Innate lymphocytes (ILCs)
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Innate lymphocytes (ILCs)
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- What is the difference between Atorvastatin and Rosuvastatin?
- How long can the patient live after heart stent surgery?
Innate lymphoid cells (ILCs) are also lymphocytes, but lack adaptive antigen receptors, so they belong to innate lymphocytes, including: ILC1s, ILC2s, ILC3s, NK, LTi.
Most of them reside in the organization and are closely related to the fibers of the organization.
ILCs development
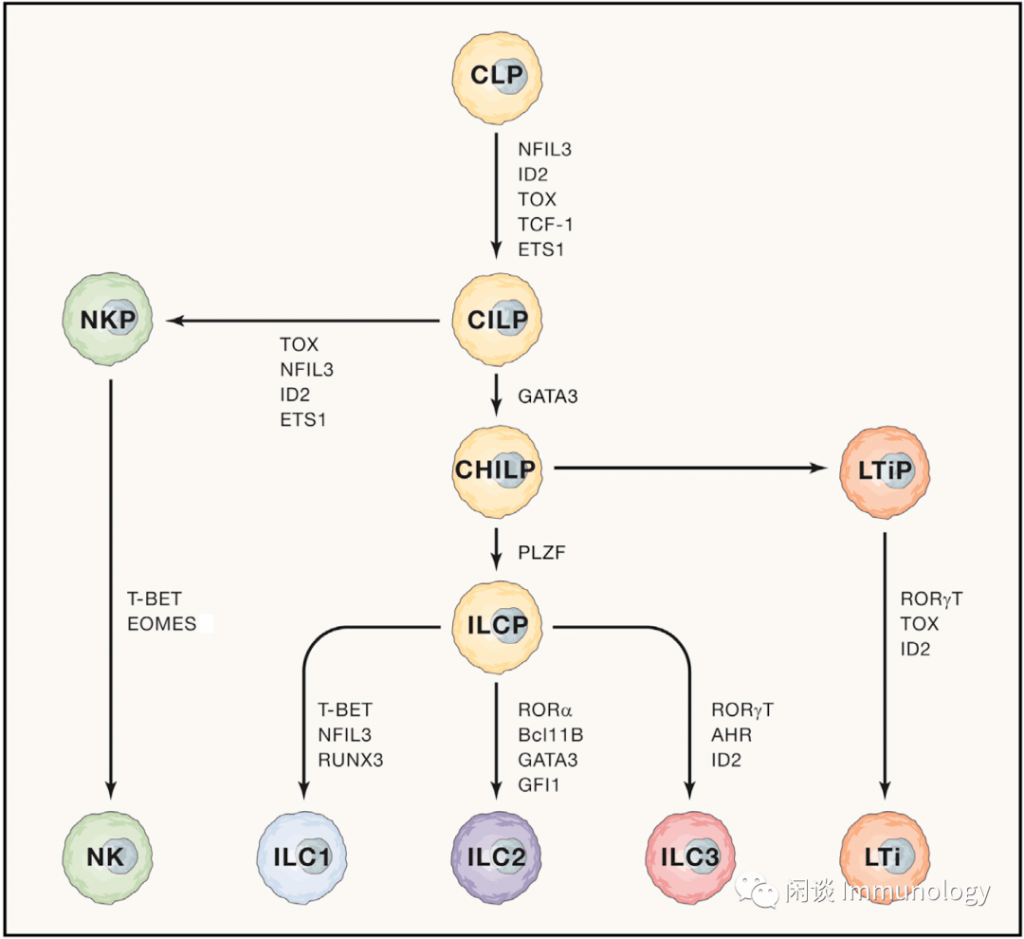
Like the development of T and B cells, ILCs originated from common lymphoid progenitors (CLP), and when they arrived at common innate lymphoid progenitors (CILP), they began the development process of innate lymphoid cells.
NK cell progenitor cells (NKP) then differentiate into NK cells
Common helper innate lymphoid progenitors (CHILP), and then differentiate into two:
- 1) Innate lymphocyte progenitor cells, and then differentiate into ILC1, ILC2, ILC3
- 2) Lymphoid tissue inducer progenitors (LTiP), differentiate into LTi (LTi is an important cell in the formation of lymph nodes, refer to reading: The architect of lymph nodes: Lymph node stromal cells)
ILCs immune function
In 2013, Hergen Spits et al. wrote an article to standardize the classification and characterization of innate lymphocytes that were confusing at that time, forming the current universal naming rule (Reference 2).
- NK cells and ILC1 belong to Group1, secrete typical cytokines IFN-γ, etc., and functionally respond to intracellular pathogens (viruses and tumors);
- ILC2 cells belong to Group2 and secrete typical cytokines IL-4, IL-5, IL-13, etc., and functionally respond to large extracellular pathogenic parasites and allergens;
- ILC3 and LTi belong to Group3, secrete typical cytokines IL-17, IL-22, etc., and develop an immune response to extracellular microorganisms (bacteria, fungi). LTi is mainly involved in the formation of stimulated lymph nodes.
Non-immune function
Metabolism
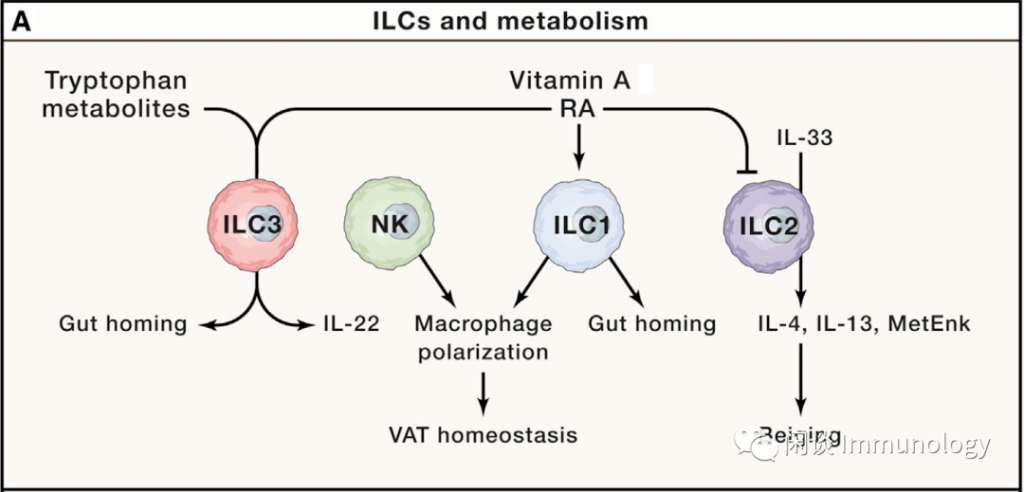
- Many different types of immune cells reside in adipose tissue, and ILC2 is the most important function among ILCs.
- ILC2 plays a role in maintaining metabolic homeostasis in individuals. If dysfunction occurs, it will cause Th1 inflammation and obesity. ILC2 resides in visceral adipose tissue and is maintained by IL-33.
- ILC2 secretes IL-5 to maintain eosinophils, and secretes IL-13 to promote the polarization of macrophages to M2, and regulate fat metabolism and insulin resistance.
- In the visceral adipose tissue, heterogeneous ILC1 and NK cells were also found with inconsistent functions.
Tissue remodeling and repair
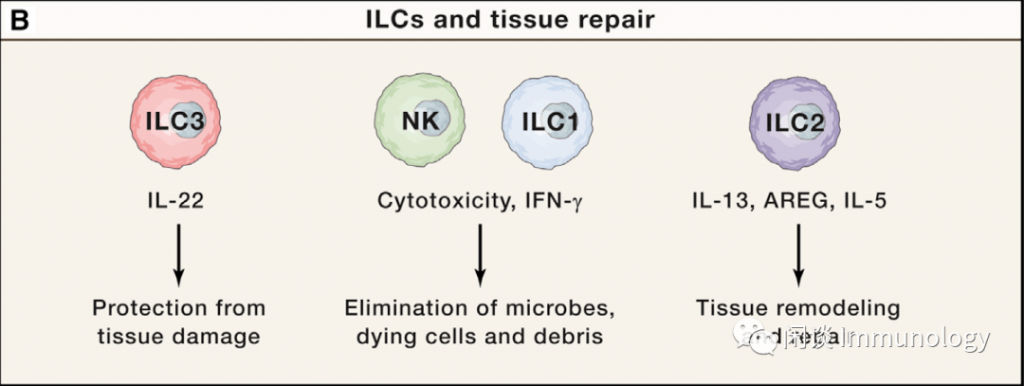
- IL-22 is secreted by ILC3 to induce epithelial cells to express antimicrobial peptides and protect the injured site from bacterial infection.
- ILC1 and NK cells, which are cytotoxic lymphocytes, secrete IFN-γ to protect against infection by pathogenic microorganisms, and digest dead cells and debris to facilitate tissue regeneration.
- ILC2s plays a prominent role in tissue repair and remodeling. Th2 type cellular immunity mediates the elimination of large microorganisms such as worms and allergic pathogens. For example, in the intestine, worm infection will stimulate the intestinal cluster cells and brush cells to secrete IL-25. IL-25 activates ILC2s and then secretes IL-13. IL-13 can drive epithelial cells to differentiate into secretory cells to form positive Feedback, promote tissue remodeling, and expel large pathogens. Immune activation to eliminate pathogens, but also accompanied by tissue damage.ILC2s limits the expansion of tissue damage. The mechanisms include: secretion of AREG, combined with its receptor EGFR, promote epithelial cell differentiation and repair damaged areas; secretion of AREG and IL-13, promote fibrosis response, including myofibroblast differentiation, proliferation, cell Outer matrix deposition, etc.; ILC2s is an important source of early IL-5, IL-5 recruits and activates eosinophils, IL-4 secreted by eosinophils, promotes the proliferation of fibroadipocyte progenitor cells, and prevents their differentiation into adipocytes , Differentiate into fibroblasts after injury.
ILC2s plays a prominent role in tissue repair and remodeling. Th2 type cellular immunity mediates the elimination of large microorganisms such as worms and allergic pathogens. For example, in the intestine, worm infection will stimulate the intestinal cluster cells and brush cells to secrete IL-25. IL-25 activates ILC2s and then secretes IL-13. IL-13 can drive epithelial cells to differentiate into secretory cells to form positive Feedback, promote tissue remodeling, and expel large pathogens.
Immune activation to eliminate pathogens, but also accompanied by tissue damage. ILC2s limit the expansion of tissue damage, the mechanisms include:
Secrete AREG, combine with its receptor EGFR, promote epithelial cell differentiation and repair damaged areas;
Secret AREG and IL-13 to promote fibrosis, including myofibroblast differentiation, proliferation, and extracellular matrix deposition;
ILC2s is an important source of early IL-5. IL-5 recruits and activates eosinophils, IL-4 secreted by eosinophils, promotes the proliferation of fibroadipocyte progenitor cells, prevents their differentiation into adipocytes, and after injury occurs Fibroblast differentiation.
Nervous system regulates ILCs function
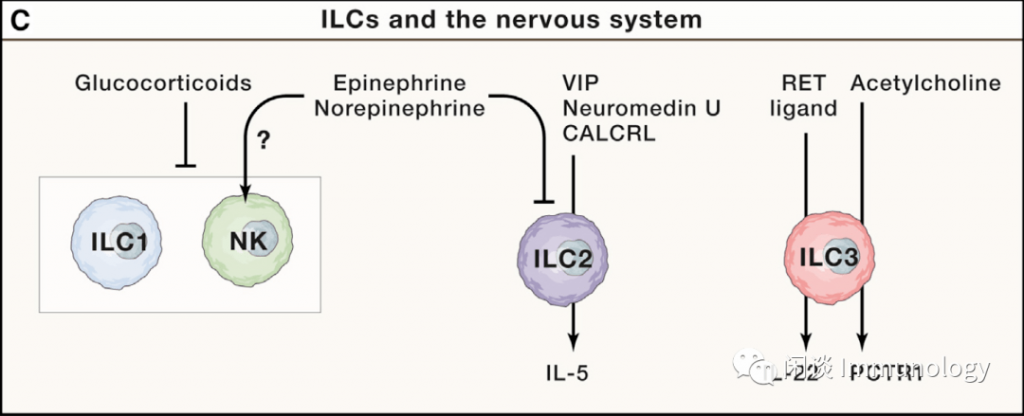 Picture from literature 1
Picture from literature 1
The nervous system is keenly aware of changes in the body’s environment. When the immune response/inflammatory response to pathogenic microorganisms or injury is excessive, the body releases glucocorticoids through the hypothalamic-pituitary-adrenal axis. ILC1 and NK cells express glucocorticoid receptors.
After binding to glucocorticoids, NK cells produce IFN-γ in the spleen and liver, and the ability of ILC1 to produce IFN-γ in the liver is weakened. IFN-γ is septic shock caused by endotoxin Important factor.
Neuropeptides and neurotransmitters are mediators of the interaction between the nervous system and the immune system. ILCs express receptors for neuropeptides and neurotransmitters.
- β2AR (β2-adrenergic receptor, is adrenaline and norepinephrine receptor): inhibit the proliferation and function of ILC2;
- NMUR1 (NMU receptor): Regulate ILC2 and maintain Th2-type protective immunity in the intestine;
- VPAC1/2 (vasoactive intestinal peptide receptor, VIP receptor): Regulates the production of IL-5 and maintains mucosal barrier homeostasis;
- CALCRL (calcitonin receptor-like, CGRP receptor): involved in Th2 asthma
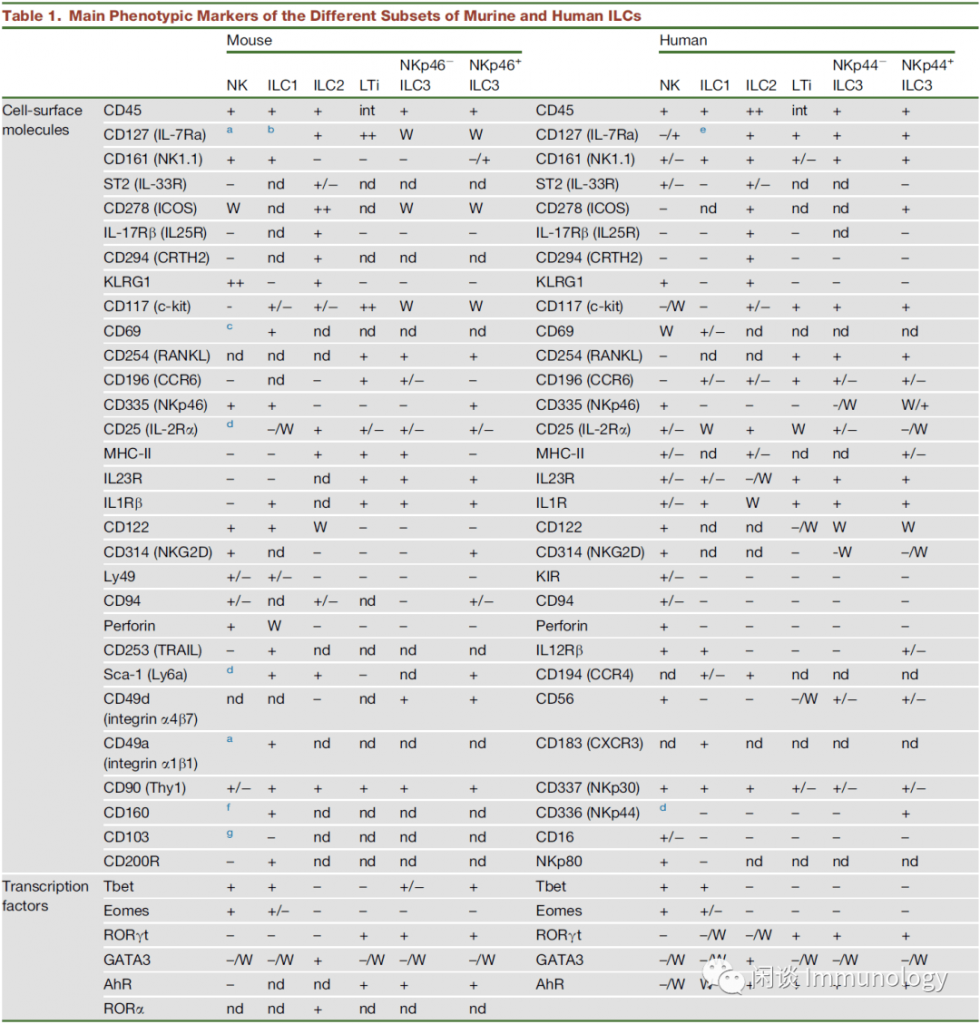
Markers of ILCs
Meow Comment: ILCs have had a lot of work in the past 10 years. As innate immune cells that echo Th1, Th2, and Th17, they reside in the tissues. Like NK, they fight on the front line of defense.
(source:intenet, reference only)



