Even mild infection with COVID-19 can trigger long-lasting neuroinflammation
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Even mild infection with COVID-19 can trigger long-lasting neuroinflammation
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Even mild infection with COVID-19 can trigger long-lasting neuroinflammation.
Many people infected with COVID-19 twice, so is the second infection not serious?
In fact, no matter whether it is against the COVID-19 infection or influenza, it is necessary to pay attention to protection during the epidemic period , whether to be infected or not to be infected; after all, even if there is no virus infection that causes severe symptoms, it will still greatly increase the incidence of autoimmunity or other diseases of the infected person.
The potential risks of disease, not to mention COVID-19 infection, remains harmful to the elderly and immunocompromised populations.
But now there are enough vaccines for vaccination; at the same time, everyone’s attention has shifted to resuming normal life and work, and our attention has also returned to “analyzing the frontiers of biomedicine and the development trend of biomedicine through big data analysis ” above.
But recently a new article written by Dr. Eric Topol [1], reminds people: for the new coronavirus infection, whether it can be prevented or prevented as much as possible; the way It includes both immunological means such as vaccination, and physical means such as wearing masks and reducing communication during the epidemic period; especially the elderly and people with low immune function need to pay more attention to protecting themselves.
In addition, household rapid detection kits are still kept at home; once the diagnosis is confirmed, antiviral drugs such as paxlovid should be taken as soon as possible.
In this article titled “The Brain and Long Covid”, Eric used the subtitle “2 new studies shed light on persistent neuro-inflammation from even mild infections”; Prolonged neuroinflammation.
Eric first reviewed the British Biobank study published in Nature [2], comparing 400 people infected with the COVID-19 with healthy controls, through baseline (before infection) and follow-up (about 3 years later) MRI scans, It was found that people infected with the COVID-19 showed brain shrinkage, loss of gray matter and cognitive decline .

The finding raises deep concerns about the effects of coronavirus infection on the brain.
Recently, two new studies published by researchers from Germany have elucidated the mechanisms by which brain tissue develops a persistent inflammatory response in patients with even mild COVID-19 infections . It is worth noting that the subjects of these studies are people infected with the COVID-19, not specifically those who are suffering from the long-term troubles of the COVID-19.
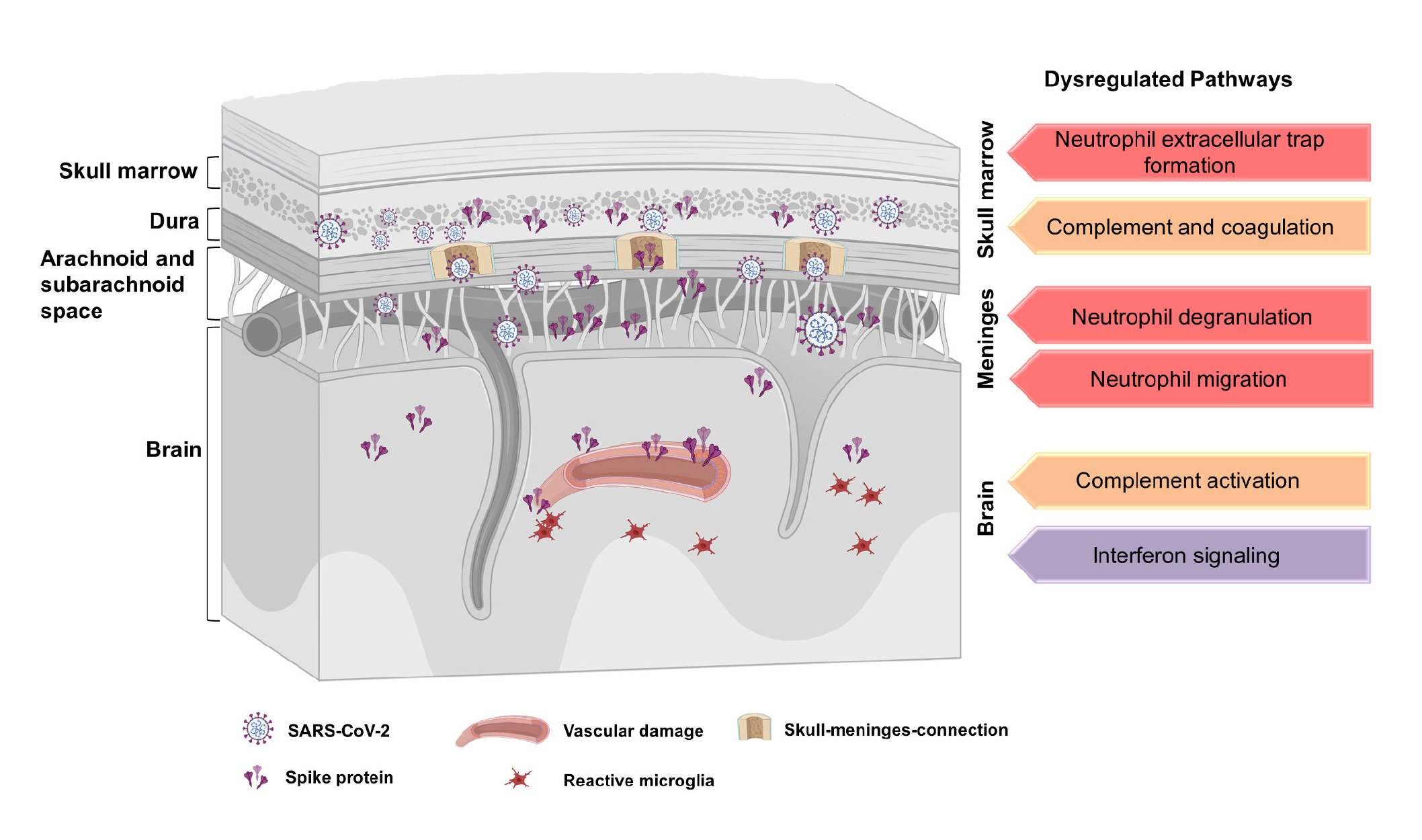
The Munich study used comprehensive imaging and omics research methods to evaluate 20 patients who died of non-COVID-19 causes but had documented COVID-19 infections [3].
Most of them (12/20) found substantial numbers of SARS-CoV- 2 spike protein accumulated , while it was not found in the control group. In the brain parenchyma, there is only the spike protein and no other parts of the virus.
In mouse models, when the spike protein was injected, brain cell damage, death, and persistent inflammation were seen. Inflammation in the skull differs compared to other bones and marrow assessed in humans and mice, reflecting the importance of this immune niche repository.
Study author Ali Erturk summarized their findings on Twitter, noting that the cranium-meningeal junction is rich in spike proteins. Persistence of the spike protein may be thought of as a factor in inflammation of the brain, according to the study .
The Hamburg study used comprehensive magnetic resonance imaging (MRI) to evaluate 11 different indicators in 223 unvaccinated people with a history of COVID-19 infection and 223 healthy controls without evidence of COVID-19 infection [4]. Unlike most patients in the UK Biobank study (15 of whom were hospitalized), 56% had only mild infections.
Imaging acquisitions were performed approximately 10 months after infection, and the main MRI findings were related to two important markers of cerebral white matter neuroinflammation—free extracellular water (FW) and mean diffusivity (MD).
There were no differences in neuropsychiatric scores between people infected with the COVID-19 and controls, including no evidence of worse cognitive function.
Abnormalities in MRI inflammatory markers were so evident that machine learning could accurately distinguish which scans were from people infected with COVID-19 and which were from controls.

Unlike the UK Biobank study,
1) All people participating in this study were not vaccinated, which eliminated the possible confounding effects of the COVID-19 vaccine;
2) These two studies did not specifically select long-term patients with COVID-19 pneumonia as research subjects.
The brain inflammation they found does not depend on symptoms, and in many cases, the central nervous system process develops asymptomatically.
However, many previous studies have linked the presence and extent of inflammation (via cerebrospinal fluid or blood markers) to long-term COVID-19 neurological symptoms, such as brain fogging, memory loss, cognitive impairment, and sleep disturbance.
A common theme of the two new German studies is the persistence of neuroinflammation, both histological and imaging findings, that persist months after COVID-19 .
Persistence of 2019-nCoV or its components, such as the spike protein, may be a driver of long-term multi-organ involvement in 2019-nCoV, an underlying mechanism that was recently reviewed and strengthened in new reports.
In response to these latest findings, Wes Ely, an intensive care physician at Ftanderbilt University, recently published an article in the Boston Globe calling for increased public awareness of the long-term covid-19:
“Many studies have documented the horrific effects of long-term COVID-19 on the brain, from the loss of the brain’s supportive cells, the glial cells, to the early dementia symptoms caused by the premature death of our neurons, many of which were only seen during the initial COVID-19 infection. It has been seen in long-term COVID-19 patients with mild symptoms of infection, even in young people.”
Indeed, associations with neurodegenerative diseases, including Alzheimer’s disease, following infection with a variety of viruses have been established.
Editor’s note:
Based largely on two recent studies, Dr. Eric Topol took an in-depth look at the impact of the new coronavirus on the brain, especially the long-term effects of neuroinflammation.
Research reveals that neuroinflammation may persist long-term after even mild infection with the new coronavirus .
The impact of the COVID-19 infection on the nervous system needs to be paid attention to; the more critical issue is that effective means must be found to reduce and treat these persistent inflammation and neurological symptoms. These are important and unresolved clinical research issues in recent years .
references:
【1】https://erictopol.substack.com/p/the-brain-and-long-covid
【2】 Douaud G, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022 Apr;604(7907):697-707. doi: 10.1038/s41586-022-04569-5 . Epub 2022 Mar 7. PMID: 35255491; PMCID: PMC9046077.
【3】https://www.biorxiv.org/content/10.1101/2023.04.04.535604v1.full.pdf
【4】https://www.pnas.org/doi/epdf/10.1073/pnas.2217232120
Even mild infection with COVID-19 can trigger long-lasting neuroinflammation.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.