COVID-19: The Safety and 30-day prognosis undergoing tracheotomy
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
COVID-19: The Safety and 30-day prognosis undergoing tracheotomy
COVID-19: The Safety and 30-day prognosis undergoing tracheotomy. A prospective observational cohort study on the safety and 30-day prognosis of COVID-19 patients undergoing tracheotomy.
Among the surviving patients, tracheotomy patients require longer mechanical ventilation and longer ICU hospital stays.
The study titled “Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study” was published in the “British Journal of Anaesthesia”. This study is by far the largest single-institution observational cohort study of tracheostomy for COVID-19 patients. Studies have found that in patients who require mechanical ventilation due to COVID-19-related pneumonia, tracheotomy may improve the 30-day survival rate of patients. With proper patient selection, medical staff training, and medical resource allocation, it is safe to perform tracheotomy in COVID-19 patients. This may help establish a reasonable medical plan when the COVID-19 outbreak occurs in the future.
【Research Background】
COVID-19 pneumonia has become a worldwide epidemic. As of June 2020, it has spread to 213 countries and infected more than 6 million people worldwide. Although most patients have mild symptoms, about 10-17% of patients will develop acute respiratory distress syndrome and require invasive mechanical ventilation. The role of tracheotomy in the treatment of new coronavirus pneumonia is unclear, and some consensus guidelines do not recommend this treatment. The Queen Elizabeth Hospital in Birmingham, UK has established a professional airway management team and formulated relevant training programs to improve the management of COVID-19 patients undergoing tracheotomy. This article reports the outcome of the top 100 COVID-19 patients who underwent tracheotomy at the institution.
【Research methods】
This is a prospective observational cohort study of COVID-19 patients who require mechanical ventilation in the ICU of Queen Elizabeth Hospital in Birmingham, UK. The main result of the study is to compare the 30-day survival of patients with tracheotomy and non-tracheostomy patients after entering the ICU, including the state of organ function (as assessed by acute physiology and chronic health [APACHE]-II score, >17 points are recorded as Severe organ failure). Secondary results include the duration of mechanical ventilation, the time to wake up after stopping sedatives, the length of stay in the ICU, the rate of tracheostomy and extubation, related complications, and whether medical staff directly involved in the tracheostomy were infected with COVID-19. The indications for tracheotomy are shown in Table 1.
Table 1: Indications for tracheotomy
Simple respiratory failure, except patients with acute renal failure who require dialysis or continuous renal replacement therapy;
Tracheal intubation and mechanical ventilation lasted more than 10 days;
After tracheal intubation, multiple sedation failures, extubation failures, or long mechanical ventilation times are expected;
Improve oxygen demand: FiO2 <0.4, PEEP<10 cm H2O;
Normal blood clotting function;
No need for prone position ventilation
【Main Research Results】
From March 9, 2020 to April 21, 2020, the institution’s ICU admitted a total of 164 COVID-19 patients who required mechanical ventilation due to respiratory failure. Among them, 100 patients (age: 55±12; 29% women) underwent tracheotomy; 64 cases (age: 57±14; 25% women) did not undergo tracheotomy.
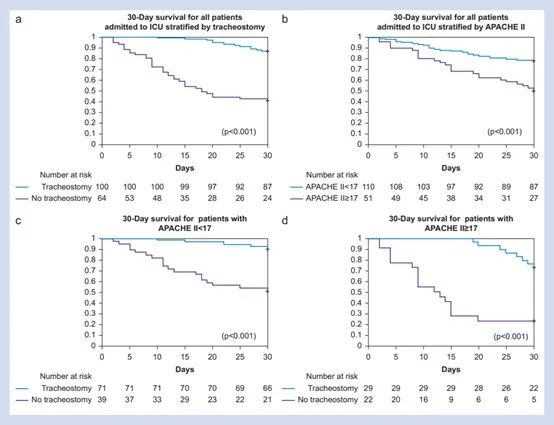
Although the APACHE-II scores of the two groups when entering the ICU were similar, the 30-day survival rate for tracheostomy patients was 85/100 (85%), while the 30-day survival rate for nontracheostomy patients was 27/64 (42%) {Relative risk: 3.9; P<0.0001}.
Among all patients with APACHE-II score ≥17, 68/100 (68%) patients with tracheectomy survived, while 12/64 (19%) patients with nontracheectomy survived (P<0.001).
Patients who underwent tracheostomy within 14 days after tracheal intubation had shorter mechanical ventilation time (mean difference: 6.0 days [95%CI: 3.1-9.0]; P<0.0001) and shorter ICU stay (mean difference: 6.7) Days [95%CI: 3.7-9.6]; P<0.0001).
No medical staff was infected with COVID-19 as a result of tracheotomy.
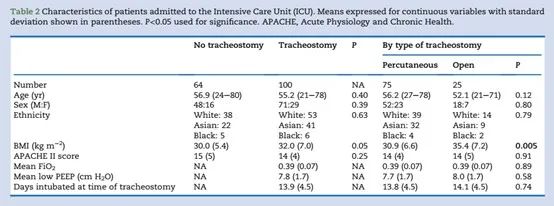
Table 2. Basic information of ICU patients included in the study
33621612429519383
35551612429519450
Figure 1. Kaplan-Meier survival curve analysis of patients 30 days after mechanical ventilation
Shown below the picture is the number at risk. (a) All patients are stratified according to whether the tracheotomy is performed. (b) All patients were stratified according to APACHE II score. (c) All patients with APA CHEII score <17 points are stratified according to whether or not the tracheotomy is performed. (d) All patients with APA CHEII score ≥17 points are stratified according to whether or not the tracheotomy is performed.
Table 3. Mechanical ventilation and recovery of surviving patients 30 days after entering the ICU
54131612429519516
Among the surviving patients, tracheotomy patients require longer mechanical ventilation and longer ICU hospital stays. Compared with patients who underwent tracheotomy 14 days after entering the ICU, patients who underwent tracheotomy within 14 days had shorter mechanical ventilation time (21 [6.0] days vs 27 [6.3] days, P=0.0001). After the tracheotomy patients were weaned with a tracheostomy mask for more than 24 hours, the mechanical ventilation was considered as the end of mechanical ventilation. There was no difference in this time between the early tracheostomy (≤14 days) group and the late tracheostomy group (>14 days). The number of days is represented by the average (standard deviation).
【Review】
This is the largest single-institution observational cohort study of patients undergoing tracheostomy for COVID-19. The survival rate of patients who underwent tracheotomy was higher than that of patients who did not underwent tracheotomy. Moreover, this result has nothing to do with the basic condition of the patients, and there was no significant difference in the basic APA CHEII scores between the two groups. The survival rate of patients with an APACHE score of <17 is higher than that of ≥17. However, regardless of the APACHE score, patients undergoing tracheotomy have a higher survival rate.
The current guidelines are mostly based on expert opinions in the absence of evidence, and this study shows that these guidelines are too conservative. It is safe to perform tracheotomy as soon as possible when there are clinical indications and the patient’s condition is appropriate, without waiting for a specific time point. This may help shorten the total time of mechanical ventilation, and in the case of a surge in the number of COVID-19 patients, more effectively increase the capacity of hospital ventilators, so that more patients have the opportunity to receive mechanical ventilation treatment.
(source:internet, reference only)
Disclaimer of medicaltrend.org



