Diagnosis and treatment of primary brainstem hemorrhage
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Diagnosis and treatment of primary brainstem hemorrhage: History, Current situation and Future
Diagnosis and treatment of primary brainstem hemorrhage. This issue focuses on spontaneous intracerebral hemorrhage. Spontaneous intracerebral hemorrhage is one of the two major types of hemorrhagic stroke.
It has a wide range of classifications and complex etiologies. Hypertensive intracerebral hemorrhage is the most common in some countries, and it is mostly described as primary in foreign literature. Cerebral hemorrhage. Hypertensive cerebral hemorrhage is a diagnosis of exclusion. It is necessary to exclude secondary cerebral hemorrhage caused by vascular structural diseases (such as intracranial aneurysms, intracranial arteriovenous malformations, and cavernous malformations).
Primary brainstem hemorrhage is the subtype with the highest disability rate and case fatality rate among hypertensive cerebral hemorrhage. Whether surgical treatment is obviously different in Eastern and Western countries, or even completely opposite, cultural differences play an important role. Among them, Western countries such as Europe and the United States Pay more attention to the quality of life, coupled with the restrictions of the medical insurance system, can not accept the long-term coma, bedridden and other low-quality living conditions of postoperative patients; Asian countries have made many efforts to save the lives of patients, thinking that survival has the opportunity to talk about the quality of life .
some countries has accumulated a lot of clinical experience in the surgical treatment of primary brainstem hemorrhage, which clearly confirms the role of surgery in saving the lives of patients. The surgical methods include traditional craniotomy, stereotactic puncture, aspiration, and internal surgery. Microscope-assisted hematoma removal. The choice of surgical method is based on the patient’s condition, medical center conditions and the experience of the surgeon.
It is particularly emphasized that “minimally invasive” is a concept that has nothing to do with surgical methods and surgical incisions. The treatment that achieves the purpose of surgery while minimizing brain damage is minimally invasive treatment. There is still a lack of high-level evidence-based medical evidence regarding the timing of surgery. Based on clinical experience and the persistent toxic mechanism of hematoma on brain tissue, surgical treatment within 24 hours of onset is better than late surgery. In general, there is currently no treatment that can clearly improve the neurological function of patients with hypertensive intracerebral hemorrhage, and it is necessary to find the best surgical treatment indication.
Summary
Primary brainstem hemorrhage is the subtype with the worst prognosis among all types of cerebral hemorrhage. At present, there is no unified diagnostic criteria, which mainly relies on the history, clinical manifestations and imaging characteristics of hypertension, and excludes cerebrovascular structural lesions and tumor strokes. Its treatment is still controversial. European and American countries advocate conservative treatment, while Asian countries including China, South Korea and Japan have conducted a lot of research on surgical treatment. At present, the research of primary brainstem hemorrhage is progressing slowly, and high-quality clinical research is mainly lacking. In the future, we hope to further clarify the best treatment plan through multicenter cohort studies or randomized controlled trials.
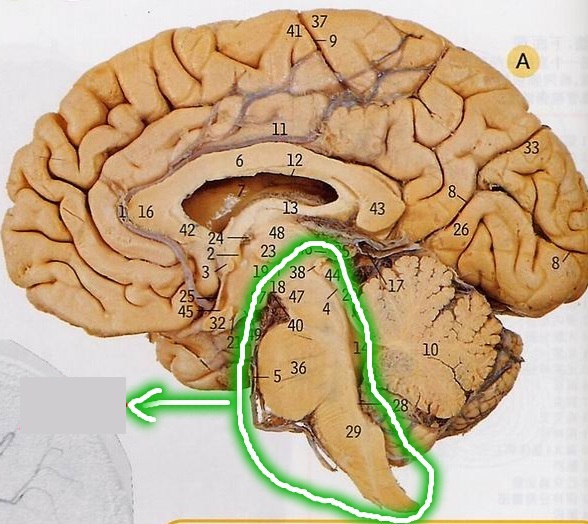
Primary brainstem hemorrhage (PBSH), which is usually called hypertensive brainstem hemorrhage in China, mainly occurs in the pons, so European and American countries also call it primary pons. Primary brainstem hemorrhage accounts for 6% to 10% of all spontaneous intracerebral hemorrhages. It is the type of hemorrhagic stroke with the worst prognosis. The fatality rate is about 65%. The case fatality rate varies depending on the bleeding site and the amount of bleeding. The prognosis of most patients with neurological function is extremely poor.
This article briefly reviews the diagnosis and treatment history of primary brainstem hemorrhage, summarizes the current status of treatment, especially the current controversial surgical treatment methods, and looks forward to possible future treatment prospects.
1. Diagnosis and treatment history
The term brainstem hemorrhage was first described by Cheyne and Underwood in the article “Stroke and Drowsiness” in 1812, and there have been few reports since then. By 1932, Dandy reported the first case of primary brainstem hematoma.
In 1939, Környey described in detail the complete process of the onset, death, and autopsy of a patient with pons hemorrhage. Since then, similar cases have been reported in the literature for more than 30 years. In 1973, Romanian neurosurgeons Arseni and Staneiu reported 2 patients with primary brainstem hematoma and reviewed all 11 previous similar cases, and proposed the main points for the differential diagnosis of primary brainstem hematoma and brainstem hemorrhage, namely, brainstem hemorrhage. The hematoma is limited and the onset is slow. The main manifestations are hemiplegia, facial paralysis and mild disturbance of consciousness; the onset of brainstem hemorrhage is rapid and progresses rapidly, mainly manifested as coma, high fever, respiratory disorder, quadriplegia, etc.
They believe that the emphasis on the importance of the differential diagnosis of primary brainstem hematoma and brainstem hemorrhage is because the treatment methods of the two are completely different. The treatment of brainstem hematoma is mainly surgical treatment, while brainstem hemorrhage should be conservatively treated in internal medicine. treatment.
The brainstem hemorrhage proposed by Arseni and Staneiu is the prototype of primary brainstem hemorrhage. It was not until 1988 that Mangiardi and Epstein accurately distinguished primary brainstem hemorrhage from other brainstem hemorrhage diseases, and defined “primary brainstem hemorrhage” as a diffuse brainstem hemorrhage disease that occurred in elderly patients, accompanied by There is severe and irreversible neurological dysfunction, and the fatality rate is extremely high (about 65%). It is particularly pointed out that the disease is often accompanied by systemic hypertension, which needs to be differentiated from the brainstem cavernous malformation.
Before the advent of CT technology, the diagnosis of brainstem hemorrhage was mainly based on clinical manifestations. Ventriculography and internal carotid cerebrovascular angiography can assist in the diagnosis, but it is difficult to distinguish primary brainstem hemorrhage from brainstem cavernous malformations and occult cerebrovascular malformations. Differentiate the secondary brainstem hemorrhage caused by others.
So far there is no universal diagnostic criteria for primary brainstem hemorrhage. The following items are available for reference:
(1) There is a clear history of hypertension.
(2) The onset is sudden, and most patients have obvious disturbance of consciousness, which can be distinguished from the brainstem cavernous malformation. The latter is mainly manifested as cranial nerve dysfunction, while the disturbance of consciousness is not obvious. This is due to the different pathogenesis of the two diseases. Primary brainstem hemorrhage is caused by the rupture of the perforating artery. The hemorrhage has destructive damage to the surrounding brainstem tissue, including the reticular activation system, and can cause obvious disturbance of consciousness; The rupture of cavernous vascular malformation hemorrhage is the blood sinus bleeding in the malformation group, and the surrounding tumor wall is buffered. Therefore, the bleeding has a swelling and oppressive effect on the surrounding brainstem tissue, and the clinical symptoms are mild.
(3) Primary brainstem hemorrhage on CT usually runs through the transverse diameter of the brainstem, showing diffuse hemorrhage in a long fusiform or irregular shape; brainstem cavernous vascular malformations are mostly regular round or elliptical.
(4) It is difficult to differentiate between primary and secondary brainstem hemorrhage based on clinical symptoms or simple hematoma morphology. CTA or DSA should be performed to rule out structural cerebrovascular disease, and MRI enhancement scan to rule out tumor stroke.
Before the application of CT technology in clinical practice, primary brainstem hemorrhage was mainly treated by internal medicine, including close monitoring of vital signs, maintaining a smooth airway, actively lowering blood pressure, correcting central high fever, and preventing lung infection, gastrointestinal hemorrhage and venous thrombosis Wait. CT can accurately locate the location and size of brainstem hemorrhage, providing basic conditions for surgical treatment. At the same time, the development of CT-based stereotactic systems has laid the foundation for intraoperative localization of brainstem hemorrhage. Because cerebral hemorrhage is mainly seen in Asian populations, especially in East Asian countries such as Japan and South Korea, the surgical treatment of primary brainstem hemorrhage originated in the above two countries.
In 1989, Japanese scholar Takahama and others first used CT-based stereotactic system puncture and aspiration to treat primary brainstem hemorrhage, creating a precedent for surgical treatment. After a long period of time, CT stereotactic puncture and aspiration became the main surgical treatment for primary brainstem hemorrhage. In 1998, South Korean scholar Hong et al. performed craniotomy on 13 patients with severe pons hemorrhage, and found that the surgical operation within 24 hours after the onset of the disease was not effective, and the surgical operation was performed 6 to 20 days after the onset of the disease. Some patients whose condition deteriorated during conservative treatment in internal medicine Effective, making the removal of hematoma under the microscope a craniotomy as another option for the treatment of primary brainstem hemorrhage. Compared with stereotactic puncture and aspiration, craniotomy surgery has more thorough removal of hematoma, faster hemostasis, and less possibility of postoperative rebleeding, but it has higher requirements for intraoperative brain tissue protection and microscopic operation.
2. Current status of surgical treatment
1) Indications
In 1992, Chung and Park classified primary brainstem hemorrhage into four types according to the area affected by the hematoma, namely unilateral tegmental type, basal tegmentation type, bilateral tegmentation type and giant type (occupying the base and the base of the brainstem). Covered part), the survival rates were 94.1%, 26.1%, 14.3%, and 7.1%, respectively. In 2017, domestic Huang et al. published a new brainstem hemorrhage prognosis scoring system in Stroke, according to the hematoma volume and state of consciousness score, where hematoma volume <5 ml is 0, 5 ~ 10 ml is 1,> 10 ml is 2, Glasgow The coma scale (GCS) scores 8 to 15 are 0, 5 to 7 are 1, 3 to 4 are 2, and the total scores 0, 1, 2, 3, and 4 are respectively 2.7% and 31.6 30 days after the onset of the disease. %, 42.7%, 81.8% and 100%.
It can be seen that, for severe patients with huge brainstem hemorrhage or brainstem hemorrhage severity score> 2, the mortality rate of medical conservative treatment is extremely high, and this type of patients is the main target group of surgical surgery.
Shrestha et al. proposed specific surgical indications for primary brainstem hemorrhage: (1) The volume of hematoma> 5 ml, and the hematoma is relatively concentrated. (2) GCS score <8, with progressive neurological dysfunction. (3) Unsteady vital signs, especially for patients who require ventilator-assisted ventilation.
2) Cultural differences
There are significant differences in the perception of life in Eastern and Western cultures, which directly lead to obvious regional differences in the surgical operations of primary brainstem hemorrhage. The general view in European and American countries is that postoperative severe disability or survival in a vegetative state is an extremely high mental and economic burden for the patient or his family. Such a clinical prognosis cannot be accepted, so surgical treatment is hardly performed. In 2015, the “Guidelines for the Treatment of Spontaneous Intracranial Hemorrhage” formulated by the American Heart Association (AHA)/American Stroke Association (ASA) clearly did not support
Surgical treatment.
Since the end of the 1990s in some countries, the surgical treatment of brainstem hemorrhage has been carried out. Initially, it was only carried out in large medical centers in big cities. Later, it was also carried out in primary hospitals and gradually gained popularity. After searching, there are nearly one hundred Chinese literatures on the surgical treatment of primary brainstem hemorrhage after 2000, covering minimally invasive treatment methods, surgical approaches, surgical efficacy and postoperative complications, as well as intraoperative electrophysiological monitoring , Robot-assisted positioning, endoscopy, hematoma removal, perioperative monitoring and intraoperative medical and nursing cooperation, etc., are comprehensive in content and have a definite effect in reducing the mortality rate.
3) Surgical methods
Microscopic craniotomy for hematoma removal in the treatment of primary brainstem hemorrhage has many advantages. It can remove the hematoma as much as possible at one time under direct vision, observe active hemorrhage and accurately stop the bleeding, and remove the broken into the fourth ventricle at the same time. Hematoma, so that the circulation of cerebrospinal fluid is unobstructed, as far as possible to avoid secondary hydrocephalus caused by the second operation. Common surgical approaches for brainstem hemorrhage include the suboccipital posterior median approach, the retrosigmoid sinus approach, and the subtemporal approach.
The suboccipital posterior median approach is usually used for pons-covered hematomas, especially for those who break into the fourth ventricle, bite off the foramen magnum and part of the posterior arch of the atlas, open the cisterna magna, fully release the cerebrospinal fluid, and reduce intracranial pressure , Removal of part of the inferior cerebellar vermis to expose the fourth ventricle. After clearing the intraventricular hematoma, it can be observed under the microscope that the hematoma breaks through the break in the brainstem.
The transinfratemporal approach is suitable for hemorrhage of the midbrain and hematoma extending to the thalamus. The focus of the operation is to expose the hematoma. Avoid stretching the temporal lobe by changing the position, releasing the cerebrospinal fluid, and cutting the sky. During the operation, care should be taken to protect the Labbe vein and Pulley nerve.
In 2011, South Korea’s Jang et al. reported a case-control study of primary brainstem hemorrhage surgery with the largest number of cases so far. A total of 86 patients underwent stereotactic puncture aspiration, craniotomy for hematoma removal, or simple ventricular drainage. The results showed Surgery can reduce the 30-day mortality rate after the onset of the disease, but cannot improve the neurological prognosis 90 days after the onset of the disease. However, because the study included patients with simple ventricular drainage, the surgical efficacy was affected to a certain extent.
In 2019, Lan et al. retrospectively analyzed the clinical treatment data of a total of 286 patients with severe hypertensive brainstem hemorrhage from 2005 to 2015, of which 46 (16.08%) underwent craniotomy and hematoma removal and 240 (83.92%) underwent medical conservative treatment With an average follow-up of 4.5 years, the results showed that the mortality rate of patients in the craniotomy group and the conservative group was 30.43% (14/46) and 70.42% (169/240), and the survival rate in the vegetative state was 4.35% (2/46) and 2.50% (6/240), severe disability rate is 32.61% (15/46) and 13.75% (33/240), moderate disability rate is 19.57% (9/46) and 7.92% (19/240), good function rate 13.04% (6/46) and 5.83% (14/240); further subgroup analysis showed that patients undergoing surgery within 6 hours of onset have a better neurological prognosis than patients undergoing surgery 6 hours after onset, indicating that the craniotomy has been removed Surgery can significantly reduce the mortality of patients and improve the prognosis of neurological function.
Stereotactic puncture and aspiration is another important surgical method for brainstem hemorrhage. With the development of stereotactic technology, the positioning of hematomas has become more precise, combined with the application of urokinase and other hemolytic enzymes, the hematoma clearance rate has been significantly improved, and the operation is simple, time-consuming, and clinically easy to popularize. It has become the main treatment method for brainstem hemorrhage in some countries. .
Professor Zhang Jianmin’s team used imaging software to reconstruct the hematoma three-dimensionally, make full use of the natural passage formed by the expansion of the hematoma, avoid important nerve conduction bundles and dense areas of nerve nuclei, individually design the surgical path, and pass the assessment of the maximum deflection angle in the path plan. Accurately remove irregular hematomas in all directions, so as to achieve no traction and no electric cauterization during the operation, and minimize iatrogenic damage as much as possible. A total of 47 patients with primary brainstem hemorrhage were enrolled, and all of them underwent stereotactic precision puncture. After aspiration, 7 patients died during the follow-up one month after the operation, with a fatality rate of 14.89%, indicating that stereotactic aspiration can effectively reduce the fatality rate of patients with primary brainstem hemorrhage.
In recent years, it has been reported that 3D printing technology has been applied to primary brainstem hemorrhage. Wang et al. enrolled 6 patients with brainstem hemorrhage, and underwent hematoma puncture and aspiration under the guidance of 3D printing navigation technology.
The results showed that all the puncture catheters were accurately located in the hematoma cavity, the postoperative curative effect was satisfactory, and the symptoms of high fever and respiratory disorders were improved.
3. Problems and prospects
The incidence of primary brainstem hemorrhage is low, and it is difficult to collect large samples of surgical data in a short period of time. Patients with brainstem hemorrhage are in serious condition, and some patients died without prompt treatment due to rapid brainstem failure. Even in hospitalized patients, due to unstable vital signs, they often need respiratory and circulatory support, and the operation risks are high, and there are many surgical complications. The treatment time is long and the cost is expensive, so most of them choose conservative treatment in internal medicine. Therefore, the evaluation of surgical efficacy of primary brainstem hemorrhage still lacks the support of large samples and high-level evidence-based medical evidence.
There are obvious limitations in the researches on primary brainstem hemorrhage surgery at home and abroad: (1) All are retrospective studies, with obvious selection bias. (2) The number of cases is relatively small, the statistical power is poor, and the conclusion is not convincing. (3) The level of surgical operations and postoperative critical care in various medical centers are quite different, and the curative effects are very different. Therefore, there is still a long way to go to transform the experience of surgical treatment of primary brainstem hemorrhage into data and to further upgrade the data to evidence.
There are many factors influencing the prognosis of primary brainstem hemorrhage. Among them, the adverse prognostic factors include early coma, ventilator-assisted ventilation, large hematoma volume (> 5 ml), huge hematoma (affecting the base and cover), etc.; The predictors of a good prognosis include small hematomas and unilateral covered hematomas. The prognostic prediction of primary brainstem hemorrhage after surgical operation is of great significance. Intraoperative neuroelectrophysiological monitoring can predict the degree of recovery of movement and consciousness. For example, the motor evoked potential (MEP) during the process of neuroelectrophysiological monitoring can monitor the motor pathway. Completeness to predict postoperative motor function; somatosensory evoked potential (SEP) has a high reference value in predicting the outcome of disturbance of consciousness.
The incidence of primary brainstem hemorrhage is relatively low, accounting for about 5% of all cerebral hemorrhages, and the efficacy of surgery is related to many factors (including the timing and approach of surgery). Therefore, large-scale case-control studies have been carried out in the clinic.
Research is very difficult; and basic research is the basis for the development of new clinical diagnosis and treatment technologies. By constructing animal models of brainstem hemorrhage, the timing and approach of surgery can be explored. Postoperative imaging (such as superfield MRI to assess brainstem white matter fiber tracts) Injury recovery, changes in brainstem volume, etc.), histopathology (such as brainstem neuron loss), and behavior (such as motor, sensory, cognitive and memory functions) and other multi-angle evaluation of surgical efficacy, to point out the direction of clinical research.
Based on some exploratory retrospective studies, Chinese scholars formulated the first treatment guidelines for primary brainstem hemorrhage and published it in J Neurorestoratol in 2020, which has certain guiding significance for primary doctors. However, the research on surgical treatment should be further in-depth. First, provide high-level evidence-based medical evidence to prove that the surgical operation of hypertensive brainstem hemorrhage is safe and effective; second, learn the research model of rare diseases abroad, and combine Qualified medical centers set up the China Hypertensive Brainstem Hemorrhage Surgical Treatment Cooperative Group to design prospective trials, including a large sample of cases, and comparing them with conservative medical treatments to evaluate the effectiveness and safety of surgery.
In summary, patients with primary brainstem hemorrhage are younger than those with cerebral hemorrhage in other parts, and the peak age of onset is 40-60 years old.
Regardless of conservative medical treatment or surgical treatment, the prognosis of neurological function is poor. Therefore, prevention is particularly important for such diseases that are harmful and there is no definite treatment method. Active screening of risk factors for brainstem hemorrhage, early diagnosis and control of hypertension, diabetes, etc. to prevent brainstem hemorrhage, has important clinical significance.
(source:internet, reference only)
Disclaimer of medicaltrend.org



