Treatment of peritoneal metastases from colorectal cancer
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Treatment of peritoneal metastases from colorectal cancer
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Treatment of peritoneal metastases from colorectal cancer.
The global incidence of colorectal cancer is increasing year by year. In 2020, the number of patients worldwide will reach 1.9 million.
For patients without distant dissemination, surgical resection of the primary tumor and regional lymph node dissection is the only possible cure. However, some patients still develop metastases in liver, lung and peritoneum.
Risk factors for peritoneal metastases include advanced tumors, lymph node metastases, and failure to achieve radical resection of the primary tumor at the time of primary surgery.
Other risk factors for peritoneal metastases include right colon cancer, mucinous histology, and peripheral nerve and vascular invasion, and peritoneal metastases occur in about 10% of colorectal cancer patients.
The incidence of peritoneal metastasis of colorectal cancer is different between left and right colon cancer, and the incidence of right colon cancer is higher.
Peritoneal metastases from mucinous colon cancer are more common than non-mucinous colon cancer.
Tumors with RAS pathway gene mutations, stroma-rich tumors, and molecular subtype IV often metastasized to the peritoneum. In contrast to liver metastases, tumors with peritoneal metastases had fewer chromosome 20q aberrations.
Treatment of peritoneal metastases from colorectal cancer
1. Systemic chemotherapy
The standard treatment for metastatic colorectal cancer is palliative systemic chemotherapy. However, peritoneal metastases have a poorer prognosis than metastases from other sites. Reasons include:
1) Clinical status and subsequent chemotherapy are important influencing factors, which are related to the poor response of peritoneal metastatic cancer to chemotherapy;
2) Mucinous tumors and tumors of the right colon;
3) Biological behavior of tumors. Peritoneal metastases have a denser extracellular matrix, which is not conducive to the action of cytotoxic drugs.
After systemic chemotherapy, the survival time of patients with peritoneal metastases is 6 to 16 months, and the chemotherapy response rate is about 10%, while that of patients with liver metastases is about 40%.
In addition, the rate of disease progression after chemotherapy in patients with peritoneal metastases is about 20%, while the rate of liver metastases is 10%.
These data analyzes are derived from subgroup analyzes of larger randomized trials, which accounted for only 5% of the study population, and CT scans were poorly evaluated for peritoneal metastases, so the confidence in these analyses is low.
2. Intraperitoneal chemotherapy
Since the 1980s, the intraperitoneal injection of 5-fluorouracil (5-FU) in the treatment of colon cancer has attracted attention.
The intraperitoneal drug concentration of 5-FU injected intraperitoneally is 450 times that of the plasma drug concentration during intravenous administration.
Despite the dosing advantage, a better treatment effect was not found. This may be because 5-FU is insoluble in water and requires prolonged exposure to exert cytotoxic effects.
Current trials place 5-FU in slow-release polymeric micelles or gels to overcome this problem.
One of the challenges of intraperitoneal chemotherapy is that intraperitoneal adhesions can hinder the intraperitoneal distribution of chemotherapy drugs, and hydrogels can be used to solve this problem.
In 2011, a new type of intraperitoneal chemotherapy was developed. In this method, an aerosol containing chemotherapy drugs is injected into the abdominal cavity.
This method can be used for repeated intraperitoneal chemotherapy combined with systemic chemotherapy.
A study showed that among 17 patients using this treatment method, 7 had complete remission, with a remission rate of 71%, but the median survival time did not exceed 15.7 months.
3. Complete Cytoreductive Surgery
In the late 1970s, cytoreductive surgery (CRS) combined with systemic chemotherapy became available for the treatment of ovarian cancer.
After 5 years, CRS was standardized as peritonectomy. Survival of CRS combined with systemic chemotherapy in the treatment of peritoneal metastases depends on the number of peritoneal resections.
Since ovarian cancer has similar characteristics with peritoneal metastasis of appendix tumors, this therapy has also become a treatment method for peritoneal metastasis of appendix tumors. The median survival time of CRS combined with systemic chemotherapy in the treatment of colorectal cancer with peritoneal metastasis can reach 34.4 months.
4. CRS combined with early postoperative intraperitoneal chemotherapy
In the late 1990s, complete CRS combined with early postoperative intraperitoneal chemotherapy was used to treat peritoneal metastases.
The chemotherapeutic drug for this treatment is 5-FU, administered in repeated doses. A randomized trial showed that this treatment strategy can prolong the median survival of patients to 25 months.
5. CRS combined with intraperitoneal hyperthermic perfusion chemotherapy
Systemic chemotherapy combined with CRS + hyperthermic intraperitoneal chemotherapy (HIPEC) is the latest treatment stage for colorectal cancer with peritoneal metastasis.
The treatment protocol was first proposed in 1993, and has since been further developed in North America, East Asia, and Europe.
n 2003, the median survival time of the first systemic chemotherapy combined with CRS+HIPEC patients was 22 months, while the median survival time of patients receiving only systemic chemotherapy was only 12 months.
This study laid the foundation for the treatment of peritoneal cancer. This treatment regimen has been included in several national guidelines and has become the standard treatment for colorectal cancer with peritoneal metastasis. More recent studies have shown that this treatment can prolong the median survival time of patients to 3 years, and the 5-year survival rate reaches 31%.
This median survival has been validated in cohort studies, randomized studies, meta-analyses, and population-based data. The 10-year survival rate of patients who achieved complete CRS was 20%.
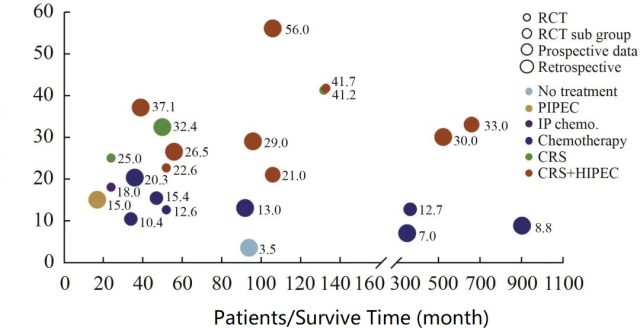
Figure 1 shows the treatment modalities for peritoneal cancer. Different treatments are indicated by different colors. The size of the bubble reflects the strength of the study’s argument, with retrospective studies being the smallest and randomized controlled trials being the largest. This figure shows the advantage of systemic chemotherapy combined with CRS+HIPEC.
After 40 years of development, a standardized treatment model of CRS, systemic chemotherapy, intraperitoneal chemotherapy, and HIPEC has been formed for peritoneal metastasis of colorectal cancer, but the contribution rate of each part to the overall efficacy needs to be further clarified.
Several studies have attempted to find out what the various parts do. There was no survival difference between systemic chemotherapy combined with CRS+HIPEC or without HIPEC.
The ongoing CARIO VI study observed the therapeutic effect of CRS+HIPEC with or without perioperative chemotherapy, and the results have not yet been published.
At present, there is a clear treatment method, that is, systemic chemotherapy combined with CRS+HIPEC, but recent randomized clinical trials have shown that there is no survival benefit for patients treated with HIPEC.
However, current guidelines state that a new treatment should only be used if it is superior to the old one.
Therefore, the treatment model of systemic chemotherapy + CRS without HIPEC is not yet supported.
In summary, systemic chemotherapy combined with CRS+HIPEC should be used as the standard treatment for peritoneal metastases, and this is the regimen with the best therapeutic effect in all reports so far.
Reference:
Verwaal Jilbert Victor. Treatment of peritoneal metastasis of colorectal cancer[J].
doi: 10.12354/j.issn.1000-8179.2022.20220835
Treatment of peritoneal metastases from colorectal cancer
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



