Alarming Spread of ‘Super Fungus’ with a 60% Mortality Rate in China
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Alarming Spread of ‘Super Fungus’ with a 60% Mortality Rate in China
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Alarming Spread of ‘Super Fungus’ with a 60% Mortality Rate in China
On January 18, a prominent academic journal in infectious diseases, Emerging Microbes & Infections, published a study led by Professor Huang Guanghua from Fudan University’s School of Life Sciences and Professor Chu Haiqing from Tongji University Affiliated Shanghai Pulmonary Hospital [1].
The research reveals a growing and concerning trend of Candida auris, commonly known as the “super fungus” with a mortality rate of 60%, in China.
Between 2018 and 2023, there has been a significant increase in infections, with a staggering 450% year-on-year rise in cases in 2023 alone.
The resistance to common antifungal drugs has reached a high of 98.7%.
Hospitals across the country are facing an unprecedented challenge of drug-resistant fungi.
Rapid Surge in Cases Across 10 Provinces in China
Candida auris, a newly emerging fungus, has been causing severe diseases and spreading easily among patients in medical facilities. Since its first discovery in China in 2018 [2][3], Candida auris has now spread to ten provinces in the country.
The study examined 312 cases of Candida auris infections across 18 hospitals. The prevalence varied significantly between years, with the lowest cases recorded in 2020-2021 and a sudden surge to 182 cases in 2023, marking a 450% increase compared to 2022 (33 cases).
Taking a specific outbreak in Guangdong, China, as an example, 140 cases were detected, with 75% originating from the ICU. The infected individuals ranged from 3 to 91 years old, with a median age of 65. Nearly half of the cases (47.9%) involved individuals aged 65 and above, with risk factors including lung infections, hypertension, liver diseases, diabetes, and cancer.
Furthermore, the study found a close genetic relationship between Candida auris strains isolated in hospital environments and those found within patients. Out of 312 infections, 280 were linked to four cluster events in hospitals in Liaoning, Jiangsu, Anhui, and Guangdong.
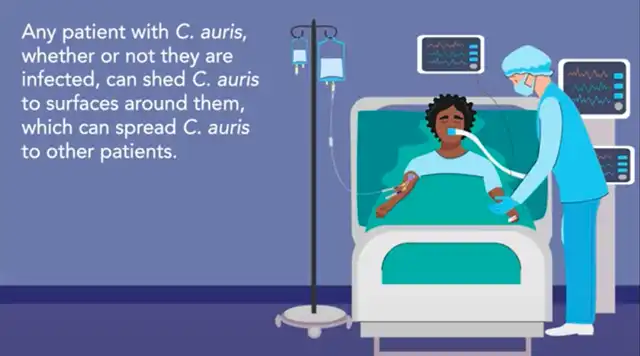
It suggests that Candida auris is spreading through hospital-acquired infections.
Notably, the isolated strains from these cases exhibited a high level of consistency in drug resistance. Up to 98.7% of strains showed high resistance to fluconazole, while 4.2% and 2.2% were resistant to amphotericin B and caspofungin, respectively.
Super Fungus in Nosocomial Settings
This is not the first time Candida auris has gained public attention. In 2009, a research team in Japan isolated the fungus from a patient’s external ear canal, but it did not draw widespread concern at that time. It wasn’t until 2016 that the Centers for Disease Control and Prevention (CDC) in the United States [5] and the Public Health England [6] issued warnings, bringing the fungus to international attention. As of now, the fungus has been reported in over 50 countries and regions [7].
Candida auris is known to cause candidemia, wound-related infections, and catheter-related infections. It can also infect the urinary tract, respiratory system, digestive system, and nervous system. The fungus can be isolated from hospital environments and patient skin, posing a significant threat.
On one hand, Candida auris mainly spreads in specialized environments such as hospitals, affecting immunocompromised individuals, with a mortality rate as high as 60% [10]. It can easily lead to nosocomial outbreaks, jeopardizing the safety of hospitalized patients and healthcare workers.
On the other hand, Candida auris naturally carries genes associated with resistance to antifungal drugs. Over 90% of clinically isolated strains are resistant to azole-class antifungal drugs [7]. This resistance makes infections difficult to treat, resulting in significantly higher treatment costs compared to other fungal infections.
In 2019, the United States Antibiotic Resistance Threats Report categorized microbial threats into four levels, designating Candida auris as an “urgent threat.” In 2020, the Clinical Microbiology Group of the Chinese Medical Association published an expert consensus on the diagnosis, treatment, and prevention of adult Candida auris infections, highlighting the fungus’s frequent multidrug resistance.
However, Candida auris is not invincible. According to the CDC’s 2018 treatment guidelines for Candida auris [12], echinocandin-class drugs are highly effective against most cases. Some refractory cases can be addressed through susceptibility testing to determine specific treatment methods [13].
Should the General Public Be Concerned?
Unlike many pathogens that public health authorities focus on, Candida auris is primarily an opportunistic infection in hospital settings. It tends to occur in individuals with underlying diseases, especially hospitalized patients, making it less likely for the general population to get infected.
The CDC has previously advised healthcare institutions that Candida auris typically infects patients through wounds, ventilators, and catheters, particularly in hospitalized and long-term care facility patients. Therefore, individuals not using catheters for an extended period and without severe immune deficiencies generally face minimal infection risks.
CDC related tips
However, healthcare institutions, especially infection control personnel and healthcare workers, need to take extra precautions.
Preventive measures against Candida auris infection include frequent environmental disinfection using effective disinfectants, minimizing the prophylactic use of antifungal drugs, and actively monitoring Candida auris infections when necessary [15], according to available data.
The CDC recommends special precautions for healthcare providers if a patient is infected, such as isolating the patient from high-risk groups, using special disinfectants to clean the room, wearing gloves, and protective clothing.
Alarming Spread of ‘Super Fungus’ with a 60% Mortality Rate in China
References:
[1]Bing J, Du H, Guo P, et al. Candida auris-associated hospitalizations and outbreaks, China, 2018-2023. Emerg Microbes Infect. 2024;13(1):2302843. doi: 10.1080/22221751.2024.2302843
[2]Wang X, Bing J, Zheng Q, et al. The first isolate of Candida auris in China: clinical and biological aspects. Emerg Microbes Infect. 2018;7(1):93. doi: 10.1038/s41426-018-0095-0
[3]Chen Y, Zhao J, Han L, et al. Emergency of fungemia cases caused by fluconazole-resistant Candida auris in Beijing, China. J Infect. 2018;77(6):561-571. doi: 10.1016/j.jinf.2018.09.002
[4]Satoh K, Makimura K, Hasumi Y, et al. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53(1):41-4. doi: 10.1111/j.1348-0421.2008.00083.x
[5]Centers for Disease Control and Prevention. Clinical Alert to U.S. Healthcare Facilities – Global Emergence of Invasive Infections Caused by the Multidrug-Resistant Yeast Candida auris. https://www.cdc.gov/fungal/diseases/candidiasis/candida-auris-alert.html
[6]Public Health England. Candida auris identified in England. https://www.gov.uk/government/publications/candida-auris-emergence-in-england/candida-auris-identified-in-england
[7]Chowdhary A, Jain K, Chauhan N. Candida auris Genetics and Emergence. Annu Rev Microbiol. 2023;77:583-602. doi: 10.1146/annurev-micro-032521-015858
[8]Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016-May 2017. MMWR Morb Mortal Wkly Rep. 2017;66(19):514-515. doi: 10.15585/mmwr.mm6619a7
[9]Eyre DW, Sheppard AE, Madder H, et al. A Candida auris Outbreak and Its Control in an Intensive Care Setting. N Engl J Med. 2018;379(14):1322-1331
[10]Boutin CA, Luong ML. Update on therapeutic approaches for invasive fungal infections in adults. Ther Adv Infect Dis. 2024 Jan 20;11:20499361231224980. doi: 10.1177/20499361231224980. PMID: 38249542; PMCID: PMC10799587.[11]Tsay S, Kallen A, Jackson BR, et al. Approach to the Investigation and Management of Patients With Candida auris, an Emerging Multidrug-Resistant Yeast. Clin Infect Dis. 2018;66(2):306-311. doi: 10.1093/cid/cix744
[13]Centers for Disease Control and Prevention. Recommendations for treatment of Candida auris. https://www.cdc.gov/fungal/diseases/candidiasis/c-auris-treatment.html
[14]Centers for Disease Control and Prevention. Recommendations for identification of Candida auris. https://www.cdc.gov/fungal/diseases/candidiasis/recommendations.html
[15]Lamoth F, Kontoyiannis DP. The Candida auris Alert: Facts and Perspectives. J Infect Dis. 2018;217(4):516-520. doi: 10.1093/infdis/jix597
[16]Karmarkar EN, O’Donnell K, Prestel C, et al. Rapid Assessment and Containment of Candida auris Transmission in Postacute Care Settings-Orange County, California, 2019. Ann Intern Med. 2021;174(11):1554-1562. doi: 10.7326/M21-2013
[17]Centers for Disease Control and Prevention. Candida auris – Information for Laboratorians and Health Professionals. https://www.cdc.gov/fungal/candida-auris/health-professionals.html
[18] Clinical Microbiology Group of the Laboratory Medicine Branch of the Chinese Medical Association. Expert consensus on the diagnosis, treatment, prevention and control of Candida auris infection in adults. Journal of Clinical Laboratory Medicine, 2020, 38(8):564-570.
[19]Brown GD, Denning DW, Gow NA, et al. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13. doi: 10.1126/scitranslmed.3004404
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



