Why are men more likely to get colorectal cancer?
- Brief Intermittent Exercise Reduces Heart Disease and Death Risk
- Personalized Lung Tumor Chips Assess PD-1 Therapy Response
- Study Shows Prior Infection Offers Strong Immunity to Original COVID-19 Strain
- Chinese Food Products Dominate Korean Tables Amid Safety Concerns
- Early Detection of Hypopharyngeal Cancer Possible with Saliva Diagnosis
- EB Virus Could Be Infected by Kiss: A Hidden Threat Linked to Cancer
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Why are men more likely to get colorectal cancer?
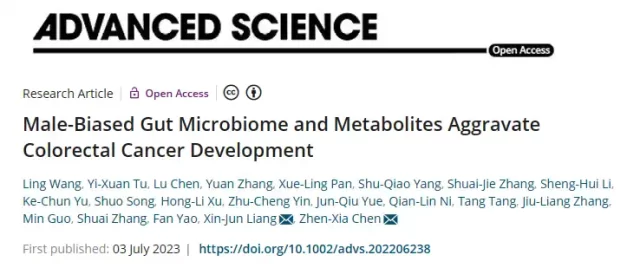
Advanced Science: The latest research reveals the mechanisms and potential therapeutic targets behind colorectal cancer sex differences!
The incidence and mortality of colorectal cancer (CRC) are higher in men than in women. This study aimed to explain the underlying causes of this gender dimorphism in CRC from the perspective of sex-biased gut microbiota and metabolites.
Sex dimorphism in colorectal tumorigenesis was observed in both ApcMin/+ mice and azomethane (AOM)/dextran sodium sulfate (DSS)-treated mice, with significantly more tumors in male mice Larger and more impaired intestinal barrier function.
In conclusion, sex-biased gut microbiome and metabolites contribute to sex dimorphism in CRC. Modulating sex-biased gut microbiota and metabolites may be a potential gender-specific therapeutic strategy for CRC.
On July 3, researchers from Tongji Medical College of Huazhong University of Science and Technology and Chen Zhenxia’s team from Hubei Hongshan Laboratory published a research article titled “Male-Biased Gut Microbiome and Metabolites Aggravate Colorectal Cancer Development” in “Advanced Science”.
A sex-biased gut microbiota and metabolites perspective to explain the underlying causes of this gender dimorphism in CRC, revealing mechanisms underlying sex differences, and arguing that modulation of sex-biased gut microbiota and metabolites may be an underlying cause Gender-specific treatment strategies for CRC.
Research Background
Colorectal cancer (CRC) is the third most common cancer and the second deadliest cancer worldwide. Notably, more men than women are diagnosed with CRC each year.
Among CRC patients, men were diagnosed at an earlier age and died on average 4-6 years younger than women.
This sex difference has attracted widespread attention because it could imply fundamental biological differences between men and women in cancer pathogenesis and response to treatment .
However, guidelines on cancer screening or treatment do not take into account gender-differentiated recommendations.
A sex-biased gut microbiome may be an underlying cause of the sex dimorphism leading to the development of CRC .
CRC is a multifactorial disease, and several CRC risk factors have been identified, such as lifestyle, genetic, and environmental factors.
The gut microbiome exerts a major influence on the central nervous system (CNS) by transmitting bidirectional biochemical signals between the gastrointestinal tract and the CNS via the gut-brain axis.
However, the relationship between a sex-biased gut microbiome and sexual dimorphism in CRC remains largely unclear.
Therefore, it is important to identify a sex-biased gut microbiome that differentially affects CRC formation in men and women.
These sex-based gut microbiomes may be valuable therapeutic targets and markers of cancer prognosis .
Various mouse models, including genetically engineered mouse models (GEMMs) and carcinogen-induced models (CIMs), have been developed in preclinical studies to recapitulate human CRC.
The ApcMin/+ mouse model is a widely used GEMM to understand the molecular processes of familial adenomatous polyposis-associated CRC initiation and progression.
While the azomethane (AOM)/dextran sodium sulfate (DSS)-induced CRC mouse model is more widely used to study inflammatory colorectal cancer.
Although sexual dimorphism has been demonstrated in CRC patients, it has not been reported in mouse models.
In this study, we used these CRC mouse models to investigate sexual dimorphism in CRC and assessed the impact of a sex-biased gut microbiota on CRC progression.
Furthermore, we found that feces from male CRC mice or human patients promoted intestinal barrier dysfunction and intestinal inflammation in pseudo-germ-free mice, suggesting that a sex-biased gut microbiome contributes to the development of CRC.
Modulating sex-biased gut microbiota and metabolites may be a potential sex-targeted therapeutic strategy for the prevention and treatment of sex-biased CRC .
Research process
Our findings in mouse models are supported by previous worldwide reports of sexual dimorphism in CRC, whereby males display higher CRC morbidity and mortality than females.
Our data showed clear differences in tumor number and size between male ApcMin/+ (standard and high-fat diet) mice or male AOM/DSS mice and their female counterparts, but this difference was evident in antibiotic-induced intestinal The gut microbiota disappears after depletion.
During CRC progression, the greatest phenotypic differences between male and female ApcMin/+ mice were observed on a high-fat diet, so we chose this model for subsequent analyses.
It was previously reported that intestinal barrier dysfunction contributes to the development of CRC.
Damage to the mucosal barrier can lead to unlimited entry of commensal microorganisms, including pathogens, into the lamina propria and even into the blood, thereby accelerating the development of CRC. Furthermore, we explored possible differences in epithelial barrier function between male and female ApcMin/+ mice.
Lipopolysaccharide (LPS), an abundant component of the gut microbiome, is involved in CRC progression and metastasis. Our enzyme-linked immunosorbent assay (ELISA) results showed increased LPS levels in the serum of male mice, consistent with reports of increased LPS levels in CRC patients and colon hyperpermeability.
In addition, our results showed that male mice had wider paragut space and lower protein expression of ZO-1, Occludin and Claudin-3 (markers related to intestinal barrier function) than female mice, indicating that male mice had Intestinal barrier function impairment was more severe compared to female mice .
Accumulating evidence indicates that the gut microbiome plays a crucial role in CRC tumorigenesis. Transplantation of feces from AOM/DSS mice into germ-free mice resulted in accelerated tumor development compared with healthy mice.
Our results further demonstrate that gavage of pseudo-germ-free mice with fecal samples from male or female mice and CRC patients has positive effects on the colonic mucosa of pseudo-germ-free mice.
We found that gut barrier function is altered depending on the sex of the fecal donor (mice or patient) but not the sex of the pseudo-germ-free mice themselves .
Pseudo-germ-free mice gavaged with feces from male mice or male CRC patients exhibited marked cell proliferation, intestinal barrier dysfunction, and intestinal inflammation.
Together, these findings suggest that the gut microbiome may play an important role in colorectal tumorigenesis .
Multiple lines of evidence have shown that sexual dimorphism in CRC is regulated by the tumor microenvironment, estrogen, and X-linked genes.
Considering that CRC patients have intestinal microbial disturbances compared with healthy people, and gender is the main factor causing the differences in gut microbiome, this study analyzed the gender bias of colorectal tumorigenesis from the perspective of gut microbiome .
Our data show that male and female ApcMin/+ mice display distinct microbiota compositions. A. inops and A. muciniphila were significantly enriched in male ApcMin/+ mice and pseudo-germ-free mice gavaged with fecal samples from male ApcMin/+ mice. A. mucinipila is an important Gram-negative anaerobic bacterium that degrades mucins in the gut. This bacterium was positively associated with colon tumor burden.
Our results showed that A. mucinipila was enriched in both male ApcMin/+ mice and pseudo-germ-free mice that received male ApcMin/+ feces.
These findings suggest that A. mucinipila acts as a potential pathogen in colorectal tumorigenesis.
Furthermore, male and pseudo-germ-free mice were gavaged with fecal samples from male ApcMin/+ mice, consuming 3 probiotics, and these findings collectively suggest that depletion of probiotics and reduction of carcinogens in the male gut microbiota Enrichment resulted in male-biased CRC development .
In addition, accumulating evidence supports that lysophosphatidylcholine (LPC) can promote colorectal tumorigenesis, which is consistent with our finding that LPC promotes CRC cell proliferation and accelerates its cell cycle.
Collectively, our findings suggest that a male-biased gut microbiota can dysregulate gut metabolism, thereby increasing levels of oncogenic LPC, promoting cell proliferation, and compromising gut barrier function, ultimately leading to accelerated development of CRC .
Significance
Sexual dimorphism in colorectal tumorigenesis has been identified in multiple mouse models. Male and female mice exhibit different gut microbiota compositions.
Male mice showed marked enrichment of harmful bacteria and depletion of probiotics, which worsened intestinal barrier function and ultimately accelerated their CRC tumorigenesis and increased their mortality.
Therefore, modulation of sex-biased gut microbiota and metabolites may be a precise gender-targeted therapeutic strategy for the prevention and treatment of CRC .
References:
https://doi.org/10.1002/advs.202206238
Why are men more likely to get colorectal cancer?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.