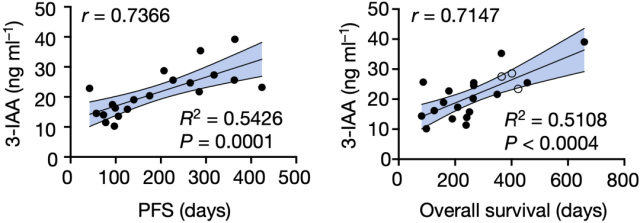
Serum 3-IAA concentrations were found to be significantly associated with progression-free survival or overall survival in a clinical cohort
As for the mechanism of 3-IAA detonating chemotherapy response, Gagliani’s team has also done in-depth exploration.
They found that this is a process that does not depend on CD8-positive T cells, but on neutrophils.
In simple terms, microorganisms such as Bacteroides fragilis and Bacteroides thetaiotaomicron in the intestinal tract will metabolize the tryptophan ingested by the human body into 3-IAA; then 3-IAA enters the blood from the intestinal tract, is absorbed by neutrophils, and is released in the bone marrow Under the action of peroxidase, 3-IAA is transformed into a toxic molecule.
This toxic molecule enters the cancer cells, causing the level of reactive oxygen species in the cancer cells to rise, inhibiting the autophagy of cancer cells. That is, at this stall, chemotherapy drugs take the opportunity Killed cancer cells .
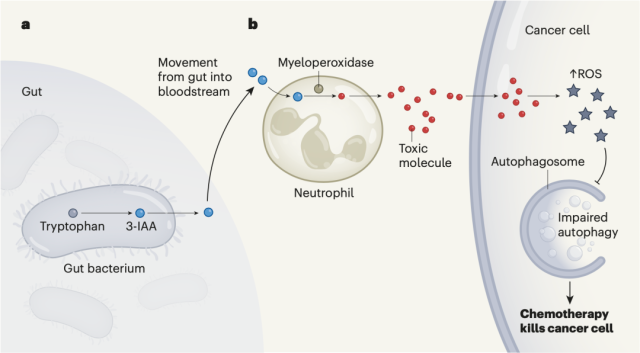
Mechanism of 3-IAA triggering chemotherapy response
Gagliani’s team believes that the 3-IAA they discovered is a key amplifier of chemotherapy response, laying the foundation for clinical research on diet combined with chemotherapy for refractory cancer.
They believe that increasing the concentration of serum 3-IAA during chemotherapy may improve the survival rate of patients who do not respond to chemotherapy .
Although it is easy to supplement tryptophan, the substrate of 3-IAA, through diet, the inhibitory effect of tryptophan on immunity cannot be ignored.
In clinical research, the intake of tryptophan and the intervention time should be well controlled, otherwise The opposite effect may occur.
In addition, tryptophan supplementation is also affected by intestinal bacteria.
If the patient lacks the necessary intestinal bacteria, the therapeutic effect will not be achieved.
In the view of Gagliani and his colleagues, it would be ideal if 3-IAA of clinical use level can be produced on a large scale, not only can exclude the inhibitory effect of tryptophan on immunity, but also need not consider the influence of intestinal bacteria.
Florencia McAllister of the University of Texas MD Anderson Cancer Center et al. published a review article on Nature at the same time [8], stating that this finding points out the direction for improving the effect of chemotherapy through nutritional intervention .
references:
[1].Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249 .doi:10.3322/caac.21660
[2]. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
[3].Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703. doi:10.1056/NEJMoa1304369
[4].Raghavan S, Winter PS, Navia AW, et al. Microenvironment drives cell state, plasticity, and drug response in pancreatic cancer. Cell. 2021;184(25):6119-6137.e26. doi:10.1016/j .cell.2021.11.017
[5].Riquelme E, Zhang Y, Zhang L, et al. Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell. 2019;178(4):795-806.e12. doi:10.1016/j.cell.2019.07 .008
[6].Tintelnot, J., Xu, Y., Lesker, TR et al. Microbiota-derived 3-IAA influences chemotherapy efficacy in pancreatic cancer. Nature (2023). https://doi.org/10.1038/s41586- 023-05728-y
[7].Hezaveh K, Shinde RS, Klötgen A, et al. Tryptophan-derived microbial metabolites activate the aryl hydrocarbon receptor in tumor-associated macrophages to suppress anti-tumor immunity. Immunity. 2022;55(2):324-340 .e8.doi:10.1016/j.immuni.2022.01.006
[8]. https://www.nature.com/articles/d41586-023-00476-5
Nature: A breakthrough in cancer nutrition therapy!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



