How to build a child’s immune barrier against COVID-19 Omicron?
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
- Mifepristone: A Safe and Effective Abortion Option Amidst Controversy
- Asbestos Detected in Buildings Damaged in Ukraine: Analyzed by Japanese Company
How to build a child’s immune barrier against COVID-19 Omicron?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
How to build a child’s immune barrier against COVID-19 Omicron?
Since the outbreak of the Omicron variant in November 2021, it has replaced the Delta variant as the dominant global epidemic in just a few months.
People infected with Omicron variant strains have the characteristics of shorter hospital stay, less respiratory support and less severe disease [1~2] .
Therefore, many European countries have lifted the control of the COVID-19 epidemic, such as Denmark, Norway, Sweden and the United Kingdom [ 1-2]. 3] .
Due to the huge differences in anatomy, physiology and immunity between children and adults, it is necessary to interpret the impact of Omicron variants on children’s health and the corresponding immune strategies.
Effects of Omicron Variant Prevalence in Children
1. Omicron mutants are susceptible to children for the following reasons:
(1) The anatomical and pathophysiological characteristics of children’s own respiratory tract [4] are one of the reasons why they are more susceptible to Omicron and more harmful:
- Upper respiratory tract: The nasal cavity of children is shorter than that of adults, the posterior nasal passage is narrow, the mucous membrane is soft, the blood vessels are rich, and it is easy to be infected; when inflamed, the posterior nasal cavity is easily blocked, which makes breathing and sucking difficult;
- Lower respiratory tract: Children’s trachea and bronchi are narrower than adults, with soft cartilage, lack of elastic tissue, weak support, and pressure during exhalation, which affects gas exchange;
- Thoracic and respiratory muscles: Children’s intercostal muscles are underdeveloped and cannot increase thoracic expansion during inhalation. They mainly rely on the diaphragm for breathing, and the diaphragm is transverse and high, which is more likely to cause respiratory failure when infected.
(2) The immune system of children is not fully developed, whether it is innate immunity or adaptive immunity, which leads to the susceptibility of children to infectious diseases.
(3) Due to the aggregated life of children, it is more conducive to the spread of Omicron mutants.
(4) The replication ability of Omicron mutant strains in human nasal mucosa cells is significantly increased, which is also one of the reasons why Omicron mutant strains are susceptible to children [5] .
(5) More importantly, due to the particularity of this group of children, the approval of the COVID-19 vaccine for children significantly lags behind the adult group, resulting in a low overall vaccination rate of the COVID-19 vaccine for children and the inability to establish an effective vaccine against the COVID-19 virus. immune barrier.
2. Omicron variant strains lead to a significant increase in the hospitalization rate of children [6] .
Although the pathogenic symptoms of the Omicron variant are mostly mild, it is highly contagious (R0=8), resulting in a significant increase in the total number of cases, which in turn leads to a significant increase in hospitalization rates.
A study by the Centers for Disease Control and Prevention (CDC) showed that during the epidemic of Omicron variants, the weekly hospitalization rate of children was 7.1 cases/100,000; during the epidemic of Delta variants, the weekly hospitalization rate of children was 1.8 cases/100,000. 100,000, the hospitalization rate caused by Omicron is about 4 times that of the Delta variant.
And the report also found that during the epidemic of Omicron variant strains, the hospitalization rate increased most obviously in 0~4 years old (not vaccinated) , and the weekly hospitalization rate during the epidemic period of Delta variant strains increased from 2.9 cases/100,000 to 15.6 Cases/100,000. (see picture 1)
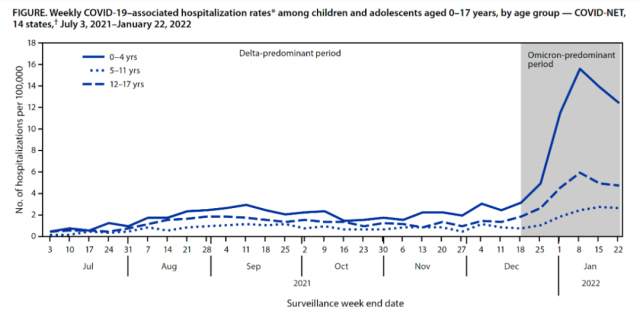
Figure 1. Comparison of Weekly Hospitalization Rates in the Omicron Variant Background and the Delta Variant Background
3. Vaccination can significantly reduce the hospitalization rate caused by Omicron in children [6] .
The research report of the CDC in the United States shows that:
1) During the epidemic of Omicron variant strains, the hospitalization rate of children aged 0-4 years who have not been vaccinated against the COVID-19 vaccine is significantly higher than that of the 5-11-year-old and 12-17-year-old groups who have been partially vaccinated (see Figure 1);
2) The study report shows that during the epidemic of the Delta variant, 90.1% of the cases in the hospitalized adolescent population were not vaccinated; during the epidemic of the Omicron variant, up to 77.8% of the cases in the hospitalized adolescent population were not vaccinated against the COVID-19; in addition, The proportion of unvaccinated adolescents admitted to the ICU (30.3%) was significantly higher than that of vaccinated adolescents (15.5%).
Vaccination is the main cause of milder disease in patients with Omicron variants
The US CDC released a report from a hospital in California and found that by comparing the clinical characteristics of patients infected with the Omicron variant strain and those infected with the Delta variant strain, it was found that the hospitalization rate, ICU admission rate and mechanical ventilation rate of the former were significantly lower than those of the latter.
From the data, it seems that the Omicron variant is naturally less pathogenic than the Delta variant.
However, a stratified analysis of the data by “vaccinated or not” found that in the unvaccinated population, there was no statistical difference in the hospitalization rate, ICU admission rate, mechanical ventilation rate and case fatality rate caused by the Omicron variant and the Delta variant. In the fully vaccinated population, the hospitalization rate, ICU admission rate, mechanical ventilation rate and mortality rate caused by Omicron were significantly lower than those of the Delta variant [7] .
Current status of childhood COVID-19 vaccination and strategies for establishing immune barriers
1. Status of children’s COVID-19 vaccination:
1) The vaccination rate of children’s COVID-19 vaccine is still low. As of January 18, 2022, the vaccination rate of children aged 5 to 11 years old in the United States receiving at least one dose of COVID-19 vaccine is 25% (see Figure 2), and there are differences between different states in the United States.
There is a huge difference in the vaccination rate of this age group. What is particularly serious is that children aged 5 to 11 have a vaccination peak in the early stage of BNT162b2 approval, and the vaccination rate of the COVID-19 every 7 days has shown a significant downward trend [8] (see Figure3);
2) The vaccination rate of children aged 3-11 in China has reached 50% by November 16, 2021 [9] ;
3) Generally speaking, the vaccination rate of children with COVID-19 in the world is still low, especially at present, there are still some young children who are not vaccinated against COVID-19.
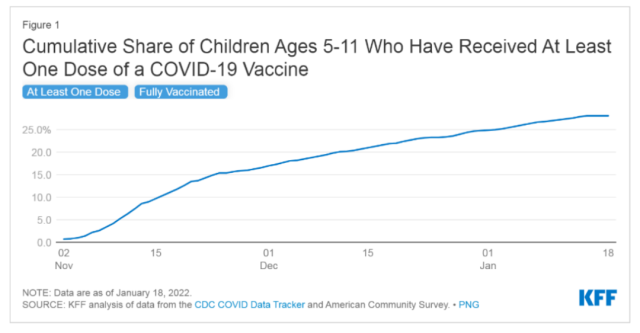 Figure 2. Involved coverage of at least one dose of COVID-19 vaccine among children aged 5-11 in the United States
Figure 2. Involved coverage of at least one dose of COVID-19 vaccine among children aged 5-11 in the United States
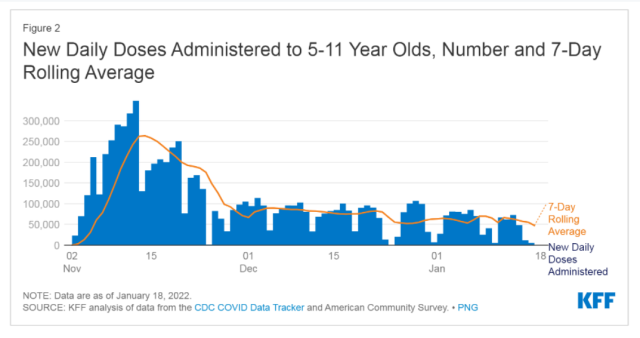 Figure 3. Trends in the 7-day vaccination rate of the COVID-19 vaccine for children aged 5 to 11 in the United States
Figure 3. Trends in the 7-day vaccination rate of the COVID-19 vaccine for children aged 5 to 11 in the United States
(2) Strategies for the construction of children’s immune barrier:
1) The overall vaccination rate of children is currently low, and the vaccination rate of children should be increased as much as possible to build a basic defense line for children to prevent and control the COVID-19 epidemic;
2) The Lancet magazine A phase IV randomized trial from Brazil has been published online exploring different homologous or heterologous vaccine booster strategies.
The study found that following completion of two doses of inactivated vaccine using different booster strategies, IgG antibody concentrations were significantly increased in all cohorts from baseline to day 28 after booster vaccination: Ad26.COV2.S increased 77-fold (95 %CI: 67-88), 152-fold (95%CI: 134-173) for BNT162b2, 90-fold for ChAdOx1 nCoV-19(95%CI: 77-104), 12-fold for CoronaVac (95%CI: 11-14) [10] .
At present, a large number of studies have shown that regardless of the technical route of the vaccine, the neutralizing antibodies of the new coronavirus in the vaccinated body show a certain degree of decline with the passage of time.
Among them, the mRNA vaccine BNT162b2 can still maintain a high neutralization level after the completion of the vaccination. antibody levels.
In addition, studies have shown that sequential vaccination by heterologous, such as inactivated vaccine sequential BNT162b2, can achieve better immunogenicity and better response to Omicron mutants.
At present, there is little evidence related to the strengthening or sequence of children’s COVID-19 vaccine. In order to better build the immune barrier of children’s COVID-19 epidemic, it is necessary to carry out children’s sequential or strengthen related research to further enrich the children’s COVID-19 epidemic prevention strategy.
Summary
There are huge differences between children and adults in anatomy, physiology and immunity, and the high replication ability of the nasal mucosa of Omicron virus makes children susceptible to Omicron variant strains and is more harmful than adults.
The Omicron variant showed lower disease severity than other variants, and vaccination was one of the main reasons. However, the current global childhood vaccination rate is generally low.
It is imperative to take measures to increase the COVID-19 vaccination rate of children, and if necessary, boost or sequential vaccination should be carried out to build an immune barrier for children against Omicron variants.
References:
[1] Christensen, Paul A et al. Signals of Significantly Increased Vaccine Breakthrough, Decreased Hospitalization Rates, and Less Severe Disease in Patients with Coronavirus Disease 2019 Caused by the Omicron Variant of Severe Acute Respiratory Syndrome Coronavirus 2 in Houston, Texas.” The American journal of pathology, S0002-9440(22)00044-X. 3 Feb. 2022, doi:10.1016/j.ajpath.2022.01.007
[2] Maslo, Caroline et al. “Characteristics and Outcomes of Hospitalized Patients in South Africa During the COVID-19 Omicron Wave Compared With Previous Waves.” JAMA vol. 327,6 (2022): 583-584. doi:10.1001/jama.2021.24868
[3] Foreign media: Many European countries ease entry bans | Epidemic | WHO | COVID-19 Pneumonia_Sina Military_Sina.com (internet.com.cn)
[4] Pediatrics/Paediatric Respiratory System Anatomy, Physiological Characteristics and Their Clinical Significance – A+ Medical Encyclopedia (a-hospital.com)
[5]https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1043652/S1454_Omicron_report_20.12_Imperial.pdf
[6]https://www.cdc.gov/mmwr/volumes/71/wr/mm7107e4.htm?s_cid=mm7107e4_w#F1_down
[7]https://www.cdc.gov/mmwr/volumes/71/wr/mm7106e2.htm?s_cid=mm7106e2_w
[8] https://www.kff.org/coronavirus-covid-19/issue-brief/update-on-covid-19-vaccination-of-5-11-year-olds-in-the-u-s/
[9] China’s 3- to 11-year-old vaccine coverage reaches 50%|Children’s vaccine|Coverage|COVID-19 Pneumonia_Sina Parenting_Sina.com (internet.com.cn)
[10] Costa Clemens, S.A., et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): a phase 4, non-inferiority, single blind, randomised study. The Lancet 399, 521-529 (2022).
How to build a child’s immune barrier against COVID-19 Omicron?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



