BMJ: Coffee can reduce the risk of prostate cancer
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
BMJ: Coffee can reduce the risk of prostate cancer
BMJ: Coffee can reduce the risk of prostate cancer. Caffeine can improve glucose metabolism, has anti-inflammatory and antioxidant effects, and affects sex hormone levels…
Recently, the scientific journal “BMJ Open” published online the results of a study from Chinese scholars: Higher coffee intake may be related to lowering the risk of prostate cancer. In other words, drinking more coffee in adult men can reduce the risk of prostate cancer.

Previous studies have shown that drinking more coffee is related to reducing the relative risk of liver cancer, bowel cancer and breast cancer. In order to study the relationship between coffee intake and prostate cancer risk, the research team searched the database to collect data on the correlation between prostate cancer risk and coffee sales.
Finally, 16 studies were included, of which 7 were conducted in North America, 7 were conducted in Europe, and 2 were conducted in Japan. The total cohort included more than 1 million (1081586) men, of which 57,732 had prostate cancer.
The statistical results show that:
❖ Compared with low coffee consumption (less than 2 cups per day), people with high coffee consumption (two or more cups per day) have a 9% lower risk of prostate cancer, and every extra cup of coffee consumed per day reduces the risk of prostate cancer by 1 %.
❖ Compared with low coffee consumption (less than 2 cups per day), people with high coffee consumption (2 cups or more per day) reduce the risk of local prostate cancer by 7%, and the risk of advanced and fatal prostate cancer by 12%-16% .
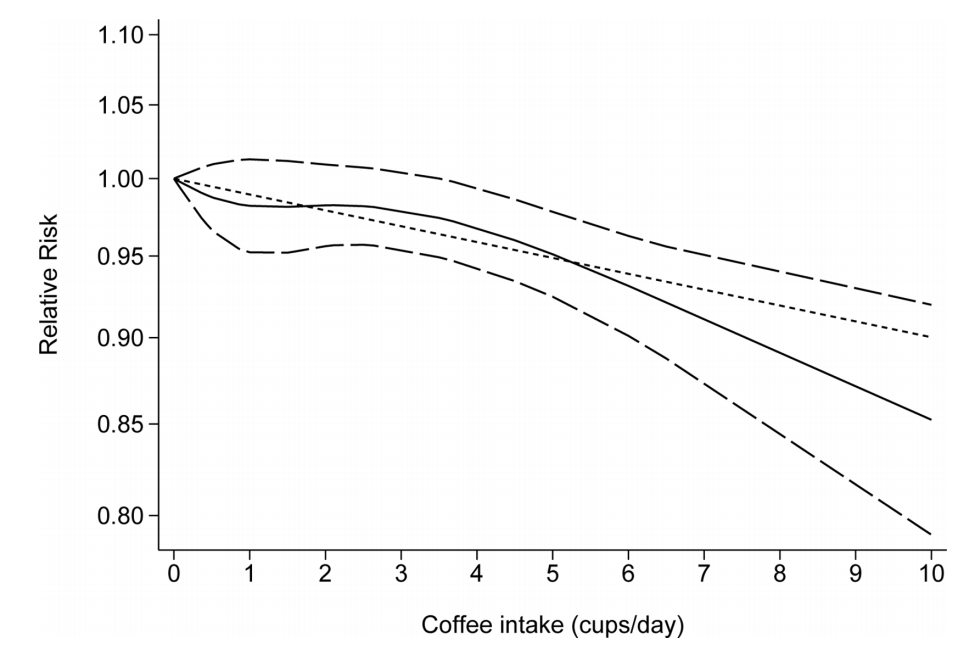
Overall, as the number of coffee cups consumed daily increases, the risk of prostate cancer decreases
The researchers explained that caffeine can improve glucose metabolism, has anti-inflammatory and antioxidant effects, and affects the level of sex hormones. These effects may affect the occurrence and further development of prostate cancer.
It should be noted that to determine the underlying mechanism and the key active substances that play a role, further research is still necessary so that it can provide relevant basis for guiding the primary prevention strategy of prostate cancer in the future.
Prostate cancer: the 4th largest cancer in the world
The latest global cancer burden data released by the International Agency for Research on Cancer (IARC) of the World Health Organization in 2020 show:
In 2020, prostate cancer will become the 4th most common cancer in the world. The incidence is second only to breast, lung and colorectal cancer. More than 1.41 million (1414259) people have new prostate cancer. At the same time, prostate cancer is also male worldwide The second largest cancer, more than 370,000 (375,304) people died of prostate cancer.
In China, more than 110,000 (115,426) people will be newly diagnosed with prostate cancer in 2020, ranking 6th in the number of newly diagnosed cancers in Chinese men; at the same time, more than 50,000 (51094) million people will die of prostate cancer, accounting for Chinese men’s cancer The 7th in the death toll. Although the incidence of prostate cancer in our country is much lower than that of European and American countries, with the aging of the population and changes in lifestyles, the incidence is increasing significantly. According to the National Cancer Center, prostate cancer has become the most common tumor in the male urinary system since 2008. In 2015, the incidence of prostate cancer in Shanghai exceeded that of liver cancer for the first time, and it became the fourth highest incidence of male malignant tumors in Shanghai, which was close to that of developed countries in Europe and America.
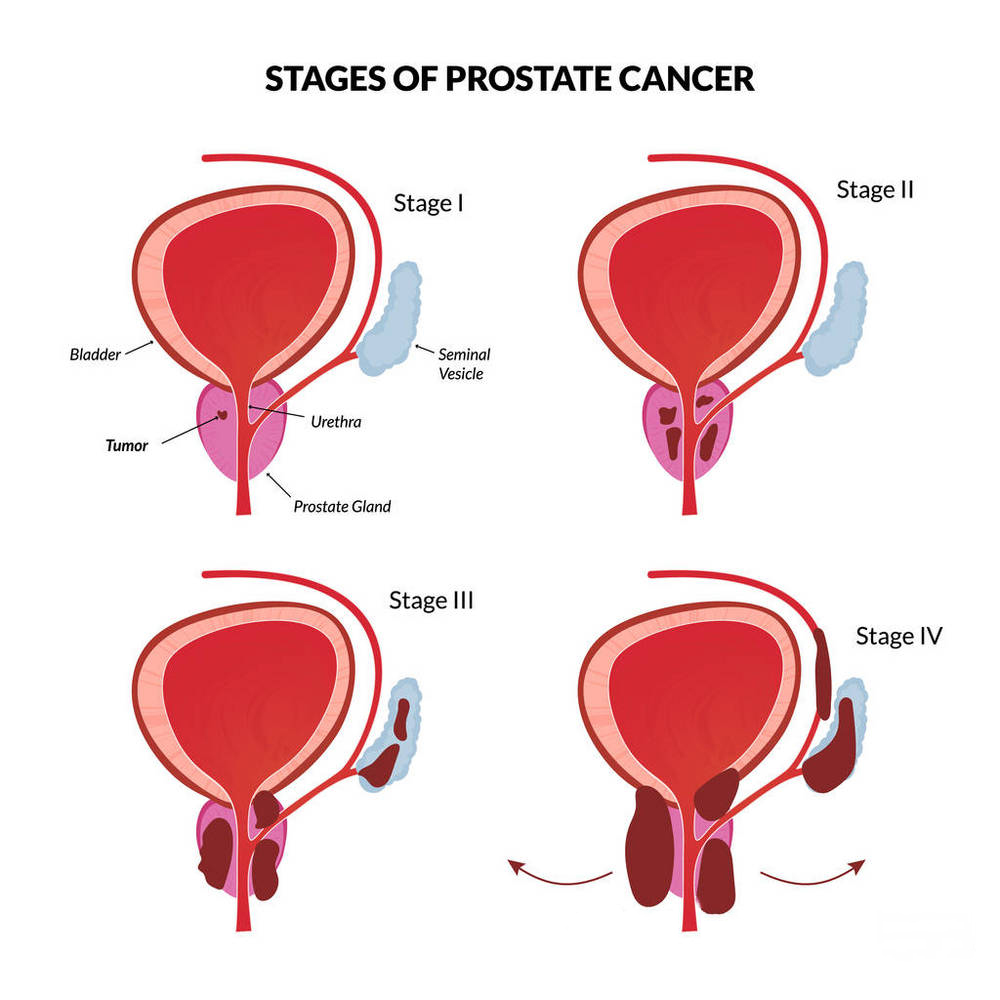
Only 30% of the new cases in China were clinically limited patients at the time of diagnosis, and the others were patients with locally advanced or extensive metastases. From the perspective of disease progression, androgen deprivation therapy (ADT) is mostly effective in the initial treatment of high-risk advanced prostate cancer and metastatic prostate cancer (mPC) patients, but as the disease progresses, most will turn into metastatic castration resistance Prostate cancer (mCRPC), which is the main cause of death from prostate cancer.
External radiotherapy: similar to radical resection
According to the “Prostate Cancer Diagnosis and Treatment Standards” (2018 edition) issued by the National Health Commission: Radical external radiotherapy (EBRT) is similar to radical prostatectomy and is one of the most important radical treatment methods for prostate cancer patients. It has the advantages of good curative effect, wide indications, small complications and adverse reactions.
For low-risk prostate cancer, external radiotherapy can achieve a similar effect to radical surgery. For metastatic prostate cancer, external radiotherapy is an important means of reducing tumors and symptoms.
Localized prostate cancer:
Low-risk patients (T1~2a, Gleason ≤6, PSA<10 ng/ml): Both external radiotherapy and radical prostatectomy are the preferred methods, and radical external radiotherapy is the first choice for elderly patients.
Intermediate-risk patients (T2b or Gleason 7 or PSA 10-20 ng/ml): radiotherapy and surgery are the preferred methods. For elderly patients, radical external radiotherapy is recommended as the first choice, combined with short-course neoadjuvant/contemporaneous/adjuvant endocrine therapy (4 ~6 months).
High-risk patients (≥T2c or Gleason≥8 or PSA>20 ng/ml): External radiotherapy is the first choice, combined with long-term neoadjuvant/contemporaneous/adjuvant endocrine therapy (2 to 3 years), but surgery is optional.
Locally advanced prostate cancer (T3~4N0M0): Radical external radiotherapy is the first choice, combined with long-term neoadjuvant/contemporaneous/adjuvant endocrine therapy (2~3 years).
The “Consensus on the Safety of Radiotherapy for Prostate Cancer” points out: High-dose image-guided radiotherapy (IGRT) has become the gold standard technique for radical external radiotherapy. The IGRT technology based on daily confirmation of the location of prostate cancer can significantly reduce the boundary of the target area and improve the accuracy of treatment. Quality assurance (QA) plays a vital role in the implementation of radiotherapy plans.
TOMO radiotherapy integrates IMRT (intensity-modulated conformal radiotherapy), IGRT, and DGRT (dose-guided intensity-modulated conformal radiotherapy). It has the dual verification function of image verification and dose verification. Before each treatment, not only the two CT The image data is compared, and the actual absorbed dose of the tumor and surrounding normal tissues is compared with the calculated dose in the treatment plan to ensure the high accuracy of each treatment and raise the safety to a new level.
(source:chinanet, reference only)
Disclaimer of medicaltrend.org



