DNA Damage Repair Pathways and Drug Development
- Child Products from Aliexpess and Temu Contain Carcinogens 3026x Over Limit
- Daiichi Sankyo/AstraZeneca’s Enhertu Shows Positive Results in Phase III DESTINY-Breast06 Clinical Trial
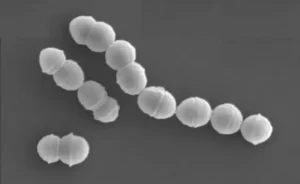
- Mn007 Molecules Offer Potential for Combating Streptococcus pyogenes Infection
- Popular Indian Spices Banned in Hong Kong Over Carcinogen Concerns
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Gut Bacteria Enzymes Offer Hope for ABO Universal Blood Transfusions
DNA Damage Repair Pathways and Drug Development
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
DNA Damage Repair Pathways and Drug Development
Over the past few decades, our understanding of DNA damage response (DDR) pathways has deepened, expanding the scope of oncology treatments.
It’s becoming increasingly clear that defects in DNA damage response leading to genomic instability in cells are a contributing factor to cancer.
On the other hand, these defects can also serve as therapeutic opportunities. An increasing number of DDR-targeting drugs have rapidly expanded to include inhibitors of multiple members involved in the DDR pathways, including PARP, ATM, ATR, CHK1, WEE1, and DNA-PK.
Currently, some of these DDR component inhibitors are in clinical trials.
Furthermore, new evidence suggests the sensitivity of DDR inhibitors to traditional cancer treatments and the correlation between DDR pathways and immune checkpoint inhibitor (ICI) response, all of which promote combination therapies based on DDR inhibitors.
Drugs targeting DNA repair pathways are increasingly playing a significant role in the field of cancer treatment.
DNA Damage and DNA Damage Response To maintain genomic integrity, complex DNA repair systems are used to combat various forms of DNA damage, collectively known as DNA damage response (DDR).
The DDR pathway consists of three functionally interwoven components: sensors that detect DNA damage, signal transducers that initiate signal cascades, and effectors that inhibit DNA repair.
These pathways are not mutually exclusive processes; instead, they work in coordination to form a precise regulatory network for DNA repair.

Base Excision Repair (BER) and Nucleotide Excision Repair (NER)
The genomes of all organisms undergo subtle changes due to various endogenous genotoxins, such as reactive oxygen species (ROS), ionizing radiation, and alkylating agents, leading to environmental damage. Most minor changes in DNA, such as single-strand breaks (SSBs), are repaired through the BER pathway.
BER is initiated by damaged bases, which are then excised, and replaced with newly synthesized DNA. The apurinic/apyrimidinic endonuclease (APE) cleaves at the AP site, creating a 3’OH end at the damage site. Finally, DNA polymerase and DNA ligase are recruited to close the gap created by the removal of the damaged base. BER is responsible for repairing minor damage, while larger double-strand breaks (DSBs) that distort the DNA helical structure require the NER pathway for repair. The NER mechanism involves a critical protein called excision repair cross-complementing protein 1 (ERCC1), which clears the DNA near the break and replaces it with normal DNA.
Homologous Recombination (HR) and Non-Homologous End Joining (NHEJ)
In mammalian cells, HR and NHEJ are the two major pathways for repairing DSBs. HR can repair DSBs during the S/G2 cell cycle phase because it uses sister chromatids as templates for new DNA synthesis, while NHEJ is active in all cell cycle phases except M.
HR analyzes homologous sequences from other parts of the genome, gathering information lost at the break site. HR begins by trimming the ends of the break, then forms Rad51 protein filaments with the help of Brca2, initiating the search for homologous sequences and facilitating the formation of a connection molecule between the broken DNA and the template, completing the repair.
NHEJ is simpler than HR; it directly rejoins the ends of the break. The essential factors required for NHEJ are an heterodimer composed of Ku70/Ku80 and the catalytic subunit of DNA-dependent protein kinase (DNA-PKcs), which recognizes DSBs and promotes downstream signaling factors for NHEJ, such as XRCC4, XLF, and DNA ligase IV. While NHEJ is considered simpler, it can sometimes lead to rearrangements, whereas HR is believed not to introduce errors.
Apart from HR and NHEJ, there is another DSB repair pathway with similar mechanisms to these two primary DSB repair pathways, but genetically distinct, known as alternative end joining (a-EJ) pathway. The a-EJ pathway can share a similar initiation process with HR and can also form DNA end-joining factors without a homologous template, similar to NHEJ. Increasing research is now focusing on the a-EJ pathway as a potential therapeutic target for cancer cells with impaired NHEJ or HR activity.
Mismatch Repair (MMR)
Apart from damage resulting from endogenous genotoxins, DNA damage can also arise from aberrant DNA processing. The DNA repair pathway for correcting replication-related errors is called MMR. During DNA synthesis, MMR corrects errors in nucleotide incorporation, preventing permanent DNA changes in dividing cells. Consequently, mutations or epigenetic silencing that leads to MMR defects can increase the spontaneous mutation rate, often associated with both hereditary and sporadic cancers.
Translesion Synthesis and Template Switching
DNA damage tolerance (DDT) is a fundamental bypass mechanism for repairing stalled DNA damage during replication, allowing DNA replication to proceed through obstructing lesions. Translesion synthesis (TLS) is one of two distinct modes of DDT, depending on the function of a specific TLS polymerase rather than the replicative DNA polymerase, allowing it to replicate directly across the damage site. Since TLS polymerases have limited proofreading activity, the TLS mechanism is error-prone, increasing the risk of mutations. Not surprisingly, TLS is a major source of cell mutations.
Conversely, the other mode of DDT, template switching (TS), involves recombining to homologous DNA templates in sister chromatids, similar to the HR process, which is considered more accurate than TLS. Repair activities of TLS and TS commence after the replication fork, indicating that they might occur during or after DNA replication. TS starts in early S-phase, while TLS begins in late S-phase.
Fanconi Anemia (FA) Pathway
Fanconi anemia is a rare genetic disorder caused by biallelic mutations in Fanconi genes, leading to deficient responses to DNA damage in affected patients. The Fanconi anemia pathway has been identified as a DNA repair pathway that can remove barriers inhibiting DNA replication and transcription, such as DNA interstrand crosslinks (ICL).
ICLs can form during various metabolic reactions (such as lipid peroxidation and ethanol metabolism) and chemotherapy (such as platinum-based therapies). While intrastrand crosslinks are repaired through the NER pathway, ICLs are primarily repaired through the FA pathway. After detecting ICLs through the UHRF1 protein and the FANCM-MHF1-MHF2 complex, the FA core complex is recruited to chromatin and monoubiquitinates substrates FANCI and FANCD2. Ubiquitinated FANCD2-I recruits various endonucleases, thus recognizing the DNA at the crosslink site and excising nucleotides to generate DNA substrates suitable for recombinational repair.

O6-Methylguanine-DNA Methyltransferase (MGMT) Pathway
It is well-known that DNA methylating agents can inhibit DNA methylation and produce a wide range of DNA adducts, such as O6-methylguanine (O6MeG) and O4-methylthymine, which can lead to base mispairing and subsequent point mutations. O6MeG, in particular, is considered a major source of methylation-induced DNA adducts, which can lead to mutations and carcinogenesis.
O6MeG can lead to the formation of G:C to A:T transition mutations, which are often observed in cancers. To mitigate the cytotoxic effects of O6MeG, MGMT, a DNA repair protein, transfers the methyl group to its catalytic cysteine, enabling the protein to bind and remove O6MeG from O6MeG:C base pairs, thus directly reversing DNA alkylation damage. In the absence of MGMT activity, O6MeG adducts mispair with thymine during DNA replication, resulting in a futile cycle of DNA repair. This ultimately leads to double-strand breaks, triggering cell death.
Therapeutic Potential of Targeting DDR Pathways Several components of the DDR pathways are being targeted for cancer treatment, either as monotherapies or in combination with other treatments. These include inhibitors of PARP, ATM, ATR, CHK1, WEE1, DNA-PK, and other key factors in DDR pathways. Understanding the DDR pathways’ intricacies can help identify the vulnerabilities of cancer cells and lead to the development of more effective targeted therapies.
-
PARP Inhibitors: Poly (ADP-ribose) polymerase (PARP) inhibitors, like olaparib, rucaparib, and niraparib, are particularly effective in treating cancers with defects in homologous recombination (HR), such as BRCA1/2 mutations. These inhibitors trap PARP enzymes at the DNA damage site, causing synthetic lethality in HR-deficient cells. This class of drugs is widely used in the treatment of ovarian and breast cancers.
-
ATM and ATR Inhibitors: Drugs targeting ATM (ataxia-telangiectasia mutated) and ATR (ataxia telangiectasia and Rad3-related) proteins have shown promise in clinical trials for various cancer types. ATM and ATR are involved in signaling DNA damage and regulating the cell cycle. Inhibitors of these proteins sensitize cancer cells to radiation and chemotherapy.
-
CHK1 and WEE1 Inhibitors: CHK1 and WEE1 are checkpoint kinases that regulate cell cycle progression in response to DNA damage. Inhibitors of CHK1 and WEE1 can abrogate cell cycle checkpoints, leading to genomic instability and cell death, especially in combination with other DNA-damaging therapies.
-
DNA-PK Inhibitors: DNA-dependent protein kinase (DNA-PK) is essential for NHEJ repair. Inhibitors of DNA-PK can sensitize cancer cells to radiation and chemotherapy, making them attractive candidates for combination therapies.
-
Fanconi Anemia Pathway Inhibitors: Targeting the Fanconi anemia pathway has shown promise for treating cancers with DNA interstrand crosslinks, which are otherwise resistant to standard chemotherapy. Drugs that inhibit the FA pathway can sensitize cancer cells to DNA crosslinking agents like cisplatin.
-
MGMT Inhibitors: The MGMT pathway is relevant in the context of DNA alkylation damage. Inhibiting MGMT can sensitize cancer cells to alkylating agents, increasing their effectiveness as chemotherapy drugs.
Clinical trials are ongoing to assess the safety and efficacy of these DDR-targeting drugs in different cancer types. In some cases, combinations of these inhibitors with traditional chemotherapy, radiation therapy, or immune checkpoint inhibitors (ICIs) are being explored to enhance therapeutic outcomes. Additionally, precision medicine approaches that involve identifying specific DDR pathway defects in individual patients are guiding the selection of the most suitable treatment strategies.
Conclusion:
The DNA damage response (DDR) pathways are essential for maintaining genomic integrity and preventing the accumulation of mutations that can lead to cancer.
Understanding these pathways and their various components has led to the development of targeted therapies that exploit DDR deficiencies in cancer cells.
Several DDR inhibitors, including PARP inhibitors, ATM and ATR inhibitors, CHK1 and WEE1 inhibitors, DNA-PK inhibitors, Fanconi anemia pathway inhibitors, and MGMT inhibitors, are under investigation in clinical trials.
These DDR-targeting drugs have shown promise in a range of cancer types, especially when used in combination with other treatments.
By exploiting the vulnerabilities of cancer cells, researchers and clinicians are working to improve the effectiveness of cancer therapy and provide more tailored treatment options for patients.
As our knowledge of DDR pathways and their role in cancer continues to evolve, we can expect further advancements in precision medicine and more effective cancer treatments.
DNA Damage Repair Pathways and Drug Development
Reference:
1. Targeting DNA repair pathway in cancer:Mechanisms and clinical application. MedComm (2020). 2021 Dec; 2(4):654–691.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.