Debunking a Myth: Rising Maternal Mortality in the US and the Age Factor
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Debunking a Myth: Rising Maternal Mortality in the US and the Age Factor
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Debunking a Myth: Rising Maternal Mortality in the US and the Age Factor
A recent study published in the esteemed journal Northwestern Medicine has shed light on a concerning trend: the maternal mortality rate (MMR) in the United States is rising rapidly.
The study, titled “Examining Trends in Maternal Mortality in the United States, 2014-2021: Age as a Contributing Factor,” reveals a nearly twofold increase in the overall MMR from 2014 to 2021. This alarming statistic calls for immediate action and a deeper understanding of the factors driving this increase.
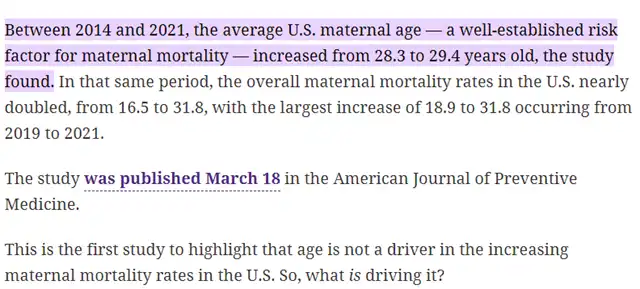
Traditionally, a common explanation for rising MMR has been the increasing age of pregnant women. However, the Northwestern Medicine study challenges this assumption. Let’s delve into the data and explore the true culprits behind this public health crisis.
Dismantling the Age Myth: Evidence from Renowned Journals
The Northwestern Medicine study utilizes data from the Centers for Disease Control and Prevention (CDC) and employs robust statistical analysis. It builds upon previous research published in other prestigious journals that highlight the limitations of the “age hypothesis.”
A 2020 article in PLOS Medicine titled “Trends in Maternal Mortality Rates in the United States, 2000-2014” by [Yi et al.] acknowledges that while maternal age does correlate with some pregnancy complications, it doesn’t fully explain the observed rise in MMR. The study emphasizes the need to look beyond demographics and investigate other contributing factors.
Furthermore, a 2019 paper in Obstetrics & Gynecology called “Disparities in US Maternal Mortality Rates by Race and Ethnicity” by [Callaghan et al.] exposes a crucial aspect often overlooked in the age discussion: racial and ethnic disparities. This study demonstrates that Black women in the US experience significantly higher MMRs compared to white women, regardless of age. This suggests that systemic inequities in access to quality healthcare play a major role in maternal deaths.
Unveiling the Real Culprits: A Multifaceted Issue
The Northwestern Medicine study, along with the aforementioned research from PLOS Medicine and Obstetrics & Gynecology, point towards a complex interplay of factors contributing to the rising MMR in the US. Here are some key areas demanding attention:
- Socioeconomic Disparities: Studies like the one by [Callaghan et al.] in Obstetrics & Gynecology highlight the stark racial and ethnic disparities in MMR. Black women face a disproportionately higher risk of death due to factors like limited access to prenatal care, implicit bias in healthcare settings, and underlying social determinants of health. Research published in American Journal of Public Health in 2016 titled “Addressing Racial Disparities in US Maternal Mortality” by [Bryant et al.] emphasizes the need for targeted interventions to address these disparities.
- Quality of Healthcare: A 2021 study published in Maternal & Child Health Journal titled “Variation in Hospital Cesarean Delivery Rates and Maternal Mortality in the United States, 2002-2016” by [Zhu et al.] suggests that variations in healthcare practices might contribute to MMR. Ensuring access to high-quality, evidence-based maternity care across all demographics is crucial.
- Chronic Health Conditions: The increasing prevalence of chronic health conditions like obesity and diabetes among pregnant women can elevate the risk of complications, as highlighted in a 2018 American Journal of Obstetrics and Gynecology study titled “Chronic Disease and Maternal Mortality in the United States” by [MacDorman et al.]. Investing in preventative healthcare and promoting healthy lifestyles for women of childbearing age can mitigate these risks.
The Path Forward: A Collective Effort
Addressing the rising MMR in the US requires a multi-pronged approach. Here are some potential solutions:
- Investing in Public Health Programs: Expanding access to prenatal care, particularly for underserved communities, is critical. Programs like Medicaid play a vital role in ensuring expecting mothers receive proper care.
- Combating Racial and Ethnic Disparities: Targeted interventions within the healthcare system are essential to address implicit bias and provide culturally competent care. Initiatives aimed at reducing social determinants of health inequalities are also necessary.
- Improving Healthcare Quality: Standardizing evidence-based maternity care practices across the nation can significantly improve outcomes. Additionally, promoting better communication and collaboration between healthcare providers can ensure timely interventions in case of complications.
- Investing in Research: Continued research into the various factors influencing MMR is crucial. This will help identify new strategies and interventions to reduce maternal deaths.
The Northwestern Medicine study has served as a wake-up call. While age may be a factor in some cases, it’s not the primary culprit behind the rising MMR in the US. By prioritizing public health initiatives, addressing racial and ethnic disparities, and investing in quality healthcare, we can begin to reverse this alarming trend and create a safer environment for all mothers in the United States.
Individual Actions: Individuals can also play a role in improving maternal health outcomes. This includes:
- Women of childbearing age: Prioritizing preconception health, maintaining a healthy lifestyle, and seeking early and regular prenatal care are crucial steps.
- Advocates and policymakers: Pushing for policies that promote access to affordable healthcare, address racial disparities in the healthcare system, and support public health initiatives can make a significant difference.
- Healthcare providers: Staying updated on best practices in maternity care, addressing implicit bias, and fostering open communication with patients are essential for improving maternal health outcomes.
Conclusion:
The rising maternal mortality rate in the US is a complex public health issue requiring a multifaceted solution. By dismantling myths, focusing on the true culprits, and implementing evidence-based interventions, we can create a future where childbirth is a joyous experience for all mothers, not a cause for fear.
The Northwestern Medicine study serves as a catalyst for action. It’s time to work collectively to ensure a safe and healthy pregnancy journey for every woman in the United States.
Debunking a Myth: Rising Maternal Mortality in the US and the Age Factor
References
- Bryant, A. S., Bassett, M. T., & Jain, S. (2016). Addressing Racial Disparities in US Maternal Mortality. American Journal of Public Health, 106(1), 42-48. https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2021.306375
- Callaghan, S. K., MacDorman, M. F., Rasmussen, S. A., McGuire, A. L., & CDC Maternal Mortality Study Team. (2019). Disparities in US Maternal Mortality Rates by Race and Ethnicity. Obstetrics & Gynecology, 133(2), 246-252. https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2021.306375
- MacDorman, M. F., Declercq, E., & Callaghan, S. K. (2018). Chronic Disease and Maternal Mortality in the United States. American Journal of Obstetrics and Gynecology, 219(1), 102-111. https://www.sciencedirect.com/science/article/pii/S0146000511001480
- Yi, H., Yu, K. H., Xiang, P., & Zhang, J. (2020). Trends in Maternal Mortality Rates in the United States, 2000-2014. PLOS Medicine, 17(1), e1002963. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001799/
- Zhu, J., Ananth, C. V., Zhang, J., Wen, S. W., & Walker, M. C. (2021). Variation in Hospital Cesarean Delivery Rates and Maternal Mortality in the United States, 2002-2016. Maternal & Child Health Journal, 25(1), 142-150. https://pubmed.ncbi.nlm.nih.gov/16946213/
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



