Which brainstem glioma patients can undergo surgery?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Which brainstem glioma patients can undergo surgery?
Which brainstem glioma patients can undergo surgery? The purpose of surgery is to remove the tumor to the greatest extent while protecting the nerve function. Brainstem glioma can occur in all age groups, but it is more common in children and young people, and it also occurs in middle-aged and elderly people. The tumor is invasive, but some are nodular or mixed, or have cystic changes.
The clinical manifestations are different due to the location, scope and degree of brain stem damage caused by the tumor, and intracranial pressure may increase in the late stage. The blood supply of the tumor comes from the branches of the vertebral-basal artery and the posterior cerebral artery.
Brainstem gliomas with relatively limited tumors, nodular and well-differentiated, are suitable for surgical treatment. After surgery has achieved certain results, supplemented with radiotherapy can prolong survival, but due to the particularity of the brainstem anatomy, the operation is difficult Very high, many patients were also sentenced to “death penalty.”
Classification of brainstem glioma
At present, there is no unified imaging classification standard for brainstem glioma. From 1985 to 2000, there were 7 to 8 classification standards. The purpose of imaging classification is to judge whether the tumor is suitable for surgical treatment, to estimate the risk of surgery and to judge the prognosis. Among the many classification methods, the most important reference is the growth mode of the tumor (exogenous/endogenous, focal/diffusion), followed by the origin of the tumor.
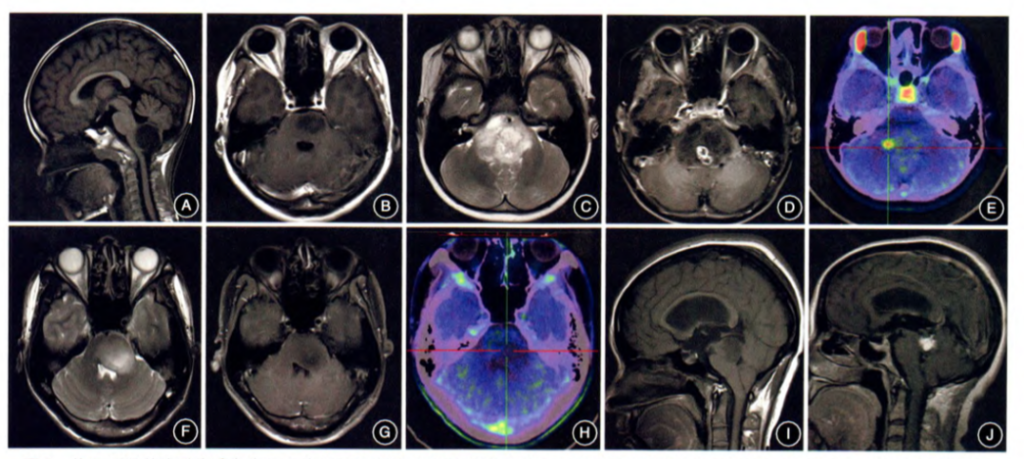
Classification of brainstem glioma based on MR imaging characteristics:
Type I:
Exogenous brainstem glioma, the tumor grows outward, and the main body is located outside the brainstem (Figure 1A).
Type Ⅱ:
Endogenous brainstem glioma, which can be divided into type Ⅱa that is focal endogenous type (Figure 1B) and type Ⅱb that is diffuse endogenous type. 11C-MET PET examination is recommended for type IIb brainstem glioma. Based on the characteristics of enhanced MRI scan and MET uptake, type IIb tumors can be classified as type IIb1 with focal enhancement or high metabolism (Figure 1 C ~E) and type IIb2 without focal enhancement or high metabolism (Figure 1F ~ H).
Type Ⅲ:
- It is a special type of brainstem glioma, type Ⅲa is tectorial glioma (Figure 1I);
- type Ⅲb is aqueduct glioma, which has a low incidence, with obstructive hydrocephalus as the first symptom The pathological types are mainly low-grade gliomas (Figure 1J);
- type IIIc is NF1-related brainstem gliomas, which can be distributed in any part of the brainstem, and can show various growth patterns and imaging characteristics.
Brainstem tumors are mostly gliomas, of which astrocytoma (including glioblastoma) accounts for the majority, and the rest are ependymoma, oligodendroglioma and mixed glioma. According to the tumor site, the pontine is the majority, and the midbrain and medulla oblongata are less, but sometimes it can spread to the entire brainstem. Tumors that originate in the medulla oblongata can also affect the upper cervical spinal cord.
Among them, the covered tumor is a focal tumor of the midbrain, which usually occurs in children under 14 years of age. They cause hemiplegia, oculomotor palsy, and ataxia by massively affecting the unilateral tegmental and corticospinal tract. In most cases, symptoms can be traced back 6-12 months before diagnosis. Occasionally, unilateral tremor can be seen, especially in patients whose tumors extend to the basal ganglia and thalamus. Later, I will share an article by James T . Professor Rutka’s case of brainstem-tegular glioma treatment can be used as a reference for other brainstem glioma patients.
Which brainstem glioma is suitable for surgery?
The surgical principle of brainstem glioma is to remove the tumor to the maximum extent under the premise of protecting function, so as to prolong the survival period of the patient; some patients with hydrocephalus or intracranial hypertension but not suitable for tumor resection can choose decompression, Shunting relieves symptoms. In addition to the indications listed below, whether or not to adopt surgical treatment should be comprehensively considered in consideration of the severity of the disease, the speed of progression, and the general condition and willingness of the patient. Brainstem gliomas suitable for surgery include the following types:
1. Surgical indications:
① Exogenous brainstem glioma.
② Focal endogenous brainstem glioma.
③ With focal enhancement or 11C-MET PET-CT, diffuse endogenous brainstem glioma with focal high metabolism.
④ For DIPGs without focal enhancement or 11C-MET PET-CT imaging without focal hypermetabolism, open biopsy or stereotactic biopsy can be selected.
⑤ Gliomas that showed a tendency to become malignant during the observation period (increased in volume, enhanced on MRI-enhanced scans, and invaded surrounding structures).
2. Surgery contraindications:
① Diffuse brainstem glioma involves the entire brainstem (midbrain, pons, medulla oblongata).
② Brainstem glioma with disseminated or implanted pia mater.
③Patients with Karnofsky functional status score (KPS) <50 and severe brainstem failure.
④ Patients with multiple organ dysfunction who cannot tolerate surgery.
3. Formulation of surgical plan:
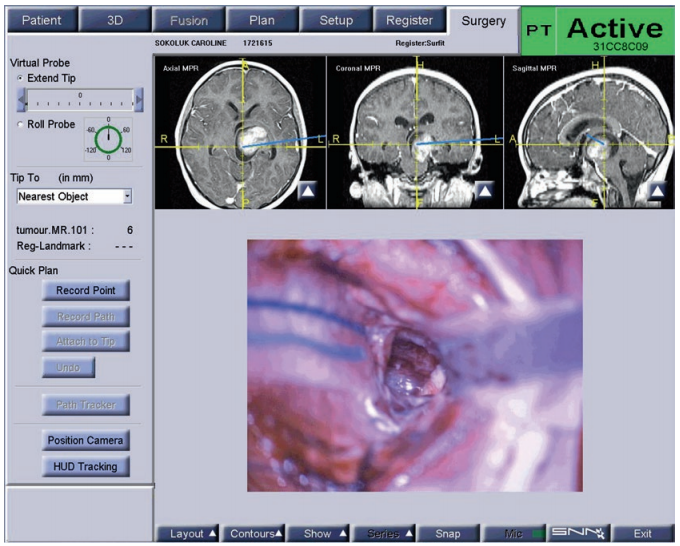
The commonly used surgical approaches for different parts of brainstem glioma are shown in Table 2. The choice of a safe entry point for the brainstem is very important. It is recommended to avoid the important conduction tracts and nuclei in the brainstem under the guidance of fiber tract navigation and intraoperative neuroelectrophysiological monitoring, and select the area of the brainstem closest to the tumor to enter The brainstem should be cut along the direction of the fiber bundle to avoid excessive damage to the fiber bundle. During the operation, reduce the mechanical traction of the brainstem as much as possible, and avoid damage to the normal blood supply artery and drainage vein of the brainstem as much as possible.
Common surgical approaches for different parts of brainstem glioma
Treatment case of INC International Professor
In his early childhood, Luke went to the doctor for symptoms such as brown spots on the body and pain in the lesion. After the diagnosis of type 1 neurofibromatosis, he continued to receive medication and his condition was stable. However, Luke developed headache and vomiting symptoms when he was 13 years old. The results of the review showed that the brainstem lesions caused the tectum and the fourth ventricle to be affected. The operation is imperative, but the operation in the “forbidden area” of the brainstem is extremely difficult. A little carelessness can cause disability and paralysis, and the condition is extremely dangerous. It is recommended that the family make an early decision.
After learning more about Luke’s condition and related information, Professor Rutka said: He can perform surgery on the child and can safely remove most of the tumors. According to the postoperative situation, he will decide whether to supplement chemotherapy and specific treatment plans. However, radiotherapy is not recommended for the time being. After receiving affirmative reply from Luke’s parents, Professor Rutka and his team quickly performed resection on the child. The temporal craniotomy was performed through the left middle temporal gyrus to the lesion. Intraoperative neuronavigation is used to determine the boundary of the tumor and remove the lesion with an ultrasonic knife.
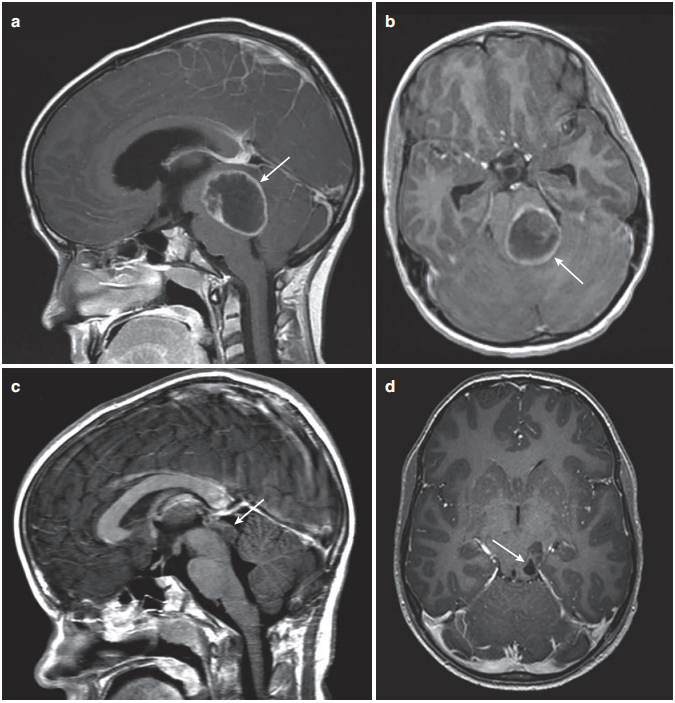
figure 2. (a) Sagittal enhanced T1 MRI showed a huge posterior fossa cystic lesion, with the tumor centered in the tectal area (arrow). (b) Enhanced MRI shows the degree of involvement of the tectum and fourth ventricle (arrow). (c) After the posterior fossa craniotomy, drainage of the tumor cyst, and the cyst cyst are removed, only a small top cover deformation can be seen on the MRI enhancement (arrow). (d) Postoperative enhanced MRI showed that the tumor originated in the parietal region without space-occupying effect (arrow).
Professor Rutka believes that, in terms of access and long-term treatment, focal tegmental tumors are a huge challenge for neurosurgeons. The choice of surgical approach includes transsylvian approach, transtemporal approach or transcorporeal approach, depending on the size of the tumor, primary location and growth morphology. The professor of surgery chose the transtemporal approach . The best neurosurgical resection is through the use of neuronavigation, especially magnetic resonance diffusion tensor imaging sequence, intraoperative neuronavigation, and intraoperative MRI scan assistance, as he did in Luke’s operation.
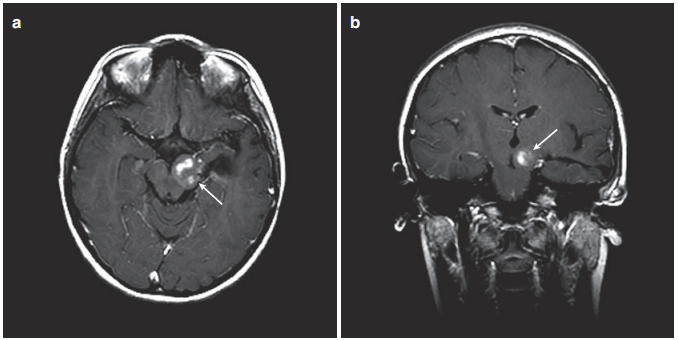
No new neurological dysfunction appeared 2 weeks after the operation. The child only experienced transient memory impairment and recovered quickly. Postoperative growth and intellectual development were normal. However, because the tumor still remains, Professor Rutka and the team have discussed internally for many times, taking into account the child’s age, tumor residual status, and past medical history, and formulated an exclusive chemotherapy regimen for Luke. Facts have proved that the child tolerates this regimen. It’s in good condition. Follow-up data showed that he continued to receive chemotherapy during the follow-up period, but Luke no longer needed further surgical treatment, which made his family very happy.
Summary
The purpose of surgery is to remove the tumor to the greatest extent while protecting the nerve function. Children with focal midbrain tumors can perform very well after aggressive neurosurgical removal of the tumor.
If there is residual tumor after surgery and continues to progress, then for older children, there are options such as targeted chemotherapy, conventional chemotherapy, or radiation therapy. With the greatest degree of safety, most children with focal midbrain tumors can lead a normal life.
In view of the possibility of recurrence, continuous MR review is strongly recommended. Overall, children with focal midbrain tumors have a good prognosis, with a 5-year-old survival rate of 90% or higher.
(source:chinanet, reference only)
Disclaimer of medicaltrend.org



