Why does Metformin have no “Magic Power” to treat breast cancer?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Why does Metformin have no “Magic Power” to treat breast cancer?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
JAMA: Metformin has no “magic power” in the face of breast cancer! Phase 3 clinical study shows that adjuvant metformin in non-diabetic early breast cancer patients does not improve survival
For a long time, metformin has been the first choice and commonly used hypoglycemic drug for the treatment of type 2 diabetes.
In addition to sticking to his own work, metformin has also shown potential in fields such as anti-aging and longevity, improving obesity-related physiology, and even proven to have anti-cancer potential.
For example, breast cancer.
Clinical studies have shown that metformin can inhibit the proliferation of breast cancer tumor cells and inhibit tumor progression [1-4].
However, some studies have shown that the relationship between metformin and breast cancer is hard to say, and it depends on the subtype.
Taking metformin is associated with a reduced risk of estrogen receptor (ER)-positive breast cancer, but it is associated with an increased risk of triple-negative breast cancer [5] .
Can metformin fight breast cancer?
This time, Pamela J. Goodwin and colleagues from Mount Sinai Hospital in Toronto, Canada, found in a clinical study called MA.32 that for early breast cancer patients without diabetes, it is not necessary to The addition of metformin to standard care did not significantly improve patients’ invasive disease-free survival, overall survival, or other outcomes .
However, the findings point to a new clue. Adjuvant metformin therapy may have clear therapeutic benefits for patients with a specific subtype of HER2-positive breast cancer .
The article was recently published in the journal JAMA [6].
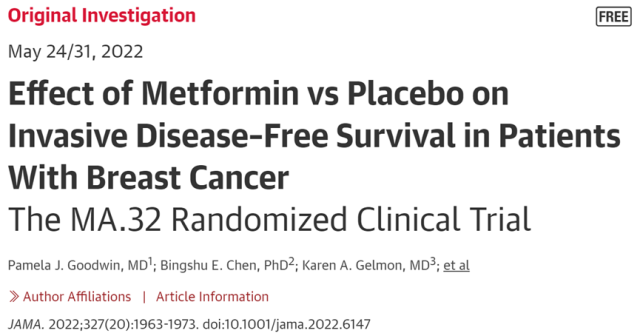
Screenshot of the paper’s homepage
Taking metformin to fight breast cancer is not imaginary.
In theory, metformin may indirectly slow down the growth of breast cancer tumors by improving the patient’s metabolism ( such as insulin levels) , or directly act on tumor cells through signaling pathways such as PI3K/Akt/mTOR and AMPK-mTOR , hindering their growth. and promote apoptosis [6].
Given the “good track record” of metformin in various fields, the clinical use of metformin in the treatment of breast cancer seems somewhat promising.
To this end, Pamela J. Goodwin and colleagues launched the MA.32 clinical trial.
A total of 3649 patients with early breast cancer (T1-3, N0-3, M0) were included in this clinical study , with an average age of 52.4 years (18-74 years), and without diabetes mellitus .
Participants were randomized 1:1 to receive placebo or metformin in addition to standard care. Oral administration of 850 mg of placebo or metformin each time, twice a day for the first four weeks, changed to once a day after four weeks of treatment. All had completed complete resection or neoadjuvant chemotherapy before enrollment.
The researchers analyzed the efficacy of metformin in patients with hormone receptor-positive (ER/PgR+) or hormone receptor-negative (ER/PgR-) breast cancer, regardless of the patient’s HER2 status.
The results showed that the addition of metformin to standard care did not significantly improve invasive disease-free survival (IDFS), overall survival (OS), distant-free survival in these early-stage breast cancer patients compared with placebo Relapse survival (DRFS), breast cancer disease-free interval (BCFI) and other outcomes .
Specifically, for ER/PgR+ breast cancer patients, the incidence of IDFS in the metformin group and the placebo group was 2.78 and 2.74 cases per 100 person-years, respectively, and there was no significant difference in IDFS between the two groups (HR 1.01; 95%CI 0.84). -1.21; P=0.93).
Metformin treatment also had no significant effect on OS in patients with ER/PgR+ breast cancer (HR=1.10; 95%CI 0.86-1.41; P=0.47), and the mortality rate was 1.46 deaths per 100 person-years in the metformin and placebo groups, respectively and 1.32 cases .
From the point of view of DRFS, metformin adjuvant therapy is even more “superfluous”. Patients with ER/PgR+ breast cancer in the metformin and placebo groups had the same rate of distant recurrence or death, 1.99 per 100 person-years (HR 0.99; 95% CI 0.80-1.23; P=0.94).
Adjuvant metformin therapy is unnecessary in patients with ER/PgR+ breast cancer
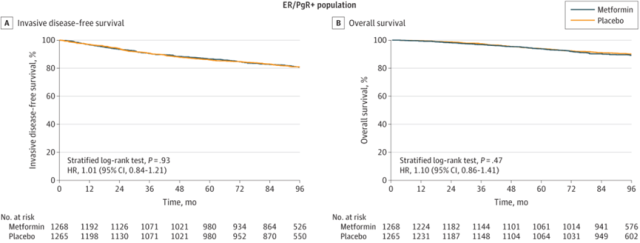
The same is true for ER/PgR-breast cancer patients.
The incidence of IDFS in ER/PgR-breast cancer patients in the metformin group was 3.58 cases per 100 person-years, the mortality rate was 1.91 cases per 100 person-years, and the incidence of distant recurrence or death was 2.35 cases per 100 person-years .
The difference in the placebo group was not significant (3.60/100 person-years, 2.15/100 person-years, 2.63/100 person-years).
Adjuvant metformin is also of little value in patients with ER/PgR-breast cancer
In addition, adjuvant metformin treatment did not result in any significant change in breast cancer-free intervals in ER/PgR+ or ER/PgR- patients compared with placebo .
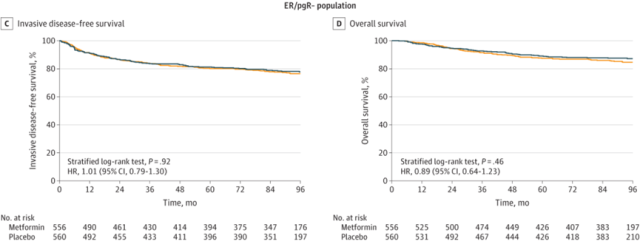
Notably, the situation shifted when the HER2 expression status of breast cancer patients was considered.
Among breast cancers, HER2-positive breast cancers tend to progress faster and are more likely to spread and recur than HER2-negative breast cancers [7].
The study included 620 patients with HER2-positive breast cancer. Compared with placebo, HER2-positive patients taking metformin had significantly longer IDFS, with IDFS event rates of 3.05 and 1.93 events per 100 person-years, respectively (HR 0.64, 95% CI 0.43-0.95, p=0.026).
At the same time, adjuvant metformin therapy also significantly improved OS in HER2-positive patients, with mortality rates of 1.43 and 0.78 per 100 person-years in the placebo group and metformin group, respectively (HR 0.53, 95%CI 0.30-0.98, p=0.0398).
Adjunctive treatment with metformin significantly improves IDFS and OS in patients with HER2-positive breast cancer
Not only that, but the researchers also assessed the safety of metformin.
The results showed that compared with the placebo group , the incidence of non-hematologic toxic events of grade 3 or higher was higher in the addition of metformin to standard care, 17.5% and 21.5%, respectively (P=0.0003) . The most common adverse events of grade 3 or higher in the metformin and placebo groups included hypertension (2.4% vs 1.9%), menstrual irregularities (1.5% vs 1.4%), and diarrhea (1.9% vs 0.8%) .
Overall, the clinical results by Pamela J. Goodwin and colleagues show that metformin is not as “magical” as expected in fighting breast cancer.
Adjuvant metformin therapy on the basis of standard therapy is not ideal for early breast cancer patients without diabetes, including invasive disease-free survival, overall survival, distant recurrence-free survival, and breast cancer disease-free. There was no significant improvement in outcomes such as interval .
In other words, metformin is not supported as adjuvant therapy for patients with early breast cancer .
However, this study also suggests that metformin may be a “tough nut to crack.” In the face of highly aggressive and highly malignant HER2-positive breast cancer, adjuvant metformin therapy can significantly prolong the invasive disease-free survival and overall survival of these patients .
Follow-up investigators will further explore the impact of metformin on patients with HER2-positive breast cancer.
It seems that the relationship between metformin and breast cancer is really a mystery.
References:
[1]Bonanni B, Puntoni M, Cazzaniga M, et al. Dual effect of metformin on breast cancer proliferation in a randomized presurgical trial. J Clin Oncol. 2012;30(21):2593-2600. doi:10.1200/JCO.2011.39.3769
[2]Niraula S, Dowling RJ, Ennis M, et al. Metformin in early breast cancer: a prospective window of opportunity neoadjuvant study. Breast Cancer Res Treat. 2012;135(3):821-830. doi:10.1007/s10549-012-2223-1
[3]Hadad SM, Coates P, Jordan LB, et al. Evidence for biological effects of metformin in operable breast cancer: biomarker analysis in a pre-operative window of opportunity randomized trial. Breast Cancer Res Treat. 2015;150(1):149-155. doi:10.1007/s10549-015-3307-5
[4]Kalinsky K, Crew KD, Refice S, et al. Presurgical trial of metformin in overweight and obese patients with newly diagnosed breast cancer. Cancer Invest. 2014;32(4):150-157. doi:10.3109/07357907.2014.889706
[5]Park YM, Bookwalter DB, O’Brien KM, Jackson CL, Weinberg CR, Sandler DP. A prospective study of type 2 diabetes, metformin use, and risk of breast cancer. Ann Oncol. 2021 Mar;32(3):351-359. doi: 10.1016/j.annonc.2020.12.008. Epub 2021 Jan 29.
[6]https://jamanetwork.com/journals/jama/fullarticle/2792615
[7]Kunte S, Abraham J, Montero AJ. Novel HER2-targeted therapies for HER2-positive metastatic breast cancer. Cancer. 2020 Oct 1;126(19):4278-4288. doi: 10.1002/cncr.33102. Epub 2020 Jul 28. PMID: 32721042.
Why does Metformin have no “Magic Power” to treat breast cancer?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



