Pancreatic cancer Research: The Latest global burden of disease data
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
Pancreatic cancer Research: The Latest global burden of disease data
Pancreatic cancer Research: The Latest global burden of disease data. Learn about the latest global burden of disease data in one article!
From 1990 to 2017, the number of deaths, incidences and DALYs caused by pancreatic cancer more than doubled globally.
Although pancreatic cancer may not be well-known to many people, it is a common and highly malignant tumor of the digestive system. This kind of cancer has a dangerous onset, hidden symptoms, strong invasiveness, short course of disease, rapid progression, and high mortality. The median survival time is only about 6 months. About 3/4 of the patients die within 1 year after diagnosis, and 5 years. The survival rate is less than 5%. Therefore, it is also called the “king of cancer”. In recent years, many celebrities including former Vice Premier of the State Council Huang Ju, world-renowned tenor Pavarotti, and famous Hong Kong artist Shen Dianxia have died of pancreatic cancer, which makes people sigh.
Worldwide, the incidence and mortality of pancreatic cancer are increasing. Assessing the burden of pancreatic cancer and its global, regional, and national patterns are essential to formulate and better allocate medical resources to control pancreatic cancer risk factors, implement early detection, and provide faster and more effective treatment.
Recently, researchers from the Institute of Health Measurement and Evaluation of the University of Washington in the United States used the data in the Global Burden of Disease (GBD) 2017 research report to examine the incidence, mortality and injury of pancreatic cancer in 195 countries and regions from 1990 to 2017. Disability adjusted life years (DALYs), and estimated the proportion of deaths caused by pancreatic cancer risk factors (smoking, high fasting blood glucose, and high body mass index). Related research results were published in “The Lancet Gastroenterology & Hepatology” (impact factor 12.856).

Pancreatic cancer is one of the cancers with the worst prognosis. The 5-year overall survival rate is only about 5%, and there is not much difference between high-, middle- and low-income countries. However, the incidence and mortality of pancreatic cancer vary greatly among countries in the world. In high-income countries, this cancer has the highest incidence and mortality, so it has the nickname “rich cancer”. Although medical staff have not yet fully clarified the pathogenesis of pancreatic cancer, they have identified some risk factors such as smoking, obesity and diabetes.
Main research results
▍In 2017, there were 448,000 new cases of pancreatic cancer worldwide and 441,000 deaths
In 1990, the global incidence of pancreatic cancer was 195,000 cases, which increased to 448,000 cases in 2017, an increase of 1.3 times in 28 years. In 2017, there were 232,000 males in the total number of cases, accounting for 51.9%; in 1990, the proportion of males was 52.1%.
In 1990, the global age-standardized incidence rate of pancreatic cancer was 5.0 cases per 100,000 person-years, and by 2017 it had risen to 5.7 cases per 100,000 person-years. It caused 9.1 million DALYs in 2017, an increase of 1.1 times from the 4.4 million in 1990.
In 2017, pancreatic cancer caused 441,000 deaths globally, of which 226,000 were men, accounting for 51.3%. In 1990, pancreatic cancer caused 196,000 deaths worldwide, an increase of 1.3 times in 28 years.
The age-standardized death rate rose from 5.1 cases per 100,000 person-years in 1990 to 5.6 cases per 100,000 person-years in 2017, an increase of 10.4%. For men, the age-standardized incidence rate of this cancer has increased from 5.7 cases per 100,000 person-years in 1990 to 6.3 cases in 2017; for women, the age-standardized incidence rate of this cancer has increased from per 100,000 in 1990. There were 4.5 cases a year for 100,000 people, which increased to 5.0 cases in 2017.
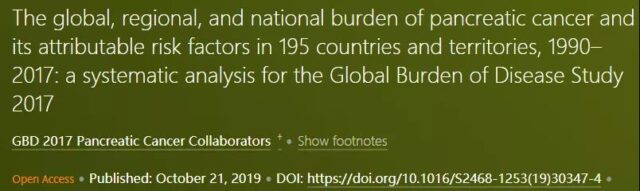
From 1990 to 2017, the age-standardized incidence and death rates of pancreatic cancer have been on the rise in the 21 regions counted by GBD, as shown in Figure 1.
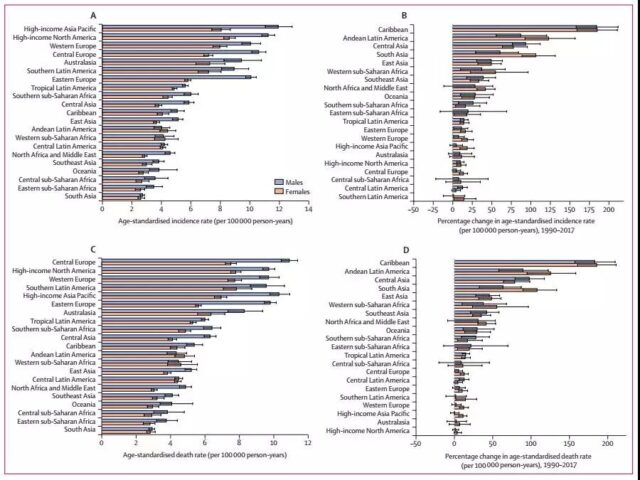
Figure 1: Trends in age-standardized incidence and mortality of pancreatic cancer in major regions of the world from 1990 to 2017
In 2017, the higher-income regions (North America, Western Europe, Central Europe, and Asia Pacific) had the highest age-standardized morbidity and mortality rates. In contrast, South Asia, East Africa, Central Africa, and Sub-Saharan regions have the lowest age-standardized morbidity and mortality. On the whole, from 1990 to 2017, the age-standardized incidence and mortality rates of men in most regions were higher than those of women.
With age, the incidence and mortality of pancreatic cancer will increase; this trend is similar between men and women; as shown in Figure 2. Men between 65 and 69 years old, and women between 75 and 79 years old, the number of morbidities and deaths in these two age groups reached a peak. The age pattern of DALYs showed a similar trend with the total number of morbidities and deaths, but declined among people over 80 years of age.
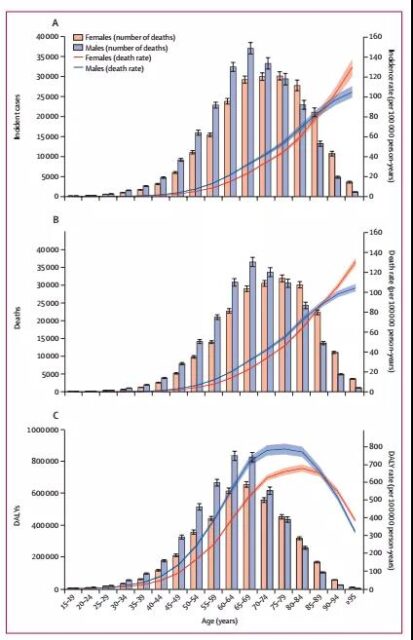
Figure 2: Pancreatic cancer incidence, mortality and DALYs trends with age
▍In 2017, there were 83,562 new cases of pancreatic cancer in China and 85,101 deaths
The number of pancreatic cancer deaths in mainland China in 1990 was 25,322, and in 2017 was 85,101, an increase of 2.36 times in 28 years; the number of new cases in 1990 was 25,250, and the number of new cases in 2017 was 83,562. This has increased by 2.31 times in 28 years. The DALYs in 1990 were 674,107 years, and the DALYs in 2017 were 1,890,853 years, an increase of 1.8 times in 28 years.
▍Three risk factors for death: smoking, high fasting blood sugar and high body mass index (BMI)
Figure 3: Main attribution scores for pancreatic cancer
Smoking:
In 2017, 93,600 pancreatic cancer deaths were attributed to smoking (21.1%), of which 25.9% were males and 16.1% were females; as shown in Figure 3A. In 1990, pancreatic cancer deaths attributable to smoking accounted for 26.6%, a decline of 5.5% in 28 years.
In terms of different regions, in 2017, the proportion of age-standardized deaths from pancreatic cancer attributed to smoking in men was highest in Eastern Europe (35.7%) and East Asia (31.3%), while women were in North America (29.3%) and southern Latin America (27.6). %)Highest. Correspondingly, men and women in the west of the Sahara Desert had the lowest standardized death rates from pancreatic cancer attributable to smoking, at 8.0% and 2.1%, respectively.
In different age groups, the proportion of age-standardized deaths attributed to smoking is higher than 25% among men between 55 and 84 years old, and the proportion of women in the same age group is higher than 16%; as shown in Figure 3B .
High fasting blood sugar:
In 2017, 8.9% of pancreatic cancer deaths were attributed to high fasting blood glucose, with 9.3% of men and 8.6% of women. In 1990, pancreatic cancer deaths attributable to smoking accounted for 7.7%, an increase of 1.2% in 28 years.
In 2017, men and women in Oceania had the highest age-standardized death rates from pancreatic cancer attributable to high fasting blood glucose, at 16.0% and 17.3%, respectively. East Asian men had the lowest age-standardized death rate from pancreatic cancer (5.8%) attributable to high fasting blood glucose, and the lowest rate (6.1%) in Latin American women in the tropics.
The age-standardized death rate attributable to high fasting blood glucose is the highest among men and women aged 85 to 89 years.
High BMI:
Similarly, in 2017, 6.2% of pancreatic cancer deaths were attributed to high BMI, with 5.0% of men and 7.4% of women. In 1990, pancreatic cancer deaths attributable to high BMI accounted for 5.0%, an increase of 1.2% in 28 years.
The age-standardized death rate of pancreatic cancer attributable to high BMI is the highest in North America, with 8.6% and 11.7% of men and women, respectively. The proportion of age-standardized deaths attributed to pancreatic cancer with high BMI in men in the east of the Sahara is the lowest (2.1%), and women in the Asia-Pacific region have the lowest (3.5%).
Although the proportion of age-standardized deaths attributed to high BMI is higher among men and women aged 45 to 79, the differences among age groups are not large.
▍The higher the social demographic index (SDI), the higher the morbidity and mortality
From 1990 to 2017, with the increase in SDI, the age-standardized incidence and mortality of pancreatic cancer also increased, as shown in Figure 4. That is to say, in countries with low SDI, the incidence and mortality of this cancer is low, while in countries with relatively high SDI, the incidence and mortality of this cancer is high; as shown in Figure 5. This fully confirms from the macro level that pancreatic cancer is indeed a rich cancer.
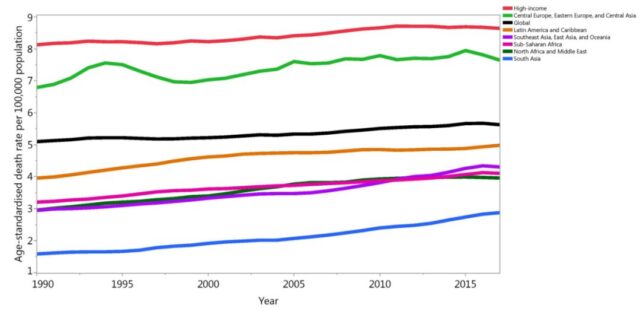
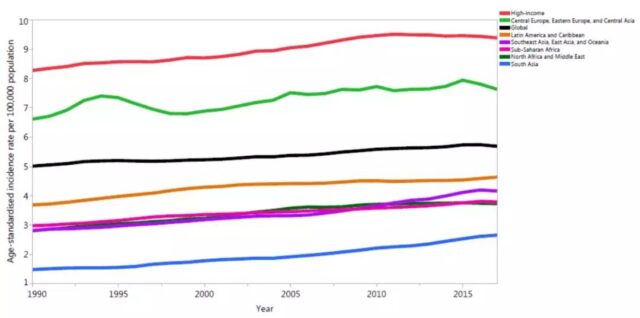
Figure 4: Trends in age-standardized incidence and mortality of pancreatic cancer from 1990 to 2017
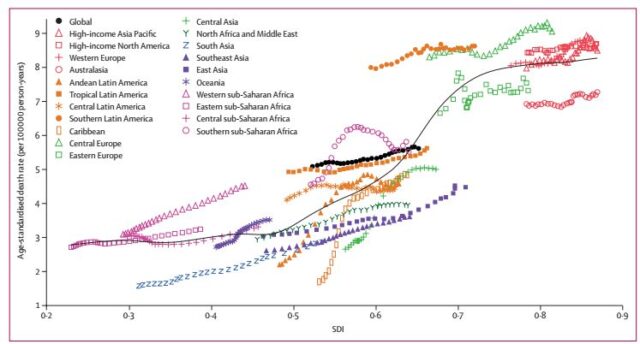
Figure 5: Relationship between age-standardized mortality of pancreatic cancer and SDI
Figure 6 shows the relationship between age-standardized mortality of pancreatic cancer and SDI in different countries and regions in 2017. In this picture, China is in the middle right position, that is, SDI is higher than the global average, and the death rate is lower than the global average.
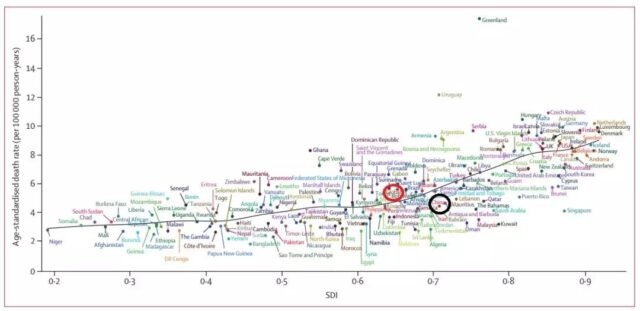
Figure 6: The relationship between age-standardized mortality of pancreatic cancer and SDI in different countries and regions
The task of prevention and control has a long way to go
From 1990 to 2017, the number of deaths, incidences and DALYs caused by pancreatic cancer more than doubled globally. With the increasing trend of population aging, the incidence of pancreatic cancer may continue to rise. Prevention work should focus on the prevention and control of changeable risk factors. Therefore, it is necessary to formulate early screening programs and develop more effective pancreatic cancer treatment strategies.
Five warning signs of pancreatic cancer
Dr. Andrew Hendifar, director of the Pancreatic Oncology Department of the Sidders-Sinai Medical Center in Los Angeles, analyzed that part of the reason for the low survival rate of pancreatic cancer is that it is difficult to identify pancreatic cancer early.
The pancreas is located deep in the abdomen and is a long, flat organ. Although the symptoms of pancreas problems are mild, experienced physicians can still identify some clues.
When you have the following symptoms in your daily life, you must beware of pancreatic cancer and get screened and tested as soon as possible.
1. Stool looks weird
If you notice lightening and floating of stool, this is a sign of poor nutrient absorption. In addition to breaking down fat, the pancreas also helps the body absorb fat-soluble vitamins. When pancreatic disease disrupts the organ’s ability to normally produce enzymes, it can cause stools to look gray and not so dense. You may also notice that the stool is a little greasy, and there is an oily film on the surface of the toilet flushing water. This is the fat in the diet that the body cannot break down.
2. Abdominal pain
Abdominal pain is one of the most common symptoms of pancreatic cancer and acute pancreatitis. If the pain starts in the center of the abdomen and then radiates to the back and waist, this may be a sign of pancreatic cancer.
3. Diabetes
Hormones secreted by the pancreas help the body control insulin production and blood sugar levels. When the pancreas is in danger, patients can easily get type 2 diabetes. If you are diagnosed with type 2 diabetes, you also need to have a careful examination of pancreatic function.
4. Nausea after eating greasy food
If you have nausea and vomiting after eating greasy foods (such as avocados, pizza, and nuts), you need to pay special attention. This is also because the enzymes produced by the pancreas help the digestive system to break down fat. Diseases that disrupt the function of the pancreas can also hinder the body’s ability to digest fat, leading to nausea.
5. Weight loss
If the weight loss is accompanied by the aforementioned abdominal radiation pain, then this weight loss may be caused by pancreatic cancer or other digestive system diseases.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



