The Dynamic Role of Platelets in Cancer Progression
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
The Dynamic Role of Platelets in Cancer Progression
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What Is The Dynamic Role of Platelets in Cancer Progression?
Platelets are the second most abundant blood cell type after red blood cells.
They are short-lived cell fragments shed from mature megakaryocytes, with a lifespan of 7-10 days.
Platelets are primarily known for their crucial roles in hemostasis and pathological thrombus formation. However, platelets also play key roles in other pathophysiological processes, including inflammation, tissue repair, and tumor growth and metastasis.
In recent years, platelets have been shown to interact dynamically with tumors to promote cancer cell survival and proliferation.
Thrombocytosis was first observed in malignant tumor patients in 1964. Since then, increasing clinical evidence has indicated a close relationship between elevated platelet counts in cancer patients and poor prognosis.
Many preclinical studies have further revealed direct and indirect crosstalk between platelets and tumor cells, which sustains tumor cell proliferation, metastasis, immune escape, and chemoresistance.
For example, platelets can bind to the surface of tumor cells to form microaggregates, establishing a physical barrier that protects tumor cells from immune cell attacks.
Platelets also release active soluble factors, such as TGF-β and platelet factor 4 (PF4), to promote tumor cell invasion and metastasis.
This intercellular communication, in turn, stimulates tumor cells to secrete various cytokines, such as IL-6 and CCL5, to induce additional platelet production and secretion of factors that promote angiogenesis, metastasis, and tumor cell proliferation.
Therefore, a deeper understanding of the molecular mechanisms and dynamic roles of platelets in tumor progression and metastasis is crucial for developing their applications in diagnosis, prognosis, monitoring treatment responses, and developing precise antiplatelet strategies for safe and effective clinical cancer treatment.
Regulatory Role of Tumor Cells on Platelets
The incidence of thrombocytosis is higher in patients with hematogenous metastasis and recurrence of ovarian, lung, and gastric cancers, especially in stage IV ovarian cancer, where the incidence of thrombocytosis can be as high as 65%. This suggests that an increase in platelet count may be a predictive factor for certain cancers and a method for monitoring tumor progression.
In ovarian cancer, tumor-induced thrombocytosis is mainly attributed to the production of IL-6 by tumor cells, which is released into the blood, stimulating the production of thrombopoietin (TPO) in the liver. Subsequently, TPO binds to the TPO receptor c-Mpl present on megakaryocytes to stimulate their growth and maturation in the bone marrow. Mature megakaryocytes then form proplatelets that extend and eventually bud off to form platelets. Besides IL-6, tumor cells and stromal cells also secrete granulocyte-macrophage colony-stimulating factor (GM-CSF), CCL5, and PF4 into the tumor microenvironment, stimulating platelet production.
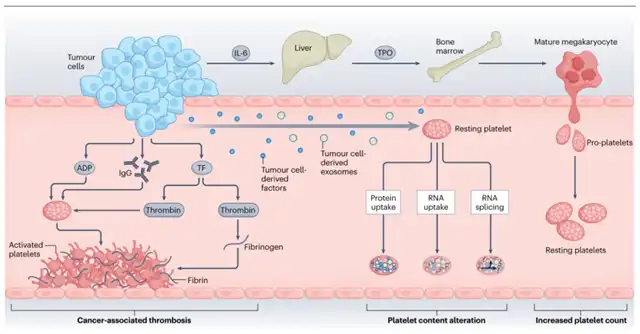
Studies have shown that the factors secreted by tumor cells, such as adenosine diphosphate (ADP) and IgG, or functional proteins and RNA, can lead to significant changes in the platelet proteome and transcriptome characteristics, increasing platelet procoagulant, proangiogenic, and prometastatic properties. Platelets in circulation can also actively absorb tumor-derived proteins and mRNA, leading to increased levels of platelet-derived growth factor (PDGF), TGF-β, and matrix metalloproteinase 1 (MMP1) in platelets.
Changes in platelet content and structure can induce platelet overactivation or activation. Platelet aggregation studies have shown that platelets from patients with metastatic ovarian, pancreatic, and breast cancers have significantly higher aggregation rates in response to agonists such as ADP, adrenaline, and collagen compared to platelets from healthy donors. Importantly, platelet activation can lead to cancer-associated thrombosis, which, if untreated, can lead to thromboembolic death in patients. However, despite significant progress in understanding the interaction between platelets and tumor cells, little is known about the molecular mechanisms by which platelets respond to tumor signals to alter their activity or behavior.
Direct Effects of Platelets on Tumor Cells
Direct contact between platelets and tumor cells triggers platelet activation and the formation of microaggregates around the surface of tumor cells, which protects them from immune recognition. Recent studies have shown that cancer cells in contact with platelets can engulf entire platelets through either membrane fusion-dependent or dynamic-dependent phagocytosis. Platelet adhesion receptor CD42a can recirculate to the cell membrane of A549 cells, which may help cancer cells adhere to the vascular wall in metastatic lesions.
Furthermore, in circulating prostate cancer cells isolated from patients, their absorption of platelets leads to the transfer of lipids, RNA, and proteins from platelets to cancer cells, enhancing their stemness and proliferative capabilities. These findings suggest that tumor cells can evade the immune system and enhance their proliferation and metastatic abilities by absorbing, presenting, or utilizing platelet-derived lipids, nucleic acids, and proteins.
Platelets Support the Tumor Microenvironment
Platelets can also release many pro-survival, pro-angiogenic, and immune-modulating factors in a non-contact manner to construct and maintain the primary and metastatic tumor microenvironments.
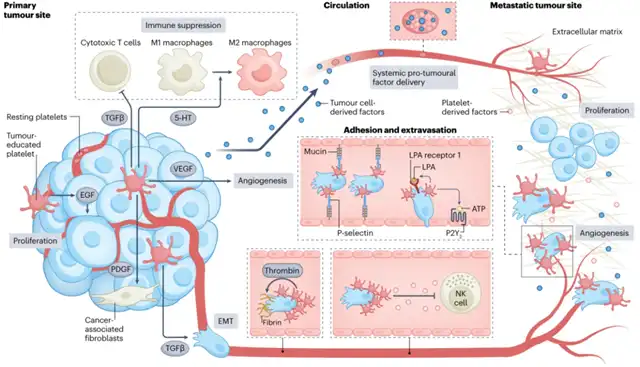
In primary tumors, platelets maintain tumor cell proliferation by secreting epidermal growth factor (EGF). Additionally, platelet-derived TGF-β and serotonin (5-HT) promote immune-suppressive microenvironments by inhibiting T cell function and promoting the M1-to-M2 phenotype transition of macrophages. Platelets also promote angiogenesis by secreting vascular endothelial growth factor (VEGF) and promote epithelial-mesenchymal transition (EMT) in tumor cells by secreting TGF-β. Platelet-derived growth factor (PDGF) can recruit cancer-associated fibroblasts, leading to excessive extracellular matrix deposition, which hinders immune cell infiltration into tumors.
In circulation, platelet microaggregates can cover circulating tumor cells (CTCs) to protect them from shear stress and immune surveillance. During the formation of platelet microaggregates induced by tumor cells, the production of thrombin induces the formation of a fibrin network, stabilizing the binding of platelet microaggregates to CTC surfaces. Additionally, the shedding of integrin metalloproteinase 10 (ADAM10) and ADAM17 from platelets, as well as the secretion of TGF-β, inhibit the activity of natural killer (NK) cells.
In distant organ sites, platelets promote the adhesion of tumor cells to endothelial cells and contribute to the formation of solid metastatic foci by facilitating transendothelial migration. Surface adhesion molecules on platelets in microaggregates, such as P-selectin, can bind to von Willebrand factor (vWF) present on endothelial cells, promoting the arrest of tumor cells at the endothelium. Adenosine triphosphate (ATP) released from platelets then interacts with P2Y2 receptors on endothelial cells to increase endothelial gaps, facilitating the extravasation of CTCs. Meanwhile, platelet-secreted lysophosphatidic acid (LPA) can bind to LPA receptor 1 on tumor cells, enhancing their invasive capacity. Additionally, circulating platelets can absorb tumor-derived
TGF-β, PDGF, and VEGF, and release them locally to promote the survival, proliferation, and angiogenesis of metastatic foci.
Conclusion
In summary, platelets play a crucial role in cancer progression and metastasis by interacting with tumor cells in various ways.
They directly protect tumor cells from immune surveillance, promote tumor cell survival and proliferation, enhance metastatic potential, and modulate the tumor microenvironment to favor cancer progression.
Understanding the complex interactions between platelets and tumors can provide valuable insights into the development of new therapeutic strategies for cancer treatment. Targeting platelet-tumor interactions could potentially improve the efficacy of existing cancer therapies and reduce the risk of metastasis and cancer-associated thrombosis.
What Is The Dynamic Role of Platelets in Cancer Progression?
Reference:
1.The dynamic role of platelets in cancer progression and their therapeutic implications. Nat Rev Cancer.2023 Dec 1.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



