Feasibility of application of opioid-free anesthesia (OFA) in lung resection
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Feasibility of application of opioid-free anesthesia (OFA) in lung resection
Feasibility of application of opioid-free anesthesia (OFA) in lung resection. There are still few clinical studies on the application of OFA in thoracic surgery. The above-mentioned research wittily achieved the OFA in thoracic surgery through intravenous use of lidocaine and magnesium sulfate assisted with various nerve block techniques, and obtained reliable results. The postoperative analgesia effect.
Background
Thoracic surgery lung cancer surgery is more traumatic, and the intraoperative and postoperative pain is significantly more severe than other operations. Effective analgesia can greatly reduce the incidence of various postoperative complications, and opioids ensure effective pain control The best means. However, opioids are not without their shortcomings. They may cause postoperative respiratory depression and affect immune regulation, leading to cancer progression and increased susceptibility to infection.
In addition, they may also increase the incidence of postoperative intestinal obstruction, nausea and vomiting, dizziness and itching, which will have a serious adverse effect on postoperative recovery. Because of this, the concept of opioid-free anesthesia (OFA) came into being. This article aims to explore the feasibility of OFA in lung cancer resection.
Due to the related side effects of opioids and their possible role in the immunosuppression of malignant tumors, opioid-saving strategies have been incorporated into the current mainstream anesthesia methods. With the vigorous development of nerve block technology and the development of non-opioids With the improvement of the concept of multi-modal analgesia management with similar drugs, the implementation of opioid-free anesthesia (OFA) has also become possible.
In recent years, OFA has been used in breast surgery, laparoscopic surgery and obstetric surgery. Compared with traditional anesthesia, patients in the OFA group did not observe a significant increase in perioperative pain, and because of the elimination of opioids The related side effects brought about, the patient’s hospital stay was significantly shortened.
A study in 2020 included 83 patients undergoing elective lung resection for the first time in the OFA group, and retrospectively matched 83 patients in the standard opioid-based technique (STD group) for analysis.
In the OFA group, the full name did not use any opioids during the operation, and the stress stimulus by inserting a double-lumen tube during induction was administered intravenously with propofol (2-3 mg/kg) and lidocaine (0.75-1 mg/kg) ) And magnesium sulfate (0.05-0.1mmol/kg). The patient was given a paravertebral nerve block (containing 0.25% bupivacaine 1 mg/kg plus clonidine 0.5-1.5 mg/kg) before operation. When hypertension occurs during the operation, the anesthesia is appropriately deepened and a single intravenous push is 0.05- 0.1mmol/kg of magnesium sulfate. In the STD group, patients did not completely unify the intraoperative anesthesia and analgesia. The opioids used included remifentanil, fentanyl, sufentanil, and morphine. Lidocaine and morphine were not used during induction intubation. Magnesium sulfate.
If there are no clear contraindications, the two groups of patients will use non-steroidal analgesics and the patient’s hand-controlled intravenous analgesics during the perioperative period. In both groups, the patients undergoing laparoscopic surgery will be given local anesthetics when the surgeon is concerned. Intercostal nerve infiltration anesthesia. If an open operation is performed, an extrapleural catheter is placed under direct vision by the surgeon, and 0.25% bupivacaine is continuously pumped within 24 hours after surgery.
The main observation indicators are the pain scores of the patient at 0, 1 and 24 hours after entering the recovery room (0 points for no pain at all, 1 point for mild pain, 2 points for moderate pain, and 3 points for severe pain), and the patient’s total pain in the recovery room The length of time and the patient’s hospital stay.
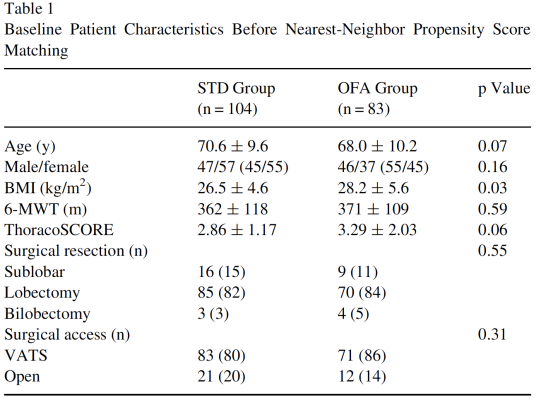
The study observed no significant differences in the baseline data of the two groups of patients (p>0.05), including gender composition, BMI, physical fitness, and surgical methods (Table1).
Devine G ,Cheng M ,Martinez G ,et al. Opioid-free anesthesia for lung cancer resection: A case-control study. J Cardiothorac Vasc Anesth. 2020; 34: 3036-3040.
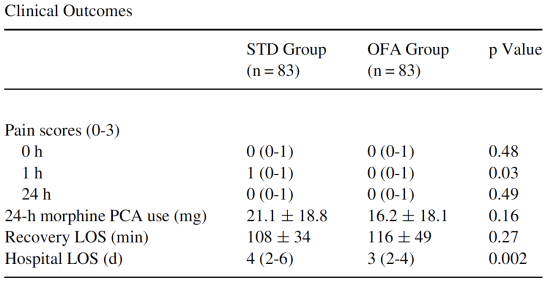
The pain degree of patients in the OFA group was lower than that of the STD group at 1 hour after surgery (p=0.03), and the pain degree at 0 and 24 hours was similar to the STD group. There was no significant difference in the amount of morphine used for postoperative analgesia and the total length of the recovery room between the two groups, but the total length of stay in the OFA group was significantly shorter than that of the STD group (p=0.002). (Table2)
Table2
Devine G ,Cheng M ,Martinez G ,et al. Opioid-free anesthesia for lung cancer resection: A case-control study. J Cardiothorac Vasc Anesth. 2020; 34: 3036-3040.
At present, there are still few clinical studies on the application of OFA in thoracic surgery. The above-mentioned research wittily achieved the OFA in thoracic surgery through intravenous use of lidocaine and magnesium sulfate assisted with various nerve block techniques, and obtained reliable results. The postoperative analgesia effect.
However, this study also has its limitations. Especially in the OFA group, some patients need to receive paravertebral block (using bupivacaine and clonidine), intercostal nerve infiltration block, extrapleural catheter, Is perioperative intravenous injection of acetaminophen, oral ibuprofen, and a self-controlled intravenous morphine analgesic pump, is such a fanfare operation really necessary? Every drug has its advantages and disadvantages. Do opioids really need to be completely abandoned? This is what we need to think about.
Of course, OFA certainly has its advantages in certain populations, especially considering that opioids may lead to the progression of cancer, but the safety and necessity of OFA in thoracic surgery still urgently need large samples and high-quality studies to confirm.
(source:internet, reference only)
Disclaimer of medicaltrend.org



