NEJM: No need for radiotherapy after breast-conserving breast cancer surgery!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
NEJM: No need for radiotherapy after breast-conserving breast cancer surgery!
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
NEJM: No need for radiotherapy after breast-conserving breast cancer surgery!
In low-risk, older, hormone-receptor (HR)-positive patients with small tumors, whether radiotherapy can be skipped after breast-conserving surgery remains controversial, and the level 1 evidence available to guide treatment decisions is limited.
Although guidelines support the omission of radiotherapy in women ≥70 years of age with T1 or partially T2, estrogen receptor (ER)-positive breast cancer, many patients still receive radiotherapy.
Recently, a research team led by Ian H. Kunkler from the University of Edinburgh published an article titled “Breast-Conserving Surgery with or without Irradiation in Early Breast Cancer” in The New England Journal of Medicine ( NEJM, IF: 176.08 ), reporting Based on the 10-year results of the PRIME II trial , the 10-year survival outcomes of breast cancer patients aged ≥65 years, positive HR, negative lymph nodes, and tumors ≤3 cm were compared with those without radiotherapy after breast-conserving surgery. high-level evidence.
 Screenshot of the homepage of the paper Source: NEJM
Screenshot of the homepage of the paper Source: NEJM
Research Background and Design
The study (PRIME II trial) was a phase III randomized clinical trial designed by the Scottish Cancer Trials Breast Cancer Group (SCTBG) and conducted at 76 centers in the UK, Greece, Australia and Serbia.
Enrolled patients meet the following conditions: women aged 65 or over, staged T1 or T2 primary breast cancer (maximum tumor diameter ≤ 3cm), have undergone breast-conserving surgery, negative axillary lymph nodes, ER positive and/or progesterone Receptor (PR) positive, margin negative (≥1mm).
From April 16, 2003 to December 22, 2009, a total of 1326 patients were enrolled and randomized in a 1:1 ratio: 658 received postoperative whole-breast radiotherapy and 668 did not receive postoperative radiotherapy.
Patients in the radiotherapy group received radiotherapy of 40-50Gy divided into 20-25 fractions, divided into doses of 2.00 to 2.66Gy/time, and the radiotherapy time was 3 to 5 weeks.
Electron wires (10-15Gy) or iridium implants (20Gy) were given if necessary. ) for tumor bed push. Both groups received tamoxifen (20 mg/day) as adjuvant endocrine therapy for 5 years.
The primary endpoint of the study was local recurrence of breast cancer. Secondary endpoints included regional recurrence, contralateral breast cancer, distant recurrence, disease-free survival, and overall survival.
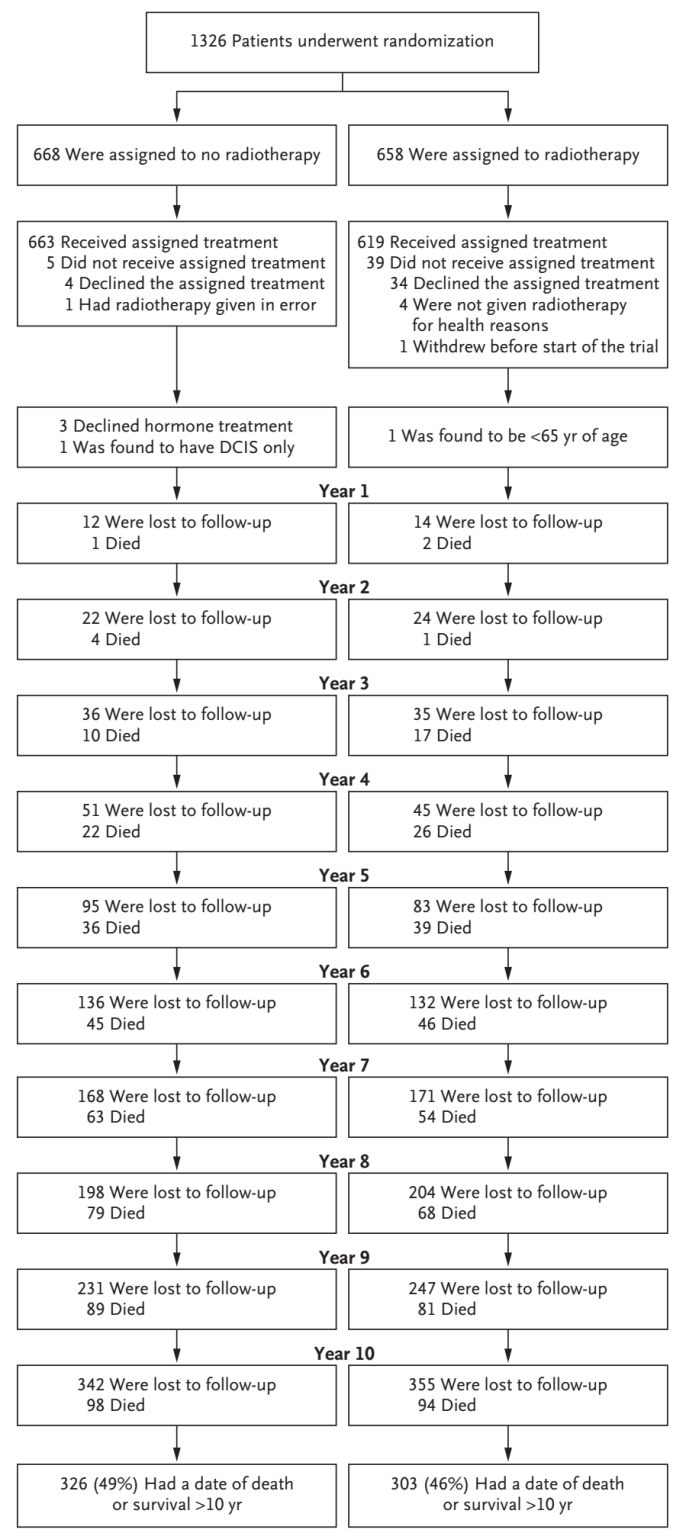 Research flow diagram Source: NEJM
Research flow diagram Source: NEJM
Research result
At a median follow-up of 9.1 years, a total of 56 patients had local breast recurrence (51 in the non-irradiated group and 5 in the irradiated group), and 31 patients died of breast cancer (16 in the non-irradiated group and 15 in the irradiated group).
Most deaths were not caused by breast cancer, and 25% (59/231) of deaths were caused by cancers other than breast cancer .
The 10-year local recurrence rate was higher in the no-irradiation group (9.5% vs 0.9%; 95% confidence interval [CI]: 6.8-12.3 vs 95%CI: 0.1-1.7) compared with the radiotherapy group, and the hazard ratio for local recurrence was 10.4 (95%CI: 4.1-26.1; P<0.001).
The 10-year cumulative incidence of distant metastases as the first event was lower in the no-radiation group, 1.6% (95% CI, 0.4-2.8), compared with 3.0% (95% CI, 1.4-4.5) in the radiotherapy group.
There were no significant differences in regional recurrence, contralateral breast or new cancer incidence, or new cancer-free survival at 10 years.
Compared with the radiotherapy group, the 10-year disease-free survival rate was lower in the non-radiation group, (68.9% vs 76.3%; 95%CI: 64.7-73.0 vs 95%CI: 72.5-80.2), and the 10-year breast cancer-specific survival rate The rates were comparable (97.4% vs 97.9%; 95%CI: 96.0-98.8 vs 95%CI: 96.5-99.2). The 10-year overall survival rates were comparable (80.8% vs 80.7%; 95% CI: 77.2-84.3 vs 95% CI: 76.9-84.3).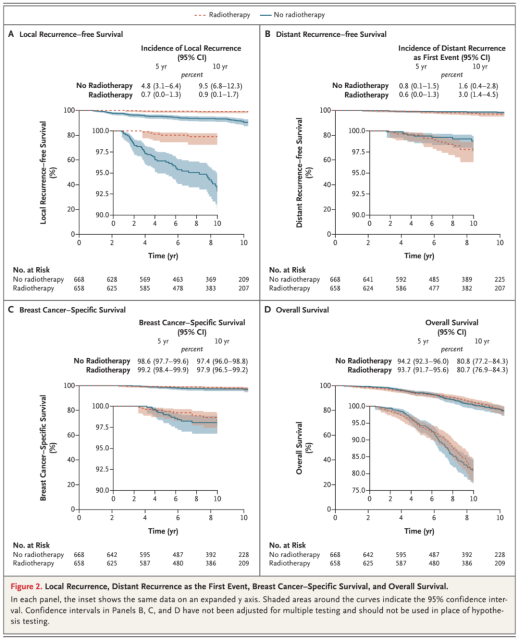 A Local recurrence-free rate, B Distant recurrence-free survival rate, C Breast cancer-related survival rate, D Overall survival rate Data source: NEJM
A Local recurrence-free rate, B Distant recurrence-free survival rate, C Breast cancer-related survival rate, D Overall survival rate Data source: NEJM
Subgroup analyzes of local recurrence according to ER status showed that patients with ER-high breast cancer had a lower rate of local recurrence than the overall trial population .
In breast cancer patients with high ER expression, the 10-year local recurrence rate was 8.6% (95% CI, 5.7 to 11.4) in the non-radiation group and 1.0% (95% CI: 0.1 to 1.9) in the radiotherapy group (HR=8.23; 95% CI: 3.24-20.85).
In breast cancer patients with low ER expression, the 10-year local recurrence rate in the non-radiation group was 19.1% (95%CI: 8.2-29.9), and no local recurrence was observed in the radiotherapy group, but the sample was very small (53 cases).
Compared with breast cancer patients with high ER expression in the radiotherapy group, the 10-year risk of local recurrence in breast cancer patients with low ER expression in the non-radiation group was 23.93 times higher (95%CI: 8.43-67.93).
Previous findings have shown that adherence below 80% is associated with a significantly reduced benefit of adjuvant endocrine therapy.
To further confirm this conclusion, the researchers collected data on the duration of adjuvant endocrine therapy, and time-dependent analysis showed that in the non-radiotherapy group, compared with patients who continued to receive endocrine therapy, patients who no longer received endocrine therapy had a higher rate of local recurrence The risk increased 4.66 times (95%CI: 1.77-12.25), which was consistent with previous research results.
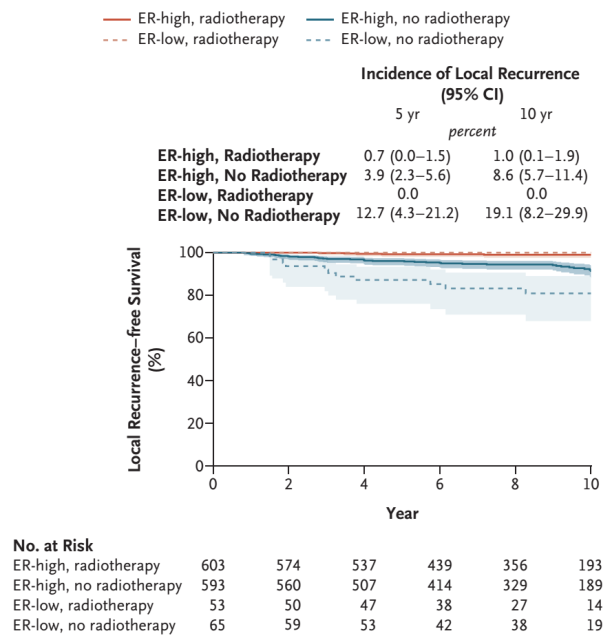 Local recurrence-free survival subgroup analysis Source: NEJM
Local recurrence-free survival subgroup analysis Source: NEJM
Discussion and expansion
In this study, patients who received whole-breast radiation had a significantly lower rate of local recurrence at 10 years after breast-conserving surgery than patients who did not receive radiation, but the absolute difference in local recurrence at 10 years between the two groups was small (8.6 percentage points) .
Despite this difference, radiotherapy had no substantial effect on the incidence of regional or distant metastases or on breast cancer-specific or overall survival.
The incidence of local recurrence at 10 years after breast-conserving surgery and radiotherapy was consistent with the results of the CALGB 9343 trial.
The EUSOMA guidelines recommend that low-risk breast cancer patients over 70 years of age who receive adjuvant endocrine therapy do not need radiotherapy, similar to the recommendations of the UK National Institute for Health and Care Excellence (NICE) and NCCN guidelines, the latter two A guideline allows omission of radiotherapy for women ≥65 years or ≥70 years of age with stage 1 ER-positive breast cancer after breast-conserving surgery.
Results from the PRIME II trial provided additional data showing that although omitting radiotherapy increased the cumulative incidence of local recurrence, it did not have a similar effect on distant disease-free survival or overall survival.
The balance of risks and benefits of radiotherapy compared with adjuvant endocrine therapy will affect the applicability of the findings in clinical practice. Radiation therapy is associated with complications such as cardiac events and secondary cancers, but in this study, the investigators did not collect data on radiation toxicity.
An analysis of treatment-related complications in the previous PRIME I trial showed no difference in overall quality of life between patients who received radiation and those who did not.
For low-risk, ER-positive older breast cancer patients, the risk-benefit ratio of radiotherapy and endocrine therapy becomes more nuanced, and investigators consider adjuvant endocrine therapy without radiotherapy a major competitor to whole-breast radiotherapy.
Further breast-conserving therapy and radiation are options for patients who do not receive radiation and subsequently experience local recurrence, so recurrence does not necessarily mean breast loss.
In this trial, few patients had grade 3 tumors (36 patients) or lymphovascular invasion (39 patients), so it is unclear whether radiation therapy could be avoided in these patients.
In selecting appropriate patients for a trial, clinicians are cautious about including patients with grade 3 tumors or lymphovascular invasion because breast cancer patients with grade 3 histologic features or lymphovascular invasion have a doubled risk of local recurrence, but these features Associations with risk factors in older patients are unclear.
The option to restrict grade 1 and 2 tumors from radiotherapy is also in line with current European guidelines, and grade 3 tumors were not included in the CALGB 9343 trial.
The findings are consistent with earlier observations that breast cancer patients with high ER expression had a lower cumulative incidence of local recurrence over 10 years than those with low ER expression.
Patients with less than 80% adherence to endocrine therapy were considered to have a poorer prognosis, but the investigators did not collect data on adherence.
Instead, using reported endocrine therapy termination as a surrogate measure, they found that in the no-irradiation group, patients who did not adhere to endocrine therapy had a four-fold higher risk of local recurrence than those who continued endocrine therapy.
In conclusion, the PRIME II trial provides strong evidence that endocrine therapy for 5 years after breast-conserving surgery is safe for women aged ≥65 years with grade 1 or 2 breast cancer patients with high ER expression.
xemption from radiotherapy. Compared with whole breast radiotherapy patients, patients without radiotherapy had a higher rate of local recurrence, but there were no significant differences in regional recurrence, first distant recurrence, disease-free survival, breast cancer-specific survival, and overall survival.
Summary
Alice Y. Ho , Duke University School of Medicine and Jennifer R. Bellon, Dana-Farber Cancer Institute/Brigham and Women’s Hospital, Harvard Medical School, published a concurrent review in NEJM on the 10-year results of the PRIME II trial.
They point out that the study offers a countermeasure to the long-standing problem of overtreatment of older women with low-risk breast cancer, but also has some shortcomings.
First, although the PRIME II trial confirmed that omitting radiotherapy did not affect distant recurrence or overall survival in these patients, less than 5% of the patients in the study had tumor grade 3 or lymphovascular invasion, which limited the results of the trial. Suitability for patients with high-risk features.
Second, the positive level of ER can predict the risk of local recurrence in patients without radiotherapy, and the risk of recurrence is higher in patients with low expression of ER.
The vast majority of patients in the study had high expression of ER, which limits the applicability of the data to patients with moderate ER positivity. In addition, non-adherence to endocrine therapy resulted in a higher rate of local recurrence in the non-irradiated group.
Third , if these trials can show that biomarkers can be used to accurately select breast cancer patients with low risk of local recurrence, the impact of current multiple studies to adjust treatment according to the biological characteristics of tumors will be truly profound, promoting the improvement of treatment in patients who are already low risk. Further risk stratification.
At the end of the article, they further concluded that any doubts that radiotherapy cannot be omitted for women over 65 years of age, ER-positive, early-stage breast cancer can be dispelled. Given the long natural history of ER-positive breast cancer, the 10-year follow-up results in the trial are reassuring.
These results do not diminish the value of radiotherapy in terms of local control, which is a compelling endpoint in itself, especially now that radiotherapy can be delivered in less burdensome ways (such as omitting radiotherapy, shortening radiotherapy, and shrinking the target volume). It is critical to adopt an individualized treatment plan that aligns with the patient’s goals and values.
Taken together, these data will help patients understand these complex options, thereby enabling them to make informed and prudent decisions about their breast cancer treatment.
references:
1. Kunkler IH, Williams LJ, Jack WJL, Cameron DA, Dixon JM. Breast-Conserving Surgery with or without Irradiation in Early Breast Cancer. N Engl J Med. 2023;388(7):585-594. doi:10.1056/ NEJMoa2207586
2. Ho AY, Bellon JR. Overcoming Resistance – Omission of Radiotherapy for Low-Risk Breast Cancer. N Engl J Med. 2023;388(7):652-653. doi:10.1056/NEJMe2216133
3. Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013;31 (19):2382-2387. doi:10.1200/JCO.2012.45.2615
NEJM: No need for radiotherapy after breast-conserving breast cancer surgery!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



