Can Fungal Infections Lead to Alzheimer’s Disease-Like Changes in the Brain?
- EB Virus Could Be Infected by Kiss: A Hidden Threat Linked to Cancer
- The Silent Threat: How Gas Stoves Pollute Our Homes and Impact Health
- Paternal Microbiome Perturbations Impact Offspring Fitness
- New Report Casts Doubt on Maradona’s Cause of Death and Rocks Manslaughter Case
- Chinese academician unable to provide the exact source of liver transplants
- Early Biomarker for Multiple Sclerosis Development Identified Years in Advance
Can Fungal Infections Lead to Alzheimer’s Disease-Like Changes in the Brain?
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Can Fungal Infections Lead to Alzheimer’s Disease-Like Changes in the Brain?
An increasing body of research suggests that environmental fungi and endosymbiotic fungi within the body are key drivers of various chronic inflammatory conditions, including asthma, chronic sinusitis, chronic pulmonary aspergillosis, eczema, and more.
Candida albicans, a type of white yeast fungus, is one of the most common fungal pathogens, responsible for a variety of infections.
It’s noteworthy that up to 40% of the general population carries Candida albicans. What’s particularly significant is that this fungus can infect the brain, leading to fungal encephalitis.
Moreover, studies indicate a connection between fungal infections, such as Candida albicans, and chronic neurodegenerative diseases like Alzheimer’s disease. However, our understanding of how these common microorganisms contribute to the development of such diseases remains limited.
Recently, researchers from Baylor College of Medicine in the United States published a study in the Cell Reports subjournal titled “Toll-like receptor 4 and CD11b expressed on microglia coordinate eradication of Candida albicans cerebral mycosis” [1].
Previously, this research team discovered that the white yeast fungus can enter the brain through the bloodstream and induce changes akin to Alzheimer’s disease. In this study, they delved further into the mechanisms through which Candida albicans breaches the blood-brain barrier and causes Alzheimer’s disease-like alterations in the brain. They also unveiled the mechanisms by which microglial cells in the brain clear Candida albicans infections.
The David Corry Laboratory at Baylor College of Medicine has extensive experience in fungal research. In 2019, they published a paper in the Nature Communications journal, becoming the first to report that white yeast fungus can enter the brain and induce changes highly reminiscent of Alzheimer’s disease [2].
In this latest research published in Cell Reports, they have gone a step further to elucidate the molecular mechanisms.
The research team found that Candida albicans secretes aspartic proteinases (Sap), enzymes that can disrupt the blood-brain barrier, enabling the fungus to enter the brain and cause damage. However, in healthy mice, Candida albicans is completely eradicated from the brain after about ten days.
In this latest study, they discovered that the clearance of Candida albicans from the brain is primarily attributed to two mechanisms of microglial cells in the brain. Specifically, the aspartic proteinase (Sap) used by Candida albicans to break the blood-brain barrier also breaks down amyloid precursor protein (APP) into β-amyloid (Aβ) peptide, which activates microglial cells via Toll-like receptor 4 (TLR4). TLR4 can reduce the Candida albicans load in the brain but cannot clear the infection. Candida albicans also produces a protein called candidalysin, which binds to another receptor, CD11b, on microglial cells. Candidalysin-mediated activation of microglial cells is essential for clearing Candida albicans from the brain. Inhibiting this pathway hinders the effective clearance of Candida albicans from the brain.
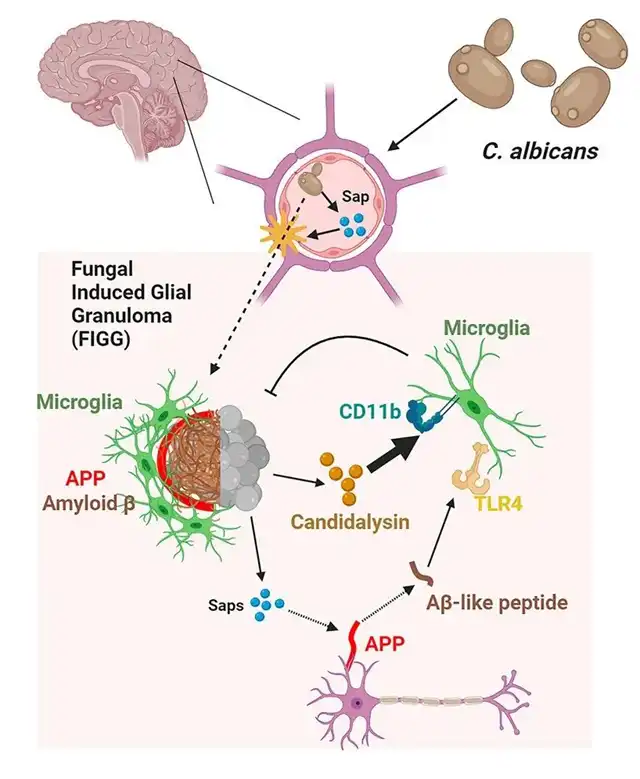
Professor David Corry, the corresponding author of the paper, suggests that this research could provide an essential piece of the puzzle in understanding Alzheimer’s disease. Current understanding posits that Alzheimer’s disease primarily results from the accumulation of toxic β-amyloid (Aβ) peptides in the brain, with the prevailing notion being that these Aβ-like peptides are endogenously produced by the brain through the cleavage of amyloid precursor protein (APP). However, this latest research hints at an alternate source for Aβ-like peptides, suggesting that commonly detected fungi in the brains of Alzheimer’s disease and other neurodegenerative disease patients, like Candida albicans, have their own set of proteinases that aid in breaching the blood-brain barrier, entering the brain, and triggering the production of Aβ-like peptides in the brain.
In summary, this study indicates that the aggregation of Aβ-like peptides in the brains of patients with neurodegenerative diseases like Alzheimer’s and Parkinson’s may result from a collaborative effort between the brain and Candida albicans. These findings support further research to assess the role of Candida albicans in the development of Alzheimer’s disease in humans, which could potentially lead to new treatment strategies.
Paper Links:
1. https://doi.org/10.1016/j.celrep.2023.113240
2. https://www.nature.com/articles/s41467-018-07991-4
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



