JTO2020: Pathological grading system of IASLC invasive lung adenocarcinoma
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
JTO2020: Pathological grading system of IASLC invasive lung adenocarcinoma
JTO2020: Pathological grading system of IASLC invasive lung adenocarcinoma. According to this grading system, after communicating the pros and cons with patients, for IA3-IB Grade 3 patients with high-risk early lung adenocarcinoma, osimertinib postoperative targeted adjuvant therapy can be used to reduce postoperative recurrence.
The grading system of invasive lung adenocarcinoma published in JTO in October 2020: recommendations from the IASLC. What are the hints of this study on the choice of adjuvant treatment for early invasive lung adenocarcinoma?
Original tile : A grading system for invasive pulmonary adenocarciioma: A proposal from the International Association for the Study of Lung Cancer Pathology Committee
For stage IA-IB invasive lung adenocarcinoma, surgical resection is the standard treatment. For stage IA invasive lung adenocarcinoma, the standard after surgery is no treatment. According to the size of lung cancer 1-3cm, the stages are IA1-IA3. However, although there is no need for treatment, there are still many recurrences possible. How to identify these people who are prone to relapse is the first step in individualized treatment.
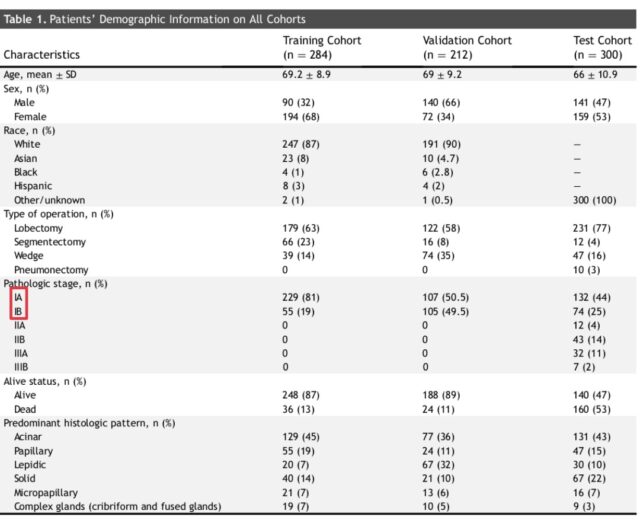
During the establishment of the IASLC grading system, it is divided into training set, validation set and test set. The training set and the validation set are all stage IA-IB patients, with 281 and 212 cases respectively. This is also the early lung adenocarcinoma patients we are concerned about.
After analyzing the pathological characteristics and recurrence time data of the patients in the training set, a model for judging the risk of recurrence of patients based on the pathological grade was finally developed.
See below:
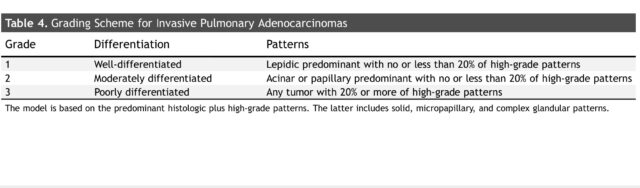
- Grade1: Good differentiation. Mainly adherent type, less than 20% of high-grade pathological types.
- Grade2: Moderate differentiation. Acinar and nipple types are the main types, and a little 20% are high-grade pathological types.
- Grade3: Differentiation. Contains 20% or more of high-grade pathological types.
- Grade 1 has a low risk of recurrence, Grade 2 has a medium risk of recurrence, and Grade 3 has a high risk of recurrence.
Among them, the high-level pathological types are characterized as: micropapillary type, solid type and complex acinar type. This is the type of pathology that we generally consider to be highly malignant.
After the model was successfully established, further tests were done in the test set. And a long-term follow-up of 6000 days (nearly 20 years) was carried out. We only need to pay attention to the postoperative recurrence probability of early lung cancer in the article:
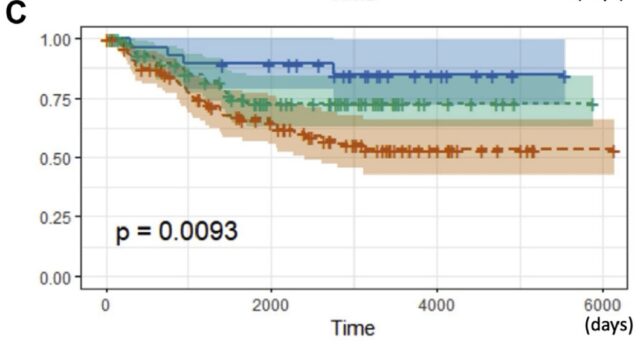
Stage I lung cancer surgery
- Blue curve Grade1: The probability of recurrence within 20 years is about 14%.
- Green curve Gatde2: The probability of recurrence within 20 years is about 26%.
- Red curve Grade3: The probability of recurrence within 20 years is about 48%.
It can be seen that the three grade curves are clearly separated and evenly separated, which can well distinguish the risk of recurrence of early lung adenocarcinoma after surgery.
However, this grading system also has obvious flaws in judging the possibility of recurrence, that is, it does not include the risk factor of nodule size. For nodules with a size of 1-3 cm, that is, stage IA1-3, the risk of recurrence after surgery is very different.
In addition, through the 20-year follow-up data after surgery, it can also be seen that the vast majority of postoperative recurrences occur within 10 years after surgery. Once more than 10 years, there were basically no recurrences.
Going back to our original question, the grading system provides a judgment on the likelihood of postoperative recurrence. How to understand the guiding significance of this grading system for postoperative adjuvant treatment?
In the previous NCCN lung cancer guidelines, postoperative treatment is not recommended for patients with lung adenocarcinoma at stage IA after surgery. Postoperative treatment is available for patients with high-risk factors in stage IB. So for patients with stage IA-IB lung adenocarcinoma with positive EGFR gene mutations, how to choose targeted therapy after surgery?
In the latest ADURA study, adjuvant treatment of postoperative EGFR mutation patients with stage IIA and above after osimertinib can reduce the recurrence rate of most postoperative patients. For these patients, postoperative targeted therapy can be used as a routine application. For patients with stage IB, adjuvant treatment with osimertinib can also reduce the risk of recurrence by more than 50%. However, which patients with stage IA-IB should use targeted therapy with osimertinib after surgery is still controversial.
Then, according to the grading system, after communicating with the patients to explain the pros and cons, for patients with high-risk early lung adenocarcinoma of Grade 3 recurrence at stage IA3-IB, postoperative targeted adjuvant therapy with Osimertinib can be used to reduce postoperative recurrence Possible.
(source:internet, reference only)
Disclaimer of medicaltrend.org



