Melanoma cells transform lymphatic vessels and promote tumor metastasis
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
Melanoma cells transform lymphatic vessels and promote tumor metastasis
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Nature Cancer: Scientists have discovered that melanoma cells release exosomes to transform lymphatic vessels and promote tumor metastasis.
With the expansion of cognition, scientists have discovered that tumors do not treat themselves as outsiders in our body at all, and even immune cells can in turn create a comfortable home for themselves.
Therefore, a large number of studies have turned their attention to the tumor microenvironment and no longer confine their thinking to the tumor cells themselves.
In 2012, Héctor Peinado from the Spanish National Cancer Research Center (CNIO) and his team discovered that tumor cells can transmit information to the surrounding microenvironment through exosomes [1].
Seven years later, Peinado and his team published an article in the “Nature” sub-issue that exosomes released by melanoma cells reach the lymph nodes and are mainly absorbed by lymphatic endothelial cells (LECs).
These exosomes secrete a nerve growth factor receptor-NGFR to change the phenotype of LECs, increase the branching of lymphatic vessels, and strengthen the adhesion to tumor cells, thereby promoting tumor metastasis [2].
It is also proposed that NGFR can be used as an important biomarker for the progression and early diagnosis of melanoma .
Those who have “moles” say: If the pigmented moles are asymmetrical, with uneven edges, unclear boundaries, large diameters, and uneven colors, then be wary of the possibility of melanoma!
The incidence rate of melanoma in some countries is 0.6 per 100,000, which mainly harms young and middle-aged people, and most of the patients are in the middle and late stages when they are diagnosed.
Among them, the 5-year survival rate of advanced patients is only 4.6%. Moreover, 90% of American melanomas are located in the trunk of the body, which is closely related to ultraviolet radiation; but our melanomas “a bit of their own ideas”, 41.8% of melanomas originate in the soles of the feet, toes, palms and undernails.
At the extremities, the ultraviolet rays are not illuminated at these positions, and the cause is not clear.
Melanoma [3]
Melanoma “runs away” very quickly in the early stage, and the first stop of its spread is the lymph nodes.
Studies have confirmed that melanoma can induce lymph node tissue changes, such as enhancing lymphangiogenesis, inducing an immunosuppressive environment, etc., thereby forming a pre-metastasis niche (PMN) in the lymph node [4].
This time Peinado and his team discovered that exosomes are the advances sent by the melanoma to the lymph nodes.
They selected three melanoma cell lines with different levels of metastasis to construct a mouse model: B16-F1 (low metastatic level) cell line, B16-F10 (high metastatic level) cell line, B16-F1R2 (has occurred) B16-F1) cell line with lymph node metastasis.
The results found that in mice with high levels of melanoma metastasis , the exosomes released by melanoma cells were more widely distributed, mainly concentrated in the popliteal lymph nodes, the level of exosomes aggregation was higher, and the accumulation rate was faster .
Moreover, the exosomes released by melanoma cells with high metastasis levels can enhance tumor colonization and promote the spontaneous metastasis of melanoma .
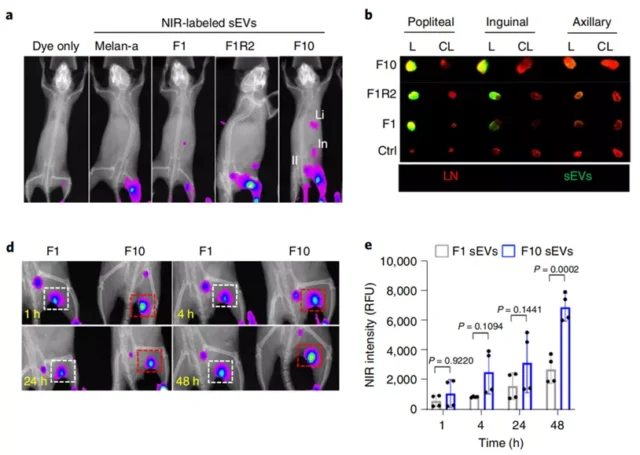
Exosomes released by highly metastatic melanoma cells accumulate faster and more in lymph nodes
So, what kind of preparations did this advance soldier make to the lymph nodes in order to help melanoma realize its expansion plan?
The researchers found that the exosomes released by melanoma cells are mainly absorbed by macrophages and LECs in the lymph nodes.
Among them, compared with macrophages, the absorption rate of LECs is faster. In a short period of time (4h), 89% of LECs have absorbed exosomes, and the absorbed quantity is also higher .
Further analysis of the human metastatic melanoma (SK-MEL-147) cell line showed that the exosomes are a major modification of the phenotype of LECs .
On the one hand, exosomes can enhance the adhesion of LECs to melanoma cells .
After LECs absorb exosomes, the expression of ICAM-1 is up-regulated. And ICAM-1 has been shown to help melanoma cells to pass through the LECs monolayer and cause tumor metastasis [5] .
The researchers found that once ICAM-1 in LECs is removed, the effect of exosomes on the adhesion of LECs is eliminated .
In addition, the expression levels of other proteins and genes related to cell adhesion and extracellular matrix reorganization have also been up-regulated, such as HLA-DRB1, TNC, EDIL3, and so on.
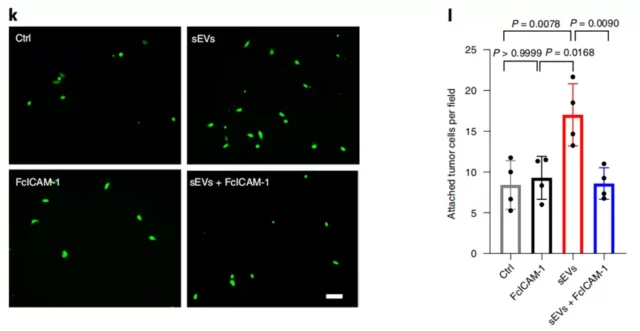
LECs become sticky after eating exosomes, and cannot be separated from ICAM-1
On the other hand, exosomes can also promote the proliferation of LECs, resulting in increased lymphatic branching , and lymphangiogenesis is also an important link in inducing an immunosuppressive environment before tumors metastasize to lymph nodes.
Researchers have observed that 48 hours after LECs absorb exosomes, lymphangiogenesis and angiogenesis-related signals (LYVE1, VEGFC, VEGFR3, etc.) are enriched.
When treating LECs with exosomes released from B16-F1R2 cells, LECs can proliferate up to 3.5 times after 24 hours .
Image
LECs are growing well after eating exosomes
It is worth noting that studies have shown that macrophages in the lymph nodes secrete lymphangiogenic factors [6].
But here, no changes in the levels of lymphangiogenic factors were observed after the macrophages absorbed exosomes.
Instead, it was discovered that these macrophages have the effect of inhibiting the abnormal growth of lymphatic vessels.
In other words, the exosomes released by melanoma cells will first reach the lymph nodes, where they will be absorbed by LECs, and then they will begin to direct the LECs to work hard to create a suitable microenvironment for the metastasis of melanoma .
So, how do exosomes “threat” LECs for their own use?
Peinado and his team first thought of NGFR. This is a nerve growth factor receptor. Studies have found that NGFR is related to melanoma metastasis and lymphangiogenesis in the process of corneal inflammation, and the expression level of NGFR in melanoma cells is higher than other types of tumor cells [7 -9].
Coincidentally, a series of studies have found that exosomes can not only induce the up-regulation of Ngfr transcription levels in LECs, but also release their own NGFR in LECs, which ultimately leads to the overall up-regulation of NGFR levels in LECs .
Moreover, only exosomes released by melanoma cells with high metastasis levels contain NGFR , and there is almost no NGFR in exosomes released by melanoma cells with low metastasis levels.
Through CRISPR technology, proteomics analysis and other technologies, the researchers found that after the level of NGFR in melanoma cells decreased, the protein components in the released exosomes also changed, and the levels of 126 proteins including NGFR were significant. Down-regulation, 281 protein levels were significantly up-regulated.
Further research results show that NGFR secreted by exosomes can induce MAPK and NF-κB pathways in LECs, thereby promoting tumor cell adhesion and lymphangiogenesis .
When NFGR inhibitor (THX-B) was used to treat melanoma mice, the metastasis of melanoma in mice was relieved .
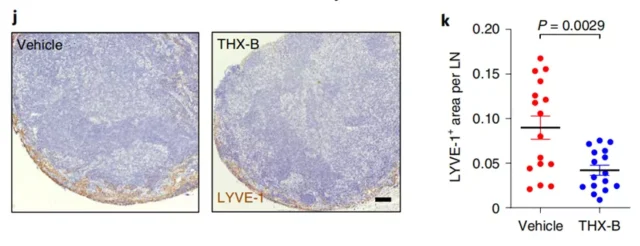
After only using NGFR inhibitors, the growth of lymphatic vessel branches in mice is alleviated
Since it is determined in mice that the expression and activity of NGFR in exosomes are a key part , what about us humans?
Peinado and his team analyzed data from The Cancer Genome Atlas and found that compared with primary melanoma, NGFR expression levels were significantly increased in metastatic melanoma .
This was also confirmed in the histological analysis of patients with stage III/IV melanoma.
Tissue biopsy results showed that compared with the primary tumor, NGFR expression levels were higher in lymph node tissues that had metastasized melanoma .
The researchers also confirmed that the number of NGFR + cells in a lymph node biopsy can be used to predict the survival of patients with melanoma .
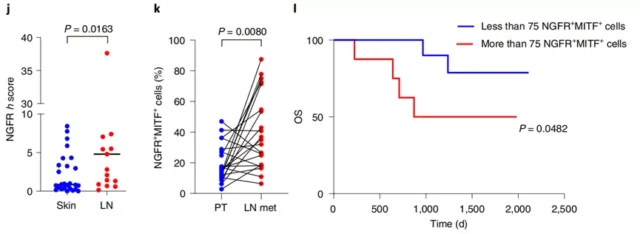
NGFR can be used as an important biomarker for melanoma progression and early diagnosis
In general, Peinado and his team found that melanoma cells can release exosomes carrying NGFR to lymph nodes, induce lymphatic branching, enhance the adhesion of lymphatic endothelial cells and melanoma cells, thereby promoting melanoma Tumor metastasis .
In this study, the researchers not only used NGFR inhibitor (THX-B) to successfully alleviate the tumor metastasis in melanoma mice , but also confirmed in melanoma patients that NGFR can be used as an effective predictive target for melanoma metastasis . This provides a new strategy for the treatment of melanoma metastasis.
References:
[1]Peinado, H. et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat. Med. 18, 883–891 (2012).
[2]García-Silva, S., Benito-Martín, A., Nogués, L. et al. Melanoma-derived small extracellular vesicles induce lymphangiogenesis and metastasis through an NGFR-dependent mechanism. Nat Cancer (2021). https:/ /doi.org/10.1038/s43018-021-00272-y
[3]https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884
[4]Sleeman, JP Te lymph node pre-metastatic niche. J. Mol. Med. 93, 1173–1184 (2015).
[5]Ghislin, S. et al. LFA-1 and ICAM-1 expression induced during melanoma–endothelial cell co-culture favors the transendothelial migration of melanoma cell lines in vitro. BMC Cancer 12, 455 (2012).
[6]Sun, B. et al. Colorectal cancer exosomes induce lymphatic network remodeling in lymph nodes. Int. J. Cancer 145, 1648–1659 (2019).
[7]Boiko, AD et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature 466, 133–137 (2010).
[8]Restivo, G. et al. Te low neurotrophin receptor CD271 regulates phenotype
switching in melanoma. Nat. Commun. 8, 1988 (2017).
[9]Civenni, G. et al. Human CD271-positive melanoma stem cells associated with metastasis establish tumor heterogeneity and long-term growth. Cancer Res. 71, 3098–3109 (2011).
Nature Cancer: Scientists have discovered that melanoma cells release exosomes to transform lymphatic vessels and promote tumor metastasis.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



