Common local anesthetic lidocaine may have a resistance effect on head and neck cancer
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Common local anesthetic lidocaine may have a resistance effect on head and neck cancer
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Common local anesthetic lidocaine may have a resistance effect on head and neck cancer
A new study reveals how the commonly used local anesthetic lidocaine activates bitter taste receptors, thus exerting an anticancer effect on head and neck cancer.
Due to its low cost and ready availability, this drug is easily used in the treatment of these challenging cancer patients.
People who have undergone wound closure or dental procedures such as fillings may be familiar with lidocaine. While it is known how this local anesthetic works for pain relief, some believe that lidocaine also benefits cancer patients, although the mechanism is not fully understood.
Now, a study led by researchers from the University of Pennsylvania School of Medicine has unraveled the long-standing mystery of how lidocaine leads to the death of certain cancer cells.
The lead author of the study, Robert Lee, says, “We have been focusing on this research direction for many years, but surprisingly found that lidocaine targets a receptor, and this receptor happens to be highly expressed in various cancers.”
This ‘receptor’ is T2R14, a bitter taste receptor expressed in head and neck squamous cell carcinoma (HNSCC), a cancer with high mortality and a high incidence related to treatment. HNSCC occurs in the oral and nasal mucosa due to exposure to carcinogens and/or human papillomavirus (HPV).
In addition to playing a role in bitter taste perception, bitter taste receptors (T2Rs) are also involved in innate immunity, thyroid function, cardiac physiology, and other biological processes. Researchers studied T2Rs in ovarian cancer, breast cancer, and HNSCC, with a particular focus on T2R14.
Previous findings indicated the presence of T2Rs in many oral and throat cancers, triggering apoptosis or programmed cell death, and increased T2R expression was associated with improved survival rates in HNSCC patients. A study published earlier this year found that injecting lidocaine around tumors before surgery improves the survival rates of breast cancer patients.
“T2R14 is present in cells throughout the body. Incredibly, many existing drugs can activate it, so there may be more opportunities to consider redesigning other drugs to safely target this receptor.”
Researchers found that lidocaine activates the T2R14 receptor in HNSCC cell lines, leading to cancer cell apoptosis. Specifically, the activation of this drug results in mitochondrial calcium overload, mitochondrial membrane depolarization, and a significant decrease in the viability of HNSCC cells. It also induces the production of reactive oxygen species (ROS), further indicating mitochondrial dysfunction and cellular stress.
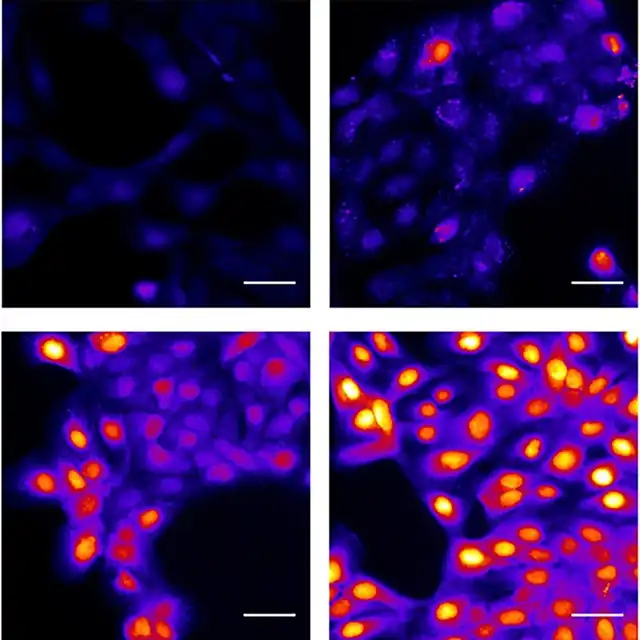
Calcium response of head and neck cancer cells to different concentrations of lidocaine Image/University of Pennsylvania School of Medicine
The research data also suggests that lidocaine inhibits proteasome degradation. The proteasome clears thousands of short-lived, damaged, misfolded, or obsolete proteins in cells. When proteasome activity is inhibited, proteins that need to be degraded accumulate, triggering apoptosis. When the inhibition of ROS generation or T2R14 signaling is reversed, lidocaine-induced proteasome inhibition is reversed, indicating that proteasome inhibition is caused by T2R stimulation, downstream mitochondrial dysfunction, and ROS.
It can be said that one advantage of HNSCC is that it is easily accessible to affected areas, so lidocaine can be applied in clinical practice as an injection or local anticancer therapy.
Co-lead author Ryan Carey says, “As a head and neck surgeon, we have been using lidocaine. We know lidocaine is safe, we are comfortable using it, and it is easily accessible, which means it can seamlessly integrate into other aspects of head and neck cancer care.”
The study also found that T2R14 is particularly high in HPV-related HNSCC, and HPV is currently the main form of HNSCC. We plan to conduct a clinical trial to test the effectiveness of adding lidocaine to standard treatment for HPV-related HNSCC.
Carey says, “While we are not saying lidocaine can cure cancer, it may gain an advantage in the treatment of head and neck cancer and move forward in improving treatment options for these challenging cancer patients, which is exciting for us.”
This research was published in the journal “Cell Reports.”
How does lidocaine affect cancer cells?
Common local anesthetic lidocaine may have a resistance effect on head and neck cancer
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



