Alzheimer’s Disease: Poor Metabolism Linked to Brain Damage
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Alzheimer’s Disease: Poor Metabolism Linked to Brain Damage
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Alzheimer’s Disease: Poor Metabolism Linked to Brain Damage
Analysis of Data from 176,000 Individuals Reveals a 12% Increase in Dementia Risk Associated with Metabolic Syndrome
Metabolic Syndrome (MetS), a collection of metabolic disorders primarily characterized by abdominal obesity, type 2 diabetes, high blood pressure, and abnormal lipid metabolism, has been found to be associated with a 12% increase in the risk of all-cause dementia, according to an analysis of data from 176,000 individuals.
MetS is a group of metabolic disorders with the aforementioned clinical features, and according to the 2023 Metabolic Syndrome Diagnosis and Treatment Guidelines, the prevalence of MetS in individuals aged 20 and older in China is as high as 31.1%.
Previous studies had suggested that MetS might be a new risk factor for dementia. However, due to limitations in sample size and follow-up time, the relationship between MetS and the risk of dementia has not been definitively established until now.
Recently, a team led by Danial Qureshi from the Nuffield Department of Population Health at the University of Oxford conducted a 15-year follow-up analysis of 176,000 non-dementia participants. They found a 12% increase in the risk of all-cause dementia associated with MetS.
Even when the researchers limited the follow-up time to 5-10 years and over 10 years, the correlation between MetS and the risk of all-cause dementia persisted (with hazard ratios of 1.17 and 1.22, respectively).
The study was published in Alzheimer’s & Dementia.
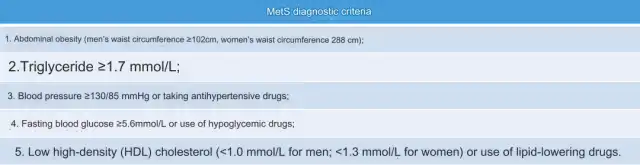
Let’s briefly review the diagnostic criteria for MetS. According to the International Diabetes Federation (IDF) and the American Heart Association (AHA) unified standards, a diagnosis of MetS is made if three or more of the following five criteria are met.
To address the limitation of small sample sizes in previous studies, the researchers selected 176,249 participants aged 60 and older without dementia from the UK Biobank, a large prospective cohort comprising over 500,000 participants aged 40-69 in the UK.
Baseline data showed that 41.7% of these participants had MetS. Among those with MetS, 52.8% met three MetS diagnostic criteria, 33.2% met four criteria, and 14.0% met all five criteria.
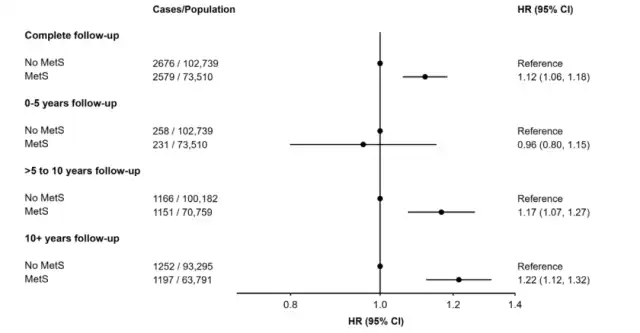
The results revealed that over 15 years of follow-up, there were a total of 5,255 cases of all-cause dementia. Participants with MetS had a 12% increased risk of dementia compared to those without MetS (with a hazard ratio of 1.12).
When the researchers conducted a stratified analysis based on follow-up time, the relationship between MetS and the risk of all-cause dementia remained significant for follow-up times of 5-10 years and over 10 years (with hazard ratios of 1.17 and 1.22, respectively).
However, for follow-up times less than 5 years, there was no correlation between MetS and the risk of all-cause dementia (with a hazard ratio of 0.96).
Prior research has shown that APOE4 is associated with an increased risk of dementia, particularly Alzheimer’s disease. Therefore, this study also examined the relationship between MetS, APOE4 carrier status, and the risk of dementia.
The results indicated that MetS was associated with an increased risk of dementia in individuals who did not carry APOE4 (with a hazard ratio of 1.26), but it was not associated with the risk of dementia in APOE4 carriers (with a hazard ratio of 1.02). This finding is consistent with previous research suggesting that MetS is related to cognitive decline in individuals without APOE4.
Finally, the researchers stratified participants based on the number of MetS diagnostic criteria met. The results showed that participants who met four or five MetS diagnostic criteria had a 19% and 50% higher risk of dementia, respectively, compared to those who did not meet any of the criteria (with hazard ratios of 1.19 and 1.50, respectively).
In summary, this study, utilizing a large sample size, discovered an association between MetS and an increased risk of all-cause dementia, with the strongest correlation observed in participants meeting four to five MetS diagnostic criteria.
However, the researchers also noted that the current findings are limited by the indications for MetS treatment, as some medications taken by MetS patients may be associated with a reduced risk of dementia. Further research is needed to explore the relationship between MetS and dementia risk.
Alzheimer’s Disease: Poor Metabolism Linked to Brain Damage
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



