When does spinal tuberculosis need surgery?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
When does spinal tuberculosis need surgery?
When does spinal tuberculosis need surgery?. The spine is the load-bearing beam of the human body. Once damaged, the spine will become unstable.
1. What are the hazards of spinal tuberculosis?
The spine is the load-bearing beam of the human body. Once damaged, the spine will become unstable. If not treated in time, the entire vertebral body and its appendages will be destroyed, leading to spinal deformities, even compressing the spinal cord and causing paralysis.
Some spinal tuberculosis abscesses will penetrate the skin to form a fistula, puncture organs or blood vessels, and form corresponding complications, which will cause great damage to the patient and a high rate of disability and teratogenesis.
2. What kind of deformity will appear with spinal tuberculosis?
According to anatomical stability, the spine is divided into anterior, middle and posterior columns. Spinal tuberculosis tends to occur in the anterior column. The bone is damaged and the supporting force is reduced, causing the instability and collapse of the anterior column. Coupled with the influence of weight and gravity, it is easy to form “kyphosis”.
3. Will spinal tuberculosis cause paraplegia?
Tuberculosis destroys the vertebral body and leads to pathological fractures. The twisted spinal canal causes compression of the spinal cord, or the abscess protrudes into the spinal canal to compress the spinal cord, which can cause the patient to be paralyzed in a relatively short period of time.
In addition, tuberculosis lesions cause damage to the vertebral body. Even with anti-tuberculosis treatment, progressively worsening kyphosis may still occur over time, and the patient slowly develops symptoms of paralysis.
4. Under what circumstances do spinal tuberculosis require surgical treatment?
In the early stage, patients without severe bone destruction, giant abscesses and nerve tissue compression can be cured with anti-tuberculosis drugs. Consider surgical treatment when the following situations occur:
(1) Bone destruction affects the stability of the spine; (2) The nerve tissue is compressed, causing progressively worsening symptoms of paralysis; (3) Progressively worsening kyphotic deformity; (4) Flowing abscess formation, large seizures And vertebral body hollow, long-lasting tuberculosis sinus.
5. What are the surgical methods for spinal tuberculosis?
The purpose of spinal tuberculosis surgery is to remove tuberculosis foci, relieve nerve compression, rebuild spinal stability, save nerve function and rebuild spinal stability as much as possible.
Surgery for treatment of spinal tuberculosis is divided into anterior, posterior and combined anterior and posterior approaches, such as: anterior debridement and bone grafting, anterior debridement and bone graft internal fixation, anterior debridement and bone graft combined with posterior internal fixation, and simple posterior Road lesion removal, bone grafting and internal fixation.
6. Does spinal tuberculosis need bone grafting and internal fixation?
Some patients with spinal tuberculosis cause bone destruction of the vertebral body, loss of spinal stability, or large bone defects after surgical removal of the lesion. At this time, bone grafting and internal fixation are required to restore spinal stability.
Bone graft fusion and internal fixation is an important method for spinal tuberculosis surgery. The commonly used bone graft materials in clinical practice include autologous bone, allogeneic bone, xenogeneic bone and other biological bone materials. Autologous iliac bone is recognized as the best bone graft material.
Instrument internal fixation is more stable and reliable than external fixation, providing a good bone growth environment for bone grafting, effectively correcting kyphosis and restoring the normal line of force of the spine.
7. Typical cases
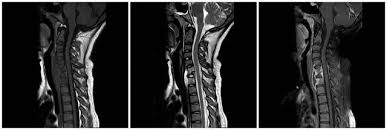
A 52-year-old female, due to “intermittent low-grade fever for 3 months, back pain and no lower limbs for 20 days”, went to the outpatient clinic. Within 20 days of the patient, the muscle strength of both lower limbs decreased progressively. At the time of treatment, the lower limbs were completely paralyzed and the feeling decreased. , Urinary incontinence, place a urinary catheter. Imaging examination showed: T5 vertebral body compression fracture, accompanied by vertebral body soft tissue space.
In view of the patient’s condition, because the lesion is located in the upper thoracic spine, the front of the spinal cord is compressed significantly, and only indirect decompression through the rear, the surgical effect is extremely limited. Surgery requires direct removal of ventral compression of the spinal cord. However, the front decompression of the thoracic spine via the posterior approach makes the operation extremely difficult and the risk of spinal cord injury during the operation is extremely high. At the same time, there are important organs such as cardiovascular, trachea, and lungs around the lesion. A little carelessness may lead to serious adverse events.
At the same time, the patient was hospitalized with hypoproteinemia and moderate anemia, and the patient had poor tolerance to surgery. Therefore, Professor Chen Yu first considers improving the patient’s surgical tolerance, and giving the patients symptomatic treatment such as albumin supplementation and red blood cell enhancement. At the same time, a series of intraoperative surgical aids such as drill grinding, ultrasonic bone knife, and intraoperative ultrasound were prepared to improve the accuracy of the operation.
The operation lasted 4 hours and ended smoothly. Now the patient’s lower limb activities and muscle strength have basically returned to normal 2 weeks after the operation.
(sourceinternet, reference only)
Disclaimer of medicaltrend.org



